Pharmachologic effect. Physicochemical and chemical mechanisms of action of medicinal substances. Individualized drug therapy strategy
First generation H 1 -histamine receptor blocker. The effect on the central nervous system is due to the blockade of H 3 -histamine receptors in the brain and inhibition of the central cholinergic structures. Relieves spasm of smooth muscles (direct action), reduces capillary permeability, prevents and weakens allergic reactions, has local anesthetic, antiemetic, sedative effects, moderately blocks cholinergic receptors of autonomic ganglia, has a hypnotic effect.
Indications - anaphylactic and anaphylactoid reactions (in complex therapy); - Quincke's edema;
Serum sickness; - other acute allergic conditions (in complex therapy and in cases where the use of the tablet form is impossible).
Side effects
From the side nervous system: drowsiness, weakness, decreased speed of psychomotor reaction, impaired coordination of movements, dizziness, tremor, irritability, euphoria, agitation (especially in children), insomnia.
From the side respiratory system: dryness of the mucous membrane of the mouth, nose, bronchi (increased viscosity of sputum).
From the side of hematopoiesis: hemolytic anemia, thrombocytopenia, agranulocytosis.
From the side of cardio-vascular system: decrease in blood pressure, tachycardia, extrasystole.
From the urinary system: urination disorder.
Allergic reactions: urticaria, photosensitivity, skin rash, itching.
Loratadin (claritin)
pharmachologic effect
Antiallergic drug, selective blocker of peripheral histamine H 1 receptors. Loratadine is a tricyclic compound with a pronounced antihistamine effect. Possesses fast and long-lasting anti-allergic action.
Loratadine does not penetrate the BBB and does not affect the central nervous system. Has no clinically significant anticholinergic or sedative effect, i.e. does not cause drowsiness and does not affect the speed of psychomotor reactions when used in recommended doses. Taking Claritin does not lead to prolongation of the QT interval on the ECG. At long-term treatment not observed clinically significant changes vital signs, physical examination data, laboratory results or ECG.
Loratadine has no significant selectivity for histamine H 2 receptors. Does not inhibit norepinephrine reuptake and has little or no effect on the cardiovascular system or pacemaker function
Side effects
From the nervous system: in children aged 2 to 12 years - headache (2.7%), nervousness (2.3%), fatigue (1%); in adults - headache(0.6%), drowsiness (1.2%), insomnia (0.1%).
in adults - increased appetite (0.5%).
In the post-marketing period
From the nervous system: rarely (< 1/10 000) - головокружение, утомляемость.
From the side digestive system: rarely (< 1/10 000) - сухость во рту, желудочно-кишечные расстройства (тошнота, гастрит), нарушение функции печени.
Allergic reactions: rarely (< 1/10 000) - сыпь, анафилаксия.
On the part of the cardiovascular system: rarely (< 1/10 000) - сердцебиение, тахикардия.
From the side skin: rarely (< 1/10 000) - алопеция.
Indications
Seasonal (hay fever) and year-round allergic rhinitis and allergic conjunctivitis (to eliminate symptoms associated with these diseases - sneezing, itching of the nasal mucosa, rhinorrhea, burning sensation and itching in the eyes, lacrimation); - chronic idiopathic urticaria; - skin diseases of allergic origin ...
33. Means that eliminate common manifestations allergic reactions type of anaphylactic shock. Epinephrine, Eufillin, prednisolone. The main pharmacological effects, the purpose of prescribing each drug and undesirable effects.
ANTI-ALLERGIC DRUGS(antiallergica; syn. desensitizing agents) - medicines that prevent or weaken the manifestations of allergic reactions. One of possible ways prevention and treatment of allergic reactions is a so-called method. specific hyposensitization, that is, a decrease in the body's sensitivity to any antigen by repeated administration of the antigen itself in low doses that do not cause manifestations of allergy. In this case, the body gradually loses its sensitivity to the injected antigen.
Adrenalin
Pharmacological action Adrenomimetic, has a direct stimulating effect on α- and β-adrenergic receptors. Under the action of epinephrine (adrenaline), due to the stimulation of α-adrenergic receptors, there is an increase in the content of intracellular calcium in smooth muscles. increases the activity of phospholipase C (through stimulation of the G-protein) and the formation of inositol triphosphate and diacylglycerol. Has a pronounced effect on the cardiovascular system. Increases heart rate and strength, stroke and cardiac output. Improves AV conductivity, increases automatism. Increases myocardial oxygen demand. Causes vasoconstriction of the abdominal organs, skin, mucous membranes, to a lesser extent - skeletal muscles. Increases blood pressure (mainly systolic), Epinephrine (adrenaline) relaxes the smooth muscles of the bronchi, lowers the tone and motility of the gastrointestinal tract, dilates the pupils, and helps to lower intraocular pressure. Causes hyperglycemia and increases plasma free fatty acids. Indications Allergic reactions of immediate type (including urticaria, angioedema, anaphylactic shock), developing with the use of drugs, serums, blood transfusions, food, insect bites or other allergens. Bronchial asthma (relief of an attack), bronchospasm during anesthesia. In order to stop bleeding. Side effect From the side of the cardiovascular system: angina pectoris, bradycardia or tachycardia, palpitations, increase or decrease in blood pressure; when used in high doses - ventricular arrhythmias; rarely - arrhythmia, chest pain. From the nervous system: headache, anxiety, tremor, dizziness, nervousness, fatigue, psychoneurotic disorders
Euphyllin
pharmachologic effect
Bronchodilator, xanthine derivative; inhibits phosphodiesterase, increases the accumulation of cyclic adenosine monophosphate in tissues, blocks adenosine (purine) receptors; reduces the flow of calcium ions through the channels of cell membranes, reduces the contractile activity of smooth muscles. Relaxes the bronchial muscles, increases mucociliary clearance, stimulates diaphragm contraction, improves the function of the respiratory and intercostal muscles, stimulates the respiratory center, increases its sensitivity to carbon dioxide and improves alveolar ventilation, which ultimately leads to a decrease in the severity and frequency of apnea episodes. By normalizing the respiratory function, it contributes to the saturation of blood with oxygen and a decrease in the concentration of carbon dioxide. It has a stimulating effect on the activity of the heart, increases the strength and number of heart contractions, increases coronary blood flow and myocardial oxygen demand. Reduces the tone of blood vessels (mainly the vessels of the brain, skin and kidneys). It has a peripheral venodilating effect, reduces pulmonary vascular resistance, reduces pressure in the "small" circle of blood circulation. Increases renal blood flow, has a moderate diuretic effect. Expands the extrahepatic biliary tract. It inhibits platelet aggregation (inhibits platelet activation factor and PgE2 alpha), increases the resistance of erythrocytes to deformation (improves the rheological properties of blood), reduces thrombus formation and normalizes microcirculation. Has a tocolytic effect, increases the acidity of gastric juice. When used in large doses, it has an enileptogenic effect.
Side effects
From the nervous system: dizziness, headache, insomnia, agitation, anxiety, irritability, tremor.
On the part of the cardiovascular system: palpitations, tachycardia (including in the fetus when taken by a pregnant woman in the third trimester), arrhythmias, cardialgia, a decrease in blood pressure, an increase in the frequency of angina attacks.
From the digestive system: gastralgia, nausea, vomiting, gastroesophageal reflux, heartburn, exacerbation of peptic ulcer disease, diarrhea, with prolonged use - decreased appetite.
Allergic reactions: skin rash, itching, fever.
Others: chest pain, tachypnea, flushing, albuminuria, hematuria, hypoglycemia, increased urine output, increased sweating.
Indications
Broncho-obstructive syndrome of any genesis: bronchial asthma (the drug of choice in patients with physical exertion asthma and as an additional remedy for other forms), chronic obstructive pulmonary disease, pulmonary emphysema, chronic obstructive bronchitis, pulmonary hypertension, pulmonary heart, sleep apnea.
Prednisone
pharmachologic effect
Synthetic GCS. Has a pronounced anti-inflammatory effect. The drug inhibits the development of symptoms of inflammation. It inhibits the accumulation of macrophages, leukocytes and other cells in the area of inflammation. Inhibits phagocytosis, the release of microsomal enzymes, as well as the synthesis and release of inflammatory mediators. It causes a decrease in capillary permeability, inhibition of leukocyte migration.
Enhances the synthesis of lipomodulin, an inhibitor of phospholipase A2, which releases arachidonic acid from phospholipid membranes while inhibiting its synthesis.
The mechanism of the immunosuppressive action of prednisone is not fully understood. The drug reduces the number of T-lymphocytes, monocytes and acidophilic granulocytes, as well as the binding of immunoglobulins to receptors on the cell surface, inhibits the synthesis or release of interleukins by reducing blastogenesis of T-lymphocytes; reduces early immunological response. It also inhibits the penetration of immunological complexes through membranes and reduces the concentration of complement components and immunoglobulins.
Prednisolone acts on the distal renal tubules, enhancing the reabsorption of sodium and water, as well as increasing the excretion of potassium and hydrogen ions.
Prednisolone inhibits the secretion of ACTH by the pituitary gland, which leads to a decrease in the production of corticosteroids and androgens by the adrenal cortex. After long-term use of the drug in high doses, the function of the adrenal glands can be restored within a year, and in some cases, persistent suppression of their function develops. Prednisolone enhances protein catabolism and induces enzymes involved in the metabolism of amino acids. It inhibits the synthesis and enhances the catabolism of proteins in the lymphatic, connective, muscle tissue. With prolonged use, the development of atrophy of these tissues (as well as the skin) is possible.
Increases the concentration of glucose in the blood by inducing enzymes of gluconeogenesis in the liver, stimulating protein catabolism (which increases the amount of amino acids for gluconeogenesis) and decreasing glucose consumption in peripheral tissues. This leads to an accumulation of glycogen in the liver, an increase in blood glucose concentration and an increase in insulin resistance.
Indications
Endocrinological diseases:
Insufficiency of the adrenal cortex: primary (Addison's disease) and secondary; - adrenogenital syndrome (congenital adrenal hyperplasia); - acute insufficiency of the adrenal cortex;
Before surgical interventions and in case of serious illnesses and injuries in patients with adrenal insufficiency; - subacute thyroiditis.
Severe allergic diseases resistant to other therapy: - contact dermatitis; - atopic dermatitis; - serum sickness; - hypersensitivity reactions to drugs;
Permanent or seasonal allergic rhinitis; - anaphylactic reactions; - angioedema.
Rheumatic diseases:
Rheumatoid arthritis, juvenile rheumatoid arthritis (in cases resistant to other treatments);
Dermatological diseases: - exfoliative dermatitis; - herpetiformis bullous dermatitis;
Severe seborrheic dermatitis; - Severe erythema multiforme (Stevens-Johnson syndrome);
Side effects
With short-term use of prednisolone (like other corticosteroids), side effects are rare. When using prednisolone for a long time, the following side effects may develop.
On the part of the water-electrolyte balance: retention in the body of sodium and fluid, hypokalemia.
From the musculoskeletal system: muscle weakness, steroid myopathy, loss of muscle mass, osteoporosis, spinal compression fracture.
From the digestive system: steroid ulcer with possible perforation and bleeding, pancreatitis, flatulence, ulcerative esophagitis, indigestion, nausea, increased appetite.
Dermatological reactions: skin atrophy, striae, acne, delayed wound healing, thinning of the skin, petechiae, hematomas, erythema, increased sweating, allergic dermatitis, urticaria, angioedema.
From the side of the central nervous system and peripheral nervous system: increased intracranial pressure with congestive nipple syndrome of the optic nerve (occurs most often in children, after a too rapid dose reduction, symptoms - headache, deterioration of visual acuity, double vision); convulsions, dizziness, headache, sleep disturbances.
From the endocrine status: secondary adrenal and hypothalamic-pituitary insufficiency (especially during stressful situations: illness, injury, surgery); Cushing's syndrome.
Others: anaphylactic reactions, hypersensitivity reactions; obliterating arteritis, weight gain, fainting.
1. The essence of pharmacology as a science. Sections and fields of modern pharmacology. Basic terms and concepts of pharmacology - pharmacological activity, action, effectiveness chemical substances.
Pharmacology- the science of medicines in all aspects - theoretical basis therapy:
a) the science of the interaction of chemicals with living systems
b) the science of managing the vital processes of the body with the help of chemicals
Development of pharmacology goes in two main directions: basic research to clarify the principles and mechanisms of drug action and develop effective drugs as the basis for the treatment of diseases.
Pharmacology is subdivided into:
1. The general- studies general patterns of interaction medicinal substances with living organisms.
Private- considers specific pharmacological groups and individual drugs
2. Experimental (basic) pharmacology- studies the effect of drugs in an experiment.
Clinical pharmacology- studies clinical efficacy and safety
the use of drugs in patients, optimizes the patient's treatment program, taking into account
his condition.
Toxicology- studies the toxic effect on organs various substances(including
and medicinal).
Sections of modern pharmacology:
1) pharmacodynamics- studies a) the effect of drugs on the human body, b) the interaction of various drugs in the body while prescribing them, c) the effect of age and various diseases on the effect of drugs
2) pharmacokinetics- studies the absorption, distribution, metabolism and excretion of drugs (i.e. how the patient's body reacts to drugs)
3) pharmacogenetics- studies the role of genetic factors in the formation of the body's pharmacological response to drugs
4) pharmacoeconomics- evaluates the results of use and the cost of drugs for making a decision on their subsequent practical use
5) pharmacoepidemiology- examines the use of drugs and their effects at the population level, or large groups people to ensure the use of the most effective and safest drugs
Basic terms and concepts:
Pharmacological (biological) activity- the property of a substance to cause changes in the biosystem (human body). Pharmacological substances = biologically active substances(BAS)
pharmachologic effect- the influence of drugs on the object and its targets
Pharmacological effect- the result of the action of a substance in the body (modification of physiological, biochemical processes, morphological structures) - quantitative, but not qualitative change in the state of biosystems (cells, tissues, organs).
The effectiveness of drugs- the ability of drugs to cause certain necessary this case pharmacological effects in the body. Assessed on the basis of "substantial evidence" - adequate well-controlled studies and clinical trials conducted by experts with appropriate scientific training and experience in drug research of this type (FDA)
2. Sources and stages of drug creation. Medicines - generics, placebo - effects Definition of the concepts of drug, drug, drug and dosage form.
Sources of drug creation:
a) natural raw materials: plants, animals, minerals, waste products of microorganisms (cardiac glycosides, porcine insulin, AB)
b) modified natural biologically active substances
c) products of chemical synthesis (methods: pharmacological screening, molecular design, reproduction of biogenic amines, targeted modification of molecules with already known activity, synthesis of pharmacologically active metabolites, random findings ("serendipitic" method))
d) genetic engineering products (recombinant insulin, interferons)
Stages of drug creation:
1. Synthesis of drugs in a chemical laboratory
2. Preclinical assessment of the activity and undesirable effects of drugs of the Ministry of Health and other organisms
3. Clinical trials of drugs The examination of the documentation by the Pharmacological Committee is carried out after the completion of each phase. The medicine can be withdrawn at any stage. (Phase I - assessment of tolerance on healthy volunteers 20-25 years old, phase II - on sick volunteers of less than 100 people suffering from a specific disease, phase III - multicenter clinical trials on large groups of people (up to 1000 people), phase IV - drug monitoring within 5 years after its official permission (performed on a large number of patients (at least 1,000-5,000 people). After the completion of the III phase of clinical trials, the documentation again goes to the Pharmacological Committee (the volume of a full dossier can be up to 1 million pages) and within 1-2 years is registered in the State Register of Medicines and Products medical purpose... Only after that the pharmaceutical concern has the right to start industrial production medicinal product and its distribution through the pharmacy network.
A generic drug is a generic drug that is a replica of the original drug for which the patent has expired. May differ from the original drug in the composition of excipients. A prerequisite for the sale of generics is evidence-based pharmaceutical, biological and therapeutic equivalence to the parent drug. Generic medicines are always cheaper than their branded counterparts, because the company does not spend money on 10-15 years of drug research, but uses ready-made data
Placebo- any component of therapy that does not have any specific biological effect on the disease being treated.
It is used for the purpose of control when assessing the effect of drugs and in order to benefit the patient without any pharmacological agents as a result of only psychological influence (i.e. placebo effect).
All treatments have psychological component, or satisfying ( placebo effect), or troubling (nocebo effect). An example of a placebo effect: rapid improvement at the patient viral infection when using antibiotics. The benefit of the placebo effect is associated with psychological impact per patient. It will be maximum only when using it. combined with treatment methods that have a pronounced specific effect. Expensive substances as a placebo also help to achieve a greater response.
Indications for placebo use:
1) weak mental disorders
2) psychological support a patient with an incurable chronic illness or with suspicion of a severe diagnosis
Medicine- any substance or product used to modify or investigate physiological systems or pathological conditions for the benefit of the recipient (according to WHO, 1966); individual substances, mixtures of substances or compositions of unknown composition with proven medicinal properties.
Medicinal substance- an individual chemical compound used as a medicine.
Dosage form- convenient for practical application the form given to a drug to obtain the desired therapeutic or prophylactic effect.
Medicinal product- a medicinal product in a specific dosage form, approved by a government authority.
For example: the drug is the antibiotic ampicillin, the drug is ampicillin trihydrate, which can be produced in the form of tablets or capsules. The drug is ampicillin trihydrate tablets 0.25 g each.
Routes of drug administration into the body and their characteristics. Presystemic elimination of drugs.
but. enteral route of administration: oral, sublingual, buccal, rectal, tube b. parenteral route of administration: intravenously, subcutaneously, intramuscularly, ... 2. For local exposure: skin (epicutary), on mucous membranes, in cavities (abdominal, pleural, articular), in tissue ...Transport of drugs across biological barriers and its varieties. The main factors affecting the transport of drugs in the body.
1) Filtration (water diffusion) - passive movement of substance molecules along a concentration gradient through pores filled with water in the membrane of each ... 2) Passive diffusion (lipid diffusion) - the main mechanism of drug transfer, ... 3) Transport using specific carriers - drug transfer using carriers built into the membrane (more often ...Transport through membranes of medicinal substances with variable ionization (Henderson-Hasselbalch ionization equation). Transfer control principles.
All drugs are weak acids or weak bases, which have their own values of the ionization constant (pK). If the pH value of the medium is equal to the pK value of the drug, then 50% of its molecules will be in the ionized state and 50% in the non-ionized state, and the medium for the drug will be neutral.
IN acidic environment(pH is less than pK), where there is an excess of protons, the weak acid will be in the undissociated form (R-COOH), i.e. will be associated with a proton - protonated. This form of acid is uncharged and readily soluble in lipids. If the pH shifts to the alkaline side (i.e., the pH becomes greater than pK), then the acid will begin to dissociate and lose a proton, passing into the non-protonated form, which has a charge and is poorly soluble in lipids.
In an alkaline medium, where there is a deficiency of protons, the weak base will be in the undissociated form (R-NH 2), i.e. will be unprotonated and devoid of charge. This form of base is highly lipid soluble and rapidly absorbed. In an acidic medium, there is an excess of protons and the weak base will begin to dissociate, while binding the protons and forming the protonated, charged form of the base. This form is poorly soluble in lipids and poorly absorbed.
Consequently, absorption of weak acids occurs mainly in an acidic medium, and weak bases in an alkaline medium.
Features of the metabolism of weak acids (SC):
1) stomach: SA in the acidic contents of the stomach is non-ionized, and in the alkaline medium of the small intestine it will dissociate and the SA molecules will acquire a charge. Therefore, absorption of weak acids will be most intense in the stomach.
2) in the blood, the medium is sufficiently alkaline and the absorbed SC molecules will transform into an ionized form. The filter of the glomeruli of the kidneys allows both ionized and non-ionized molecules to pass through, therefore, despite the charge of the molecule, SCs will be excreted into primary urine
3) if the urine is alkaline, then the acid will remain in an ionized form, will not be able to reabsorb back into the bloodstream and will be excreted in the urine; If urine is acidic, then the medicine will go into a non-ionized form, which is easily reabsorbed back into the bloodstream.
Features of the metabolism of weak bases: opposite to SC (absorption is better in the intestine; in alkaline urine they are reabsorbed)
That., to accelerate the elimination of a weak acid from the body, urine must be alkalized, and to accelerate the elimination of a weak base, it must be acidified (detoxification according to Popov).
The quantitative dependence of the drug ionization process at different pH of the medium allows one to obtain the equation Henderson-Hasselbach:
Where pKa corresponds to the pH value at which the concentrations of the ionized and non-ionized forms are in equilibrium .
The Henderson-Hasselbach equation makes it possible to estimate the degree of drug ionization at a given pH value and to predict the probability of its penetration through the cell membrane.
(1)For dilute acid, A,
HA ↔ H + + A -, where HA is the concentration of the non-ionized (protonated) form of the acid and A - is the concentration of the ionized (non-protonated) form.
(2) For weak base, B,
BH + ↔ H + + B, where BH + is the concentration of the protonated form of the base, B is the concentration of the non-protonated form
Knowing the pH of the medium and the pKa of the substance, it is possible to determine the degree of ionization of the drug from the calculated logarithm, and hence the degree of its absorption from gastrointestinal tract, reabsorption or excretion by the kidneys with different meanings urine pH, etc.
Transport control principles.
For faster absorption
Ø weak acids (ASA) - the pH of the gastric juice must be acidic;
Ø weak based - the pH of the gastric juice should be neutral.
To speed up the withdrawal
Ø weak acids - the urine is made alkaline;
Ø weak bases - acidify urine.
Transfer of drugs in the body. Water diffusion and diffusion in lipids (Fick's law). Active transport.
The transfer of drugs in the body can be carried out by water and lipid diffusion, active transport, endocytosis and pinocytosis.
Features of the transfer of drugs in the body by water diffusion:
1. Epithelial integuments (mucous membranes of the gastrointestinal tract, oral cavity, etc.) - water diffusion of only very small molecules (methanol, lithium ions, etc.)
2. Capillaries (except for cerebral ones) - filtration of substances with a molecular weight of up to 20-30 thousand. Yes.
3. Capillaries of the brain - basically do not have water pores, with the exception of the areas of the pituitary gland, pineal gland, zone IV ventricle, choroid plexus, median eminence
4. Placenta - has no water pores (although a controversial issue).
5. Binding of drugs to blood proteins prevents their release from the bloodstream, and hence water diffusion
6. Diffusion in water depends on the size of drug molecules and water pores
Features of lipid diffusion:
1. The main mechanism of drug transfer across cell membranes
2. Determined by the lipophilicity of the diffusible substance (ie the oil / water distribution coefficient) and the concentration gradient, it can be limited by the very low solubility of the substance in water (which prevents the drug from penetrating into the aqueous phase of membranes)
3. Non-polar compounds diffuse easily, ions are difficult to diffuse.
Any diffusion (both water and lipids) obeys Fick's law of diffusion:
Diffusion rate - the number of drug molecules carried per unit time; С 1 - the concentration of the substance outside the membrane; С 2 - the concentration of the substance from the inside of the membrane.
Corollary from Fick's law:
1) the filtration of the drug is the higher, the greater its concentration at the injection site (S of the absorbed surface in the intestine is greater than in the stomach, therefore the absorption of the drug into the intestine is faster)
2) the higher the drug concentration at the injection site, the higher the drug filtration
3) the filtration of drugs is the higher, the less the thickness of the biological membrane to be overcome (the thickness of the barrier in the alveoli of the lungs is much less than that of the skin, therefore the absorption rate is higher in the lungs)
Active transport- drug transfer regardless of the concentration gradient using energy ATP, is characteristic of hydrophilic polar molecules, a number of inorganic ions, sugars, amino acids, pyrimidines.
Characterized by: a) selectivity for certain compounds b) the possibility of competition of two substances for one transport mechanism c) saturation at high concentrations of the substance d) the possibility of transport against the concentration gradient e) energy consumption.
7. The central postulate of pharmacokinetics is the concentration of a drug in the blood - the main parameter for controlling the therapeutic effect. Tasks solved on the basis of knowledge of this postulate.
The central postulate (dogma) of pharmacokinetics: drug concentration in blood plasma determines (quantifies) the pharmacological effect.
In most cases, the rate of absorption, distribution, metabolism and excretion of drugs is proportional to their concentration in blood plasma (obeys the law of mass action), therefore, knowing it is possible:
1) determine the half-life (for drugs with first-order kinetics)
2) explain the duration of some toxic effects of drugs (for drugs in high doses with saturation kinetics)
[C] plasma → [C] on target → effect
Determined by laws is determined by the z-us of pharmacodynamics
Distribution
Objectives: to learn how to control the concentration of the drug in the blood.
Pharmacokinetic models (one-chamber and two-chamber), quantitative laws of drug absorption and elimination.
The whole organism is a single homogeneous container. Assumptions: 1) a rapid dynamic development is established between the drug content in ... 2) the drug is quickly and evenly distributed throughout the blood volumeDistribution of drugs in the body. Compartments, ligands. Main determinants of distribution.
Distribution compartments: 1. Extracellular space (plasma, intercellular fluid) 2. Cells (cytoplasm, organelle membrane)Elimination constant, its essence, dimension, relationship with other pharmacokinetic parameters.
Elimination rate constant(k el, min -1) - shows what part of drugs is eliminated from the body per unit of time Þ Kel = A out / A total, where A out is the amount of drugs released in units. time, And total - the total amount of drugs in the body.
The value of k el is usually found by solving a pharmacokinetic equation describing the process of elimination of a drug from the blood; therefore, k el is called a model kinetic index. K el is not directly related to the planning of the dosage regimen, but its value is used to calculate other pharmacokinetic parameters.
The elimination constant is directly proportional to the clearance and inversely proportional to the volume of distribution (from the definition of clearance): Kel = CL / Vd; = hour -1 / min -1 = fraction per hour.
The half-life of drugs, its essence, dimension, relationship with other pharmacokinetic parameters.
Half-elimination period(t ½, min) is the time required to reduce the concentration of drugs in the blood by exactly half. In this case, it does not matter in what way a decrease in concentration is achieved - with the help of biotransformation, excretion, or due to a combination of both processes.
The half-life is determined by the formula:
![]()
The half-life is the most important pharmacokinetic parameter that allows:
b) determine the time of complete elimination of the drug
c) predict the concentration of drugs at any time (for drugs with first-order kinetics)
Clearance as the main pharmacokinetic parameter for dosing regimen management. Its essence, dimension and relationship with other pharmacokinetic parameters.
Clearance(Cl, ml / min) - the volume of blood that is cleared from drugs per unit of time.
Because plasma (blood) is the "visible" part of the volume of distribution, then clearance is the fraction of the volume of distribution from which the drug is released per unit of time. If we denote the total amount of the drug in the body through And overall, and the amount that was allocated after And vyd, then:
On the other hand, it follows from the definition of the volume of distribution that the total amount of the drug in the body is A total = V d ´C ter / plasma... Substituting this value into the clearance formula, we get:
![]() .
.
Thus, clearance is the ratio of the rate of elimination of a drug to its concentration in blood plasma.
In this form, the clearance formula is used to calculate the maintenance dose of the drug ( D p), that is, the dose of the drug that should compensate for the loss of the drug and maintain its level at a constant level:
Administration rate = elimination rate = Cl'C ter (dose / min)
D p = infusion rate 't (t is the interval between drug intake)
Ground clearance is additive, i.e. elimination of a substance from the body can occur with the participation of processes in the kidneys, lungs, liver and other organs: Cl systemic = Cl renal. + Cl liver + Cl others.
Clearance bound with drug half-life and volume of distribution: t 1/2 = 0.7 * Vd / Cl.
Dose. Types of doses. Drug dosage units. Drug dosing targets, administration methods and options, administration interval.
The effect of drugs on the body is largely determined by their dose.
Dose- the amount of a substance introduced into the body at one time; expressed in weight, volume or conventional (biological) units.
Dose types:
a) single dose - the amount of substance per dose
b) daily dose - the amount of the drug prescribed for a day in one or more doses
c) course dose - the total amount of the drug for the course of treatment
d) therapeutic doses - doses in which the drug is used with therapeutic or preventive purposes(threshold, or minimum effective, average therapeutic and highest therapeutic doses).
e) toxic and lethal doses - doses of drugs at which they begin to have pronounced toxic effects or cause death of the body.
f) loading (introductory) dose - the number of injected drugs, which fills the entire volume of distribution of the body in the effective (therapeutic) concentration: VD = (Css * Vd) / F
g) maintenance dose - a systematically administered amount of drugs that compensates for the loss of drugs with clearance: PD = (Css * Cl * DT) / F
Pharmaceutical dosage units:
1) in grams or fractions of a gram of drugs
2) the number of drugs per 1 Kg body weight (for example, 1 mg / kg) or per unit surface area of the body (for example, 1 mg / m 2)
Drug dosing goals:
1) determine the amount of drugs required in order to cause the desired therapeutic effect with a certain duration
2) avoid the phenomena of intoxication and side effects with the introduction of drugs
Methods of drug administration: 1) enteral 2) parenteral (see section 5)
Drug administration options:
a) continuous (by long-term intravascular infusion of drugs by drip or through automatic dispensers). With continuous administration of drugs, its concentration in the body changes smoothly and does not undergo significant fluctuations.
b) intermittent administration (by injection or non-injection methods) - administration of a drug at regular intervals (dosing intervals). With intermittent administration of drugs, its concentration in the body constantly fluctuates. After taking a certain dose, it first rises, and then gradually decreases, reaching minimum values before the next administration of the drug. Fluctuations in concentration are the more significant, the larger the administered dose of the drug and the interval between injections.
Introduction interval- the interval between the administered doses, ensuring the maintenance of the therapeutic concentration of the substance in the blood.
15. Administration of drugs at a constant rate. Kinetics of drug concentration in blood. Stationary concentration of the drug in the blood (C ss), the time to reach it, its calculation and management.
 The peculiarity of the introduction of drugs at a constant rate is a smooth change in its concentration in the blood upon administration, while:
The peculiarity of the introduction of drugs at a constant rate is a smooth change in its concentration in the blood upon administration, while:
1) the time to reach a steady-state drug concentration is 4-5t ½ and does not depend on the infusion rate (the size of the administered dose)
2) with an increase in the infusion rate (injected dose), the C SS value also increases in a proportional number of times
3) elimination of the drug from the body after the termination of the infusion takes 4-5t ½.
Сss - equilibrium stationary concentration- the concentration of drugs achieved at the rate of administration equal to the rate of excretion, therefore:
![]() (from the definition of clearance)
(from the definition of clearance)
For each subsequent half-life, the drug concentration increases by half of the remaining concentration. All drugs that obey the first order elimination law are will reach Css in 4-5 half-lives.
Approaches to managing the Css level: change the administered dose of drugs or the interval of administration
16. Intermittent administration of drugs. Kinetics of drug concentration in blood, therapeutic and toxic concentration range. Calculation of the stationary concentration (C ss), the boundaries of its fluctuations and its control. Adequate discrete dosing interval.
 Fluctuations in the concentration of drugs in blood plasma: 1 - with constant intravenous drip; 2 - with a fractional introduction of the same daily dose with an interval of 8 hours; 3 - with the introduction of a daily dose with an interval of 24 hours.
Fluctuations in the concentration of drugs in blood plasma: 1 - with constant intravenous drip; 2 - with a fractional introduction of the same daily dose with an interval of 8 hours; 3 - with the introduction of a daily dose with an interval of 24 hours.
Intermittent drug administration- introduction a certain amount Drugs at some intervals.
The steady-state equilibrium concentration is reached after 4-5 half-elimination periods, the time to reach it does not depend on the dose (at the beginning, when the drug concentration level is low, the rate of its elimination is also low; as the amount of the substance in the body increases, the rate of its elimination also increases, therefore, early or a moment will come late when the increased rate of elimination will balance the administered drug dose and further increase in concentration will stop)
Css is directly proportional to the drug dose and inversely proportional to the injection interval and drug clearance.
Css Swing Boundaries: ![]() ; C ss min = C ss max × (1 - e-mail). Fluctuations in drug concentration are proportional to T / t 1/2.
; C ss min = C ss max × (1 - e-mail). Fluctuations in drug concentration are proportional to T / t 1/2.
Therapeutic range (safety corridor, therapy window)- This is the range of concentrations from the minimum therapeutic to causing the first signs of side effects.
Toxic range- concentration range from the highest therapeutic to lethal.
Adequate administration of discrete doses: a mode of administration in which the fluctuation of the drug concentration in the blood falls within the therapeutic range. To determine an adequate regimen of drug administration, it is necessary to calculate. The difference between Css max and Css min should not exceed 2Css.
Controlling Css Fluctuations:
The range of Css fluctuations is directly proportional to the drug dose and inversely proportional to the interval of its administration.
1. Change the dose of drugs: with an increase in the dose of a drug, the range of fluctuations of its Css proportionally increases
2. Change the interval of drug administration: with an increase in the interval of drug administration, the range of fluctuations of its Css proportionally decreases
Simultaneously change the dose and the interval of administration
Introductory (loading) dose. Therapeutic meaning, calculation by pharmacokinetic parameters, conditions and limitations of its use.
Introductory (loading) dose- a dose administered at a time and fills the entire volume of distribution in the current therapeutic concentration. VD = (Css * Vd) / F; = mg / l, = l / kg
Therapeutic meaning: the introductory dose quickly provides an effective therapeutic concentration of drugs in the blood, which makes it possible, for example, to quickly stop an attack of asthma, arrhythmias, etc.
The introductory dose can be administered at a time only when the process of substance distribution is ignored
Limiting the use of VD: if the drug is distributed much slower than its entry into the bloodstream, the introduction of the entire loading dose at once (especially intravenously) will create a concentration significantly higher than the therapeutic one and will cause the occurrence of toxic effects. VD use condition: therefore, the introduction of loading doses should always be slow or fractional.
Maintenance doses, their therapeutic meaning and calculation for the optimal dosing regimen.
Therapeutic sense: PD compensates for losses with clearance over the interval between drug injections. Calculation for optimal dosage of drugs (for quick relief of an attack): ... 1. Calculate VD: VD = (Css * Vd) / FIndividual, age and sex differences in drug pharmacokinetics. Corrections for the calculation of individual values for the volume of distribution of drugs.
2. Sex differences in the action of drugs. For women, less body weight is characteristic than for men, therefore, the size of the doses of the medicine for them should ... 3. Pathological conditions organism and the action of drugs a) liver disease: F drugs due to the shutdown of presystemic metabolism, a fraction of unbound drugs due to a lack of ...Renal clearance of drugs, mechanisms, their quantitative and qualitative characteristics.
Mechanisms of renal clearance and their characteristics: 1. Filtration: drugs released only by filtration (insulin) will have clearance, ... Determined by: renal blood flow, unbound drug fraction and kidney filtration capacity.Factors affecting the renal clearance of drugs. Dependence of clearance on the physicochemical properties of drugs.
a) glomerular filtration b) renal blood flow rate c) maximum secretion rateHepatic drug clearance, its determinants and limitations. Enterohepatic drug cycle.
1) metabolism (biotransformation) by oxidation, reduction, alkylation, hydrolysis, conjugation, etc. The main strategy of xenobiotic metabolism: non-polar substances ® polar ... 2) secretion (excretion of non-transformed substances into bile)Correction of drug therapy for liver damage and other pathological conditions.
Correction of the dosage regimen for kidney disease see above in section 26, general principles correction - v.25. Correction of the dosage regimen under the control of the total clearance of the drug: Correction of the dose: Dind. = Dtypical × Clind. / Cltypical.Correction of the dosage regimen under the control of the residual renal function.
We know: a) the residual renal function, which is determined by creatinine clearance in a given ... b) the total clearance of a given drug (CLP / total) and the proportion of renal drug clearance in the total clearanceIndividual drug therapy strategy.
Confession important role concentration as connecting link pharmacokinetics and pharmacodynamics contributes to the creation of a strategy of target concentration - dose optimization in a given patient based on the measurement of drug concentration. It consists of the following stages:
1. Choice of target concentration
2. Calculate V d and Cl based on typical values and make adjustments for factors such as body weight and renal function.
3. Entering the loading dose or maintenance dose, calculated taking into account the values of TC, V d and Cl.
4. Registration of the patient's reaction and determination of drug concentration
5. Revision of V d and Cl based on the results of concentration measurements.
6. Repeat steps 3-6 to adjust the maintenance dose required for optimal drug response.
Biotransformation of drugs, its biological meaning, main direction and influence on the activity of drugs. The main phases of metabolic transformations of drugs in the body.
Biotransformation of drugs - chemical transformations of drugs in the body.
The biological meaning of biotransformation of drugs: the creation of a substrate that is convenient for subsequent disposal (as an energy or plastic material) or to accelerate the elimination of drugs from the body.
The main direction of the metabolic transformations of drugs: non-polar drugs → polar (hydrophilic) metabolites excreted in the urine.
There are two phases of metabolic reactions of drugs:
1) metabolic transformation (non-synthetic reactions, phase 1) - the transformation of substances due to microsomal and extra microsomal oxidation, reduction and hydrolysis
2) conjugation (synthetic reactions, phase 2) - a biosynthetic process accompanied by the addition of a number of chemical groups or molecules of endogenous compounds to a drug or its metabolites by a) the formation of glucuronides b) glycerol esters c) sulfoesters d) acetylation e) methylation
The effect of biotransformation on the pharmacological activity of drugs:
1) most often, biotransformation metabolites do not have pharmacological activity or their activity is reduced in comparison with the initial substance
2) in some cases, metabolites can retain activity and even exceed the activity of the parent substance (codeine is metabolized to more pharmacologically active morphine)
3) sometimes toxic substances are formed during biotransformation (metabolites of isoniazid, lidocaine)
4) sometimes in the course of biotransformation, metabolites with opposite pharmacological properties are formed (metabolites of nonselective agonists b 2 - adrenergic receptors have the properties of blockers of these receptors)
5) a number of substances are prodrugs that initially do not give pharmacological effects, but in the course of biotransformation they are converted into biologically active substances (inactive L-dopa, penetrating through the BBB, turns into active dopamine in the brain, while there are no systemic effects of dopamine).
Clinical significance of drug biotransformation. Factors affecting their btotransformation. Metabolic drug interactions.
Influence on biotransformation of drugs various factors: a) the functional state of the liver: in its diseases, the clearance of drugs is usually ... b) the influence of environmental factors: smoking promotes the induction of cytochrome P450, as a result of which the metabolism of drugs in ...Ways and mechanisms of drug elimination from the body. Possibilities of drug elimination management.
Ways and mechanisms of drug excretion: elimination of drugs by the liver and kidneys and some other organs:
a) by the kidneys by filtration, secretion, reabsorption
b) by the liver by biotransformation, excretion with bile
c) through the lungs, saliva, sweat, milk, etc. by secretion, evaporation
Possibilities for managing the processes of drug withdrawal:
1. pH control: in alkaline urine, the excretion of acidic compounds increases, in acidic urine, the excretion of basic compounds
2.application choleretic drugs(cholenzym, allochol)
3.hemodialysis, peritoneal dialysis, hemosorption, lymphosorption
4.forced diuresis (IV NaCl or glucose for water load+ furosemide or mannitol)
5.gastric lavage, use of enemas
The concept of receptors in pharmacology, the molecular nature of receptors, signaling mechanisms of drug action (types of transmembrane signaling and secondary messengers).
Receptors - molecular components of a cell or organism that interact with drugs and induce a number of biochemical events leading to the development of a pharmacological effect.
The concept of receptors in pharmacology:
1. Receptors determine the quantitative patterns of drug action
2. Receptors are responsible for the selectivity of drug action
3. Receptors mediates the action of pharmacological antagonists
The concept of receptors is the basis for the targeted use of drugs that affect regulatory, biochemical processes and communication.
Molecular nature of receptors:
1.regulatory proteins, mediators of the action of various chemical signals: neurotransmitters, hormones, autocoids
2.enzymes and transmembrane transporter proteins (Na +, K + ATPase)
3.structural proteins (tubulin, cytoskeletal proteins, cell surface)
4.nuclear proteins and nucleic acids
Signaling mechanisms of drug action:
1) the penetration of lipid-soluble ligands through the membrane and their effect on intracellular receptors.
2) the signaling molecule binds to the extracellular domain of the transmembrane protein and activates the enzymatic activity of its cytoplasmic domain.
3) the signaling molecule binds to the ion channel and regulates its opening.
4) the signaling molecule binds to a receptor on the cell surface, which is coupled to the effector enzyme via the G-protein. The G-protein activates a secondary messenger.
Types of transmembrane signaling:
a) through 1-TMS receptors with and without tyrosine kinase activity
b) through 7-TMS receptors associated with G-protein
c) through ion channels (ligand-dependent, voltage-dependent, gap contacts)
Secondary intermediaries: cAMP, Ca2 + ions, DAG, IF3.
Physicochemical and chemical mechanisms of action of medicinal substances.
The main pharmacological effects: 1) narcotic 2) general depressive 3) paralyzing 4) locally irritating 5) membranolytic action. Chemical nature of substances: chemically inert hydrocarbons, ethers, alcohols, ... Mechanism of action - reversible destruction of membranes.Selectivity and specificity of drug action. Therapeutic, side and toxic effects of drugs, their nature from the standpoint of the concept of receptors. A therapeutic strategy for combating side and toxic effects of drugs.
Specificity–Binding of drugs with a strictly specific type of receptor.
Selectivity- is able to bind drugs to one or more types of receptors more accurately than others.
It is more preferable to use the term selectivity, since it is unlikely that any drug molecule can bind to only one type of receptor molecule, since the number of potential receptors in each patient is astronomical.
Therapeutic action- the main desired pharmacological effect expected from a given pharmacological preparation.
Side effects- those effects that occur when substances are used in therapeutic doses and constitute the spectrum of their pharmacological action.
Toxic effects- undesirable effects manifested in this drug when it leaves the therapeutic range.
Relationships between the therapeutic and toxic effects of drugs based on the analysis of receptor-effector mechanisms:
1) therapeutic and toxic effects mediated by the same receptor-effector mechanism (prazosin acts as an alpha-selective antagonist on vascular SMC receptors and has a hypotensive effect in essential hypertension, but at a high dose, the patient may experience postural hypotension)
2) therapeutic and toxic effects mediated by identical receptors, but various fabrics or by various effector pathways (cardiac glycosides are used to increase the contractility of the myocardium, at the same time they disrupt the function of the gastrointestinal tract, vision due to the blockade of Na + / K + -ATPase of the cell membrane)
3) therapeutic and toxic effects, mediated different types receptors (for example, norepinephrine has a hypertensive effect through a 1 -Ar, but at the same time causes tachycardia through b 1 -Ar)
Therapeutic strategy for combating therapeutic and side effects LS:
1. The drug should always be administered in the lowest dose that produces an acceptable therapeutic effect.
2. Reducing the dose of one drug due to the appointment of another drug with similar action, but through other receptors and with a different toxicity profile.
3. The selectivity of the drug action can be increased by controlling the drug concentration in the region of the receptors of various parts of the body ( local application LS - inhalation use of salbutamol for bronchial asthma)
32. Terms and concepts of quantitative pharmacology: effect, efficacy, activity, agonist (full, partial), antagonist. Clinical difference between the concepts of activity and effectiveness of drugs.
 Effect (response)- quantitative yield of the reaction of interaction of a cell, organ, system or organism with a pharmacological agent.
Effect (response)- quantitative yield of the reaction of interaction of a cell, organ, system or organism with a pharmacological agent.
Efficiency- the measure of the reaction along the axis of the effect - the magnitude of the response of the biological system to the pharmacological effect; it is the ability of drugs to provide the maximum possible effect for him... Those. in fact, this is the maximum effect size that can be achieved with the administration of a given drug. Numerically characterized by the value of E max. The higher E max, the higher the effectiveness of the drug
Activity- a measure of sensitivity to drugs along the concentration axis, characterizes the affinity (the affinity of the ligand for the receptor), shows what dose (concentration) of the drug is capable of causing the development of a standard effect equal to 50% of the maximum possible for this drug. Numerically characterized by the value of EC 50 or ED 50. The higher the drug activity, the lower its dose is required to reproduce the therapeutic effect.
Efficiency: 1 = 2> 3
Activity: 1> 3> 2
In clinical practice, it is more important to know the effectiveness, rather than the activity, because we are more interested in the ability of drugs to cause a certain effect in the body.
Agonist- a ligand that binds to the receptor and causes a biological response, the activation of the physiological system. Full agonist- maximum response, partial- cause less reaction even when all receptors are occupied.
 Antagonist- ligands that occupy receptors or change them in such a way that they lose the ability to interact with other ligands, but do not themselves cause a biological reaction (block the action of agonists).
Antagonist- ligands that occupy receptors or change them in such a way that they lose the ability to interact with other ligands, but do not themselves cause a biological reaction (block the action of agonists).
Competitive antagonists- interact with receptors reversibly and thus compete with agonists. Increasing the concentration of the agonist can completely eliminate the effect of the antagonist. Competitive antagonist shifts the dose-effect curve for the agonist, increases EC 50, does not affect E max.
Non-competitive antagonists- irreversibly change the affinity of receptors for the agonist, binding often does not occur with the active site of the receptor, an increase in the concentration of the agonist does not eliminate the effect of the antagonist. A noncompetitive antagonist decreases Emax, does not change the EC50, and the dose-response curve is compressed about the vertical axis.
33. Quantitative patterns of drug action. The law of decreasing the response of biological systems. Clark's model and its consequences. General form dependences concentration - effect in normal and lognormal coordinates.
Clark-Ariens model:
1. The interaction between ligand (L) and receptor (R) is reversible.
2. All receptors for a given ligand are equivalent and independent (their saturation does not affect other receptors).
3. The effect is directly proportional to the number of occupied receptors.
4. The ligand exists in two states: free and bound to the receptor.
A), where Kd is the equilibrium constant, Ke is the internal activity.
B) Because with an increase in the number of ligands at some point in time, all receptors will be occupied, then the maximum possible number of ligand-receptor complexes formed is described by the formula:
= [R] × (1)
The effect is determined by the likelihood of activation of the receptor upon binding to the ligand, i.e. its internal activity (Ke), therefore E = Ke ×. In this case, the effect is maximum at Ke = 1 and minimum and Ke = 0. It is natural that maximum effect is described by the relation Emax = Ke ×, where is the total number of receptors for a given ligand
The effect also depends on the concentration of the ligand on the [C] receptors, therefore
It follows from the above relations that EC 50 = Kd

E max is the maximum effect, B max is the maximum number of bound receptors, EC 50 is the drug concentration at which an effect equal to half of the maximum occurs, K d is the constant of dissociation of the substance from the receptor, at which 50% of the receptors are bound.
The law of decreasing response the parabolic dependence "concentration - efficiency" corresponds. The response to low doses of drugs usually increases in direct proportion to the dose... However, as the dose is increased, the increase in response decreases and ultimately a dose can be reached at which there is no further increase in response (due to the occupation of all receptors for a given ligand).
Gradual and quantum evaluation of the effect, essence and clinical applications. Quantification of the activity and effectiveness of drugs in experimental and clinical practice.
All pharmacological effects can be roughly divided into two categories:
but) gradual (continuous, integral) effects- such effects of drugs that can be measured quantitatively (the effect of antihypertensive drugs - by the level of blood pressure). The gradual "dose-effect curve" (see p. 33) is described, on the basis of which it is possible to estimate: 1) individual sensitivity to drugs; 2) drug activity; 3) maximum drug efficiency.
b) quantum effects- such effects of drugs, which are a discrete quantity, a qualitative feature, i.e. described by just a few options for conditions (headache after taking an analgesic, either there or not). A quantum dose-effect curve is described, where the dependence of the manifestation of the effect in the population on the value of the taken drug dose is noted. The dose-effect plot is dome-shaped and is identical to the Gaussian normal distribution curve. Based on the quantum curve, one can: 1) estimate the population sensitivity of drugs; 2) note the presence of an effect at a given dose; 3) choose an average therapeutic dose.
Differences between gradual and quantum dose-effect characteristics:
A quantitative assessment of the activity and effectiveness of drugs is carried out on the basis of constructing dose-effect curves and their subsequent assessment (see Clause 32)
Types of drug action. Changes in the action of drugs when they are repeated.
1. By localization: · local - the action that occurs at the site of application of the drug (usually the skin and ... · resorptive - this is the effect that the drug has when absorbed into the bloodstream or directly injected into ...The dependence of the action of drugs on age, gender and individual abilities of the body. The meaning of circadian rhythms.
Children - the field of pharmacology, which studies the characteristics of the action of drugs on children's organism, is called pediatric pharmacology. ... · elderly people - in the elderly and old age pharmacokinetic ... 2. Gender - animal experiments and clinical observations show that there are sex differences in ...Variability and variability of drug action. Hypo- and hyperreactivity, tolerance and tachyphylaxis, hypersensitivity and idiosyncrasy. Reasons for the variability of drug action and rational therapy strategy.
Variability of drug action - reflects the difference in the pharmacological effects of one drug in different individuals.
Variability of drug action - reflects the ability of a drug to have an effect that differs from its typical pharmacological effects.
Variants of variability and variability of drug action:
1. Hyporeactivity- a decrease in the effect of a given dose of drugs in comparison with the effect that is observed in most patients.
2. Hyperreactivity- an increase in the effect of a given dose of drugs in comparison with the effect that is observed in most patients.
3. Tolerance- a decrease in the body's response to repeated injections of drugs; in order to restore the reaction to drugs, it has to be administered in larger and larger doses.
4. Tachyphylaxis- a condition in which frequent administration of drugs causes the development of tolerance after a few hours, but with sufficiently rare administration of drugs, its effect is fully preserved. The development of tachyphylaxis is usually associated with depletion of the effector systems.
5. Hypersensitivity- the development of an allergic or other immune reaction to the repeated administration of drugs.
6. Idiosyncrasy- a perverse reaction of the body to drugs associated with genetic characteristics of drug metabolism or individual immunological reactivity.
The main reasons for the variability of the drug action:
1) a change in the concentration of a substance in the receptor zone - due to differences in the rate of absorption, its distribution, metabolism, elimination
2) variations in the concentration of the endogenous ligand - the receptor - propranolol (β-blocker) slows down the heart rate in people with elevated level catecholamines in the blood, but does not affect the background heart rate in athletes.
3) changes in the density or function of receptors.
4) changes in the reaction components located distal to the receptor.
Rational therapy strategy: consists in the fact that for the appointment of a drug and in order for it to have the expected effect, it is necessary to take into account the individual factors of the body (age, gender, etc.), the daily rhythms of a person, the presence of chronic diseases and other abnormalities. It is also necessary to predict the development of uncharacteristic effects, taking into account all possible options variability of drug action.
Drug safety assessment. Therapeutic index and standard safety margins.
Huge funds are spent on the creation and implementation of a new drug - from 100 to 350 million dollars and more. These costs include the labor expended on ... In order to pass all stages of the assessment of the drug must correspond to the main ... The safety assessment of new drugs is carried out in 2 stages:Pharmacokinetic drug interactions (examples).
Pharmacokinetic interaction of drugs is a type of pharmacological interaction, i.e. the interaction of drugs, which manifests itself only when they enter the human body together.
Pharmacokinetic interaction occurs at the stage of absorption, distribution and deposition, metabolism and excretion.
1. During the suction phase- this type of interaction can lead to an increase or decrease in their absorption. It can be avoided if the interval between drugs is taken at least 4 hours.
When the drug is administered per os, its absorption is determined by:
· pH of the medium- non-ionized drugs are absorbed in the gastrointestinal tract better than ionized ones, therefore, an increase in the pH of gastric juice increases the absorption of weak bases and reduces the absorption of weak acids. Example: antacids, blockers of H 2 -histamine receptors inhibit the absorption of ketoconazole and other antifungal drugs, indirect anticoagulants, acetylsalicylic acid, barbiturates (almost completely prevent their hypnotic effect); an increase in the pH of the medium improves the absorption of glibutide, accelerates the dissolution of the shell of enteric-soluble substances.
· direct interaction in the digestive tract- the formation of chelate complexes and compounds that are not absorbed in the gastrointestinal tract. NS Examples: activated carbon forms insoluble compounds with drugs, preventing their absorption in case of poisoning; tetracyclines interact with calcium, aluminum, iron, magnesium to form chelate complexes, therefore, their absorption decreases with the use of antacids, bismuth preparations; fluoroquinolones + antacids or sucralfate = reduced effectiveness of antibiotic therapy.
· gastrointestinal motility- can cause either acceleration or deceleration of drug absorption. Examples: prokinetics (metoclopromide) accelerate the absorption of rapidly absorbed drugs (ethanol, paracetamol, tetracycline) and slow down those that are slowly absorbed (digoxin, cimetidine); laxatives reduce the absorption and bioavailability of drugs; when taking anticholinergic drugs, blockers of H 2 -histamine receptors (lengthening the time of passage of drugs through the gastrointestinal tract) increases the bioavailability and absorption of cardiac glycosides, iron preparations, which can lead to the manifestation of toxic effects.
· intestinal microflora - she is directly involved in the absorption of drugs, therefore any dysbiosis is manifested by disorders of drug absorption. Examples: digoxin + erythromycin = an increase in the concentration of digoxin in the blood and the development of undesirable effects; oral contraceptives + broad spectrum AB = reduced contraceptive effect
· damage to intestinal CO- inhibits the absorption of some drugs. Examples: cytostatics (cyclophosphamide) inhibit the absorption of digoxin; impaired absorption of iron preparations, cyanocobalamin, folic acid.
At the stage of distribution and deposit
· Competitive displacement from the bond with blood plasma albumin - if the drug is associated with proteins less than 90%, then displacement from the bond with it will not lead to ... · displacement from the bond with proteins in tissues: quinidine displaces digoxin + ... 3. At the stage of metabolism - drugs can increase or decrease activity enzyme systems involved in the metabolism of drugs (...At the stage of hatching
· Changes in tubular secretion - quinidine + digoxin = increased concentration of digoxin in the blood and the development of toxic effects (quinidine ... · changes in tubular reabsorption - only reabsorption is ...Side and toxic effects of medicinal substances. Teratogenic, embryotoxic, mutagenic effects of drugs. Medical and social aspects fight against drug addiction, drug addiction and alcoholism. The concept of substance abuse.
Side effects- those effects that occur when substances are used in therapeutic doses and constitute the spectrum of their pharmacological action can be primary and secondary:
a) primary side effects - as a direct consequence of the influence of this drug on a specific substrate (hyposalivation when using atropine to eliminate bradyarrhythmia)
b) secondary side effects - indirectly occurring adverse effects (AB, suppressing normal microflora, can lead to superinfection)
Toxic effects- undesirable effects manifested in this drug when it leaves the therapeutic range (drug overdose)
The selectivity of the drug action depends on its dose. The higher the dose of the drug, the less selective it becomes.
Teratogenic action- the ability of drugs, when administered to a pregnant woman, to cause anatomical anomalies of fetal development (thalidomide: phocomelia, antiblastoma drugs: multiple defects)
Embryotoxic action- adverse effects not associated with organogenesis disorders in the first three months of pregnancy. For more later dates manifests itself fetotoxic effect.
Mutagenic effect of drugs- damage to the germ cell and its genetic apparatus of drugs, which is manifested by a change in the genotype of the offspring (adrenaline, cytostatics).
Carcinogenic effect of drugs- the ability of some drugs to induce carcinogenesis.
1) Drug addiction- mental state and / or physical state, which is a consequence of the effect on the body of drugs and is characterized by specific behavioral reactions, it is difficult to overcome the desire to re-take drugs in order to achieve a special mental effect or to avoid discomfort in the absence of drugs in the body. Drug dependence is characterized by:
but) psychological addiction- the development of emotional distress when you stop taking drugs. A person feels empty, plunges into depression, experiences a feeling of fear, anxiety, his behavior becomes aggressive. All these psychopathological symptoms arise against the background of thoughts about the need to inject yourself with drugs that have caused addiction. The urge to take drugs can range from simple desire to a passionate thirst for taking drugs, which absorbs all other needs and turns into the meaning of a person's life. It is believed that psychological dependence develops when a person becomes aware that he can achieve optimal well-being solely through the introduction of drugs. The foundation psychological dependence- a person's belief in the action of the drug (cases of the development of psychological dependence on placebo are described in the literature).
b) physical addiction- violation of normal physiological state organism, which requires the constant presence of drugs in it to maintain a state of physiological balance. Stopping the medication causes the development of a specific symptom complex - withdrawal syndrome - a complex of mental and neurovegetative disorders in the form of dysfunction to the side, the opposite of that, which is characteristic of the action (morphine eliminates pain, depresses the respiratory center, narrows the pupils, causes constipation; with withdrawal, the patient experiences excruciating pain, frequent noisy breathing, pupils are dilated and persistent diarrhea develops)
in) tolerance... Tolerance to drugs that cause drug dependence is often cross-cutting, i.e. arises not only to a given chemical compound, but also to all structurally similar compounds. For example, in patients with drug dependence to morphine, tolerance arises not only to it, but also to other opioid analgesics.
For the development of drug dependence, the presence of all 3 criteria is not necessary condition.
Opioids, barbiturates, alcohol cause strong physical and psychological dependence and tolerance. Anxiolytics (diazepam, alprazolam) predominantly cause psychological dependence.
2) Addiction (drug addiction)- This is an extremely severe form of drug dependence, compulsive use of drugs, characterized by an ever-increasing, irresistible urge to administer this drug, increasing its dose. Desire compulsiveness means that the patient's need to administer the drug dominates all other (even vital) needs. From the standpoint this definition, craving for morphine is drug addiction, while craving for nicotine is drug addiction.
3) Addicted to medicine- characterizes a less intense urge to take medications, when refusal from the medication causes only light feeling discomfort, without the development of physical dependence or a detailed picture of psychological dependence. That. addiction encompasses that part of drug addiction that does not fit the definition of addiction. For example, the aforementioned drug addiction to nicotine is a form of addiction.
4) Drug abuse- unauthorized use of medicines in such doses and in such ways that differ from the accepted medical or social standards in a given culture and in the given time... That. drug abuse covers only the social aspects of drug use. An example of abuse is the use of anabolic steroids in sports or to improve physique by young men.
5) Alcoholism- chronic abuse of alcohol (ethyl alcohol), leading nowadays to damage to a number of organs (liver, gastrointestinal tract, central nervous system, cardiovascular system, immune system) and accompanied by psycho-physical dependence.
6) Substance abuse- chronic abuse of various drugs (including drugs, alcohol, hallucinogens), manifested by a variety of mental and somatic disorders, behavioral disorders, and social degradation.
Drug addiction treatment difficult and thankless task. Still not created effective methodology, which would ensure the success of treatment in more than 30-40% of patients. Reaching anyway notable results is possible only with the full cooperation of the efforts of the patient, the doctor and that social environment, in which the sick person is (the principle of voluntariness and individuality). At the heart of modern techniques lie following principles:
Psychotherapeutic and occupational therapy methods;
Group treatment and rehabilitation (society of alcoholics anonymous, drug addicts)
Gradual or abrupt withdrawal of the drug during detoxification therapy
Substitution therapy (replacement narcotic slow and long-acting analogues with their subsequent cancellation; for example, the so-called. methadone substitution therapy program for heroin addicts)
Treatment with specific antagonists (naloxone and naltrexone) or sensitizing agents (teturam)
Neurosurgical methods of cryodestruction of the cingulate gyrus and hippocampus
42. Pharmaceutical drug interactions. Warnings and precautions for fluid therapy.
Pharmaceutical interactions - the type of interaction associated with a physicochemical reaction between drugs during the manufacture of a medicinal product, even before the introduction of these agents into the human body
but) typical mistakes leading to pharmaceutical incompatibility: writing complex prescriptions, improper storage, the possibility of adsorption of drugs on the surface of plastic (organic nitrates) is not taken into account
b) problems with infusion therapy: mixing of soluble salts, derivatives of insoluble weak acids or bases leads to their precipitation; in liquid dosage forms, cardiac glycosides and alkaloids are hydrolyzed, AB is destroyed; pH of the medium (alkaloids precipitate in an alkaline medium)
c) recommendations: 1) It is better to prepare all mixtures ex tempore 2) The most reliable solution is with one drug 3) All solutions must be checked for suspensions before use 4) Interaction can occur without visible changes in solutions 5) Drugs cannot be added to blood and AK solutions 6) In the absence of special instructions, the preparations should be dissolved in 5% glucose solution (pH 3.5-6.5), isotonic NaCl solution (pH 4.5-7.0).
HCl-stabilized glucose solution is incompatible with epinephrine, benzylpenicillin, apomorphine, kanamycin, vitamin C, oleandomycin, cardiac glycosides. Cardiac glycosides are incompatible with atropine, papaverine, platifillin. AB are incompatible with heparin, hydrocortisone. Vitamins of group B are incompatible with each other, with vitamins PP, C. Vitamin PP and C are also incompatible with each other.
Cannot be mixed with any other drugs: phenothiazide, chlorpromazine, barbiturates, vitamin C preparations, amphotericin B, furosemide, sulfadiazine, aminophylline, adrenomimetics.
Types of pharmacotherapy. Deontological problems of pharmacotherapy.
1. etiotropic PT - correction and elimination of the cause of the disease (AB in infectious diseases) 2. pathogenetic PT - impact on the mechanism of disease development (inhibitors ... 3. symptomatic PT - elimination of disease symptoms if it is impossible to influence its cause or pathogenesis (NSAIDs ...Basic principles of treatment and prevention of drug poisoning. Antidote therapy (examples).
Classification of toxic substances (OM):
1. By belonging to certain classes chemical compounds: barbiturates, benzodiazepines, cyanides.
2. By origin: non-biological nature (acids, alkalis, salts of heavy metals), toxic waste products of some MB (botulinum toxin), vegetable origin(alkaloids, glycosides), animal origin (snake and bee venoms)
3. According to the degree of toxicity: a) extremely toxic (DL50< 1 мг/кг) б) высоко токсические (1-50) в) сильно токсические (50-500) г) умеренно токсические (500-5000) д) мало токсические (5000-15000) е) практически нетоксические (> 15.000)
4. By toxicological action: a) nerve-paralytic (bronchospasm, suffocation) b) skin-resorptive c) general toxic (hypoxic convulsions, coma, paralysis) d) suffocating e) lacrimal and irritating e) psychotropic (impaired mental activity, consciousness)
5. Depending on the area of preferential use: industrial poisons, pesticides, household poisons, chemical warfare agents, medicinal substances.
6. Depending on the toxicity of drugs: List A - drugs, the purpose, use, dosing and storage of which, due to their high toxicity, should be done with great care. The same list includes drugs that cause drug addiction; list B - drugs, the appointment, use, dosing and storage of which must be carried out with caution in connection with possible complications when used without medical supervision.
Selectively toxic effect of drugs.
a) cardiotoxic: cardiac glycosides, potassium preparations, antidepressants
b) neurotoxic: psychopharmacological agents, oxyquinolines, aminoglycosides
c) hepatotoxic: tetracyclines, chloramphenicol, erythromycin, paracetamol
d) nephrotoxic: vancomycin, aminoglycosides, sulfonamides
e) gastroenterotoxic: steroid anti-inflammatory drugs, NSAIDs, reserpine
f) hematotoxic: cytostatics, chloramphenicol, sulfonamides, nitrates, nitrites
g) pneumotoxic
Toxicokinetics - studies the absorption, distribution, metabolism and excretion of drugs taken in toxic doses.
The entry of toxic substances into the body is possible a) enterally b) parenterally. The speed and completeness of absorption reflects the rate of development of the toxic effect and its severity.
Distribution in the body: Vd = D / Cmax - the actual volume in which the poisonous substance is distributed in the body. Vd> 5-10 l / kg - OM is difficult to allow for its removal (antidepressants, phenothiazines). Vd< 1 л/кг – ОВ легче удалить из организма (теофиллин, салицилаты, фенобарбитал).
Overdose- changes in pharmacokinetic processes: solubility, connection with proteins, metabolism ® significant increase in the free fraction of drugs ® toxic effect.
The kinetics of the first order with an increase in the concentration of the drug transforms into the kinetics of the zero order.
The toxigenic stage is detoxification therapy, the somatogenic stage is symptomatic therapy.
Toxicodynamics . The main mechanisms of toxic action:
a) mediator: direct (by the type of competitive blockade - FOS, psychomimetics) and indirect (activators or inhibitors of enzymes)
b) interaction with biomolecules and intracellular structures (hemolytic substances)
c) metabolism by the type of lethal synthesis ( ethanol, thiophos)
d) enzymatic (snake venoms, etc.)
Types of action: local, reflex, resorptive.
Poisoning classification:
1. Etiopathogenetic:
a) accidental (self-medication, mistaken reception)
b) deliberate (with the aim of suicide, murder, development of a helpless state in the victim)
2. Clinical:
a) depending on the rate of development of poisoning: acute (intake of a single dose or with a short time interval of a toxic dose of a substance), subacute (delayed development clinical picture after a single dose), chronic
b) depending on the manifestation of the main syndrome: damage to the CVS, damage to the DS, etc.
c) depending on the severity of the patient's condition: mild, moderate, severe, extremely severe
3. Nosological: takes into account the name of the drug, the name of the group of substances
General mechanism of death in case of poisoning:
a) the defeat of the CVS:
1) lowering blood pressure, hypovolemia peripheral vessels, collapse, brady or tachycardia (tricyclic antidepressants, beta blockers, calcium channel blockers)
2) arrhythmias (ventricular tachycardia, fibrillation - tricyclic antidepressants, theophylline, amphetamine)
b) damage to the central nervous system: stupor, coma ® respiratory depression (drugs, barbiturates, alcohol, hypno-sedative drugs)
c) convulsions, muscle hyperreactivity and rigidity ® hyperthermia, myoglobinuria, renal failure, hyperkalemia
Toxicological triad:
1) duration of use, dose and substance ® history.
2) assessment of the state of consciousness by symptoms: respiration, blood pressure, body temperature
3) laboratory data
Basic principles of treatment:
I. The first urgent care : artificial respiration, heart massage, anti-shock therapy, control of water-electrolyte balance
II. Delayed absorption and removal of non-absorbed OM from the body:
Purpose: to end contact with OV
1. Parenteral route:
a) through the lungs:
1) stop inhalation
2) irritating substances (ammonia, formaldehyde) ® to consolidate active movements, to warm, to give oxygen and antifoaming agents (in ammonia antifoam vinegar, and formaldehyde has a dilute solution of ammonia)
b) through the skin: wash off with copious amounts warm water with soap or detergent, specific antidotes, neutralization and termination of exposure to agents on the skin (FOS: washed with water, removed with 10-15% ammonia or 5-6% sodium bicarbonate solution with water; phenolcresol: vegetable oil or ethylene glycol, but it is forbidden Vaseline oil, KMNO 4: 0.5-1% solution ascorbic acid or equal volumes of 3% hydrogen peroxide and 3% solution acetic acid, CCl 4, turpentine, petrol: warm soapy water)
c) when injected into a limb: a tourniquet above the injection site
d) in case of contact with eyes: rinse with warm saline or milk for 10-20 minutes, drip a local anesthetic; in case of contact with acids and alkalis, it cannot be neutralized. Consultation with an ophthalmologist is required.
2. Enteral route: to free the stomach from OM, accelerate the passage
a) removal of OM:
1) preliminary intake of water. Do not take milk (with the exception of caustic poisonous substances) and ethanol (with the exception of methanol).
2) vomiting - indicated mainly in case of poisoning with large tablets or capsules that cannot pass through the probe. Can be provoked by reflex or emetic (NaCl: 1 tablespoon per 1 glass of water; Ipecac syrup: adults 2 tablespoons, children 2 teaspoons; mustard: 1-2 teaspoons per glass of water; apomorphine: 5-10 mg / kg subcutaneously , except for children under 5 years old). Do not induce vomiting after ingestion: organic solvents - danger of inhalation, detergents - foaming, convulsive substances - danger of aspiration, caustic substances - damage to the esophagus)
3) probe gastric lavage - is an emergency and mandatory measure. The stomach is washed if no more than 4-6 hours have passed since the poisoning, sometimes up to 10 hours; in case of poisoning acetylsalicylic acid- after 24 hours. The patient is pre-intubated with a tube with an inflatable cuff: in a coma in the absence of a cough and laryngeal reflex. The stomach is washed with water or saline solution 30 ° C, the procedure takes 4 hours or more. At the end of the wash, activated carbon and sodium sulfate.
b) decrease in absorption from the gastrointestinal tract: activated charcoal inside after gastric emptying + sodium or magnesium sulfate. Features of measures to reduce absorption:
1) organic solvents: do not induce vomiting, gastric lavage after intubation, activated carbon + liquid paraffin
2) detergents: do not induce vomiting and gastric lavage, it is necessary to give a lot of water + defoamers (simethicone)
3) acids and alkalis: do not induce vomiting, gastric lavage through a tube, lubricated vegetable oil after the introduction of a narcotic analgesic - the only indication for giving milk. For acid poisoning - antacids, for alkali poisoning - citric or acetic acid.
III. Removal of absorbed OM from the body
a) forced diuresis (conditions: sufficient renal blood flow and glomerular filtration; pour in-pour out 20-25 liters in 24 hours)
b) peritoneal hemodialysis
c) hemosorption
d) exchange blood transfusion
e) forced hyperventilation
IV. Symptomatic therapy of functional disorders.
2) toxicokinetic - accelerate the biotransformation of OM (trimedoxime bromide, sodium thiosulfate, ethanol, AO) 3) pharmacological - atropine, naloxone 4) immunological antidotesRules for prescribing poisonous, narcotic and potent drugs.
Prescriptions for narcotic substances (morphine, omnopon, promedol, phenamine, cocaine, etc.) and those equated to them, regardless of drugs. f-we are prescribed for special ... In case the lek. Wed-in content. alcohol, then the seal is put to lay down. institutions. “For ... In cases where the max. a dose of poisonous or strong. in-in exceed, required. indicate their number in words with the addition of ...What will we do with the received material:
If this material turned out to be useful to you, you can save it to your page on social networks:
Information about the time of absorption, distribution and elimination, that is, about the pharmacokinetics of medicinal substances, can be expressed mathematically. This is necessary when planning regimens for clinical use. drugs... On the basis of pharmacokinetic data, the principles of rational choice and dosage of the latter are being developed. At the same time, along with these calculations, constant clinical monitoring of the drug's action is required, since pharmacokinetic studies only complement this control and allow more objective conclusions to be drawn.
The elimination of most medicinal substances occurs in accordance with exponential kinetics, namely in such a way that for each equal period of time a constant part of the total amount of the administered medicinal substance disappears from the body. In most cases, the rate at which the drug disappears from the body is reflected in the corresponding rate of decrease in plasma levels of the drug.
The concentration of drugs in biological fluids is determined by liquid or gas-liquid chromatography, radioimmunoassay or enzymatic analysis, polarography or spectrophotometry. Repeated determination of drug concentrations in the blood during the course of treatment is called THERAPEUTIC MONITORING. For this purpose, saliva is sometimes used, which is a protein-free ultrafiltrate of blood.
Based on the obtained values, a graph is plotted, on the abscissa of which the sampling time is marked, and on the ordinate is the concentration of the drug in the biological sample (most often in the blood plasma) in the appropriate units. The resulting curve characterizes the pharmacokinetic processes occurring with the drug. So, after a single intravenous injection, the concentration of the drug in the plasma decreases exponentially. The rate of an exponential process can be characterized in terms of a rate constant (K), reflecting the change in concentration per unit time or through the period of a semi-exponential process (denoted as T 1/2 or t / 2). This period is equal to the time it takes to complete the process by 50%.
The elimination of drugs from the body can be judged by the half-life or elimination half-life, half-life, half-life, which is defined as the time when the concentration of the drug in the blood decreases by 50% of the administered amount of the drug or the elimination of 50% of the bioavailable amount of the drug.
The term "SEMI-ELIMINATION PERIOD" is more successful than the "SEMI-ELIMINATION PERIOD", since drugs are not only excreted, but also biotransformed. The elimination half-life can be determined from the concentration-time graph by measuring the time interval in which any concentration of the substance on the curve has decreased by half.
It is practically important to remember that in one half-life
50% of the drug is excreted from the body, 75% over two periods, 90% over three periods, 94% over four.
Since the complete elimination of the exponential type requires a time longer than four (4) half-lives, then with repeated administration of the drug at shorter intervals, its cumulation (accumulation) is noted. It is estimated that in order to reach a concentration plateau, that is, a constant plasma concentration of the drug, it takes about four periods of the biological half-life of the drug.
It is important that a decrease in drug elimination leads to a lengthening of the biological half-life and prolongation of drug action.
For some drugs, the pharmacological effect may be longer than the t / 2 would suggest. In this regard, drugs such as growth hormone, anaprilin can be administered at intervals longer than their T / 2.
To avoid a dangerous increase in the plasma level of the drug in patients with reduced elimination in case of impaired liver, kidney or cardiovascular system, its maintenance doses should be reduced either by decreasing each dose, or by lengthening the intervals between administration in proportion to the lengthening of their biological half-life. ...
BIOLOGICAL AVAILABILITY OF MEDICINES
To provide a therapeutic effect, the drug must be delivered to those organs or tissues in which its specific action is carried out (in the biophase). With intravascular injection, the drug immediately and completely enters the bloodstream. For other routes of administration (oral, intramuscular, subcutaneous, etc.), before entering the bloodstream, the drug must pass through a number of biological cell membranes (gastric mucosa, liver cells, muscles, etc.) and only then some part of it will enter the systemic circulation. The effect of the drug largely depends on how much of the administered dose of the drug enters the systemic circulation. This indicator characterizes the bioavailability of the agent (F). Thus, in essence, the bioavailability of a drug reflects its concentration at the receptors, that is, in the blood and body tissues after absorption. Naturally, the bioavailability of the same agent will be different for each patient. Obviously, with the intravenous administration of the drug, its bioavailability is approximately 100%, and with other routes of administration, the bioavailability almost never reaches 100%.
Distinguish between ABSOLUTE AND RELATIVE BIOAVAILABILITY. Absolute bioavailability is the proportion of the absorbed drug during extravascular administration in relation to its amount after intravenous administration.
An important indicator is the RELATIVE BIOAVAILABILITY, which determines the relative degree of absorption of the drug from the test drug and from the reference drugs. In other words, the relative bioavailability is determined for different series of drugs, for drugs when changing
production technology, for drugs produced by various manufacturers, for various dosage forms. To determine the relative bioavailability, data on the level of the drug substance in the blood or its excretion in the urine after a single or multiple administration can be used. This term is important when comparing 2 drugs with each other.
Comparative bioavailability of the same drugs made by different firms (example: cocarboxinase of Polish origin and made in Dnepropetrovsk) is determined by comparing chemical, biological and therapeutic equivalences.
CHEMICAL EQUIVALENCE is a coincidence in drugs not only chemical formula drugs, but also the coincidence of isomerism, the spatial configuration of atoms in a drug molecule.
BIOLOGICAL EQUIVALENCE means the same, equal concentration active substance in the blood when taking the drug from different companies.
Finally, THERAPEUTIC EQUIVALENCE implies the same, equivalent therapeutic effect.
If the listed 3 characteristics are the same, the drugs are said to have equal bioavailability (bioavailability). Currently, there are many examples that similar drugs are biologically nonequivalent due to differences in bioavailability. The practitioner should keep this in mind, especially when transferring a patient from one drug to similar drug another firm.
Of course, all these questions can only be answered by a new science - namely, CLINICAL PHARMACOLOGY. It is an independent science with its own subject and research objectives. Why did it stand out as an independent subject? First of all, because, as it turned out, not everything can be studied in an experiment on animals. For example, mental processes, which are highly characteristic only of man.
The rapid development of the pharmaceutical industry has led to the creation of a huge number of medicines. An avalanche of drugs appeared, creating a kind of medicinal jungle. The current situation makes it very difficult to choose the right tool even in one group of drugs, it prevents the doctor from orienting himself on the drug that is optimal for a particular patient. Clinical pharmacology helps to answer all these questions.
As an example, we can cite the possibility of choosing a drug for collagen diseases (connective tissue diseases, rheumatoid arthritis, rheumatism, systemic lupus erythematosus, etc.). With one
sides - acetylsalicylic acid (aspirin), but at the same time, there are other modern non-narcotic analgesics that have, in comparison with aspirin, a number of advantages: naproxen, piroxicam, etc.
What is better, which drug will be more adequate for a given patient, which one gives the most pronounced therapeutic effect? Clinical pharmacology helps to answer these questions.
The main tasks of a clinical pharmacologist are:
1) Choice of medicines to treat a specific pain
2) Determination of the most suitable medicinal products for him
forms and mode of their application.
3) Choice of the route of drug administration.
4) Monitoring the effect of the drug.
For this purpose, sensors are installed that give a constant picture of the concentration of the drug in the blood on the monitor. All other aspects of pharmacokinetics are being studied.
5) Study of undesirable reactions and side effects on drugs, their elimination, as well as study of the consequences of drug interactions in a given patient.
6) Transfer of accumulated knowledge through training.
7) Organization of laboratory and information services and advice on research planning (WHO, 1971).
PHARMACODYNAMICS (PD) is a branch of pharmacology that studies
1) mechanisms of action (that is, the essence of the processes of interaction with tissue, cellular or subcellular receptors - specific or nonspecific) 1.
1 02) pharmacological effects (that is, the content and changes in the effect of the drug depending on the age, sex of the patient, the nature and course of the disease, concomitant pathology), as well as 3) the localization of drug action. In short, PD can be defined as a section of pharmacology that studies the effect of drugs on the body.
Usually, the mechanism of action of a drug is studied in experiments on animals, since they are almost always the same in animals and humans. Knowledge of the mechanism of action of a drug allows the doctor to intelligently choose the necessary drug for treatment.
There are many mechanisms of action of drugs, but all of them can be conditionally reduced into 2 groups.
The first group of mechanisms is associated with those cases when drugs act on specific receptors - that is, these are RECEPTOR MECHANISMS.
The second group of mechanisms is associated with drugs, which, due to their physical and chemical properties do not act through receptors. Here, first of all, one can indicate the effect of drugs on specific enzymes, their physicochemical effect on cell membranes and direct chemical interaction with cell substances.
An example of non-receptor mechanisms is
the case with drugs for anesthesia, say with fluorothane. It is an excellent solvent for fats, therefore it primarily acts on the membranes of nerve cells, causing a pharmacological effect - anesthesia.
Let us examine the main, most often found receptors and mechanisms of action of drugs.
In pharmacological terms, receptors are functional biochemical macromolecular membrane structures that are selectively sensitive to the action of certain chemical compounds, and in our case to the action of drugs. Research recent years showed that pharmacological receptors are proteins or enzymes (G-proteins are a single peptide chain of 7 domains) - in this they fundamental difference from morphological receptors.
Selective sensitivity of a drug to a receptor means the fact that a drug can, firstly, bind to a receptor, that is, it has affinity or affinity for it. In other words, affinity or affinity refers to the ability of a drug to bind to a receptor.
Affinity or affinity reflects the kinetic constants that bind drug, receptor and response to molecular level... The interaction of medicinal substances with the receptor leads to the emergence of a number of biochemical and physiological changes in the body, which are expressed in one effect or another.
The second characteristic of a drug substance is its ability to induce a pharmacological response, the effect after interaction with the receptor. This ability is referred to as the intrinsic activity of the drug or its effectiveness. To a certain extent, the biological response is regulated by changing the number of receptors and their sensitivity.
In the course of evolution, receptors have been formed that are sensitive to a variety of endogenous regulators. According to the receptor theory, the mechanism of action of drugs is to change the rate of functioning of specific body systems when natural mediators or exogenous substances act on receptors.
Medicines, the action of which is associated with direct arousal or increase functionality(abilities) of receptors are called AGONISTS, and substances that interfere with the action of specific agonists are called ANTAGONISTS. In other words, if a drug has both characteristics (that is, both affinity and intrinsic activity), then it is an agonist. Therefore, an agonist is a substance with high affinity for the receptor and high intrinsic activity. If the substance has the ability only to bind to the receptor (that is, it has an affinity), but at the same time is unable to cause pharmacological effects, then it causes a blockade of the receptor and is called an antagonist.
Drugs that have the same affinity for the receptor as the agonist, or weaker, but have less pronounced intrinsic
activity are called partial agonists or agonist-antagonist. These drugs, used concomitantly with agonists, reduce the effect of the latter due to their ability to occupy the receptor.
Example: atropine - has a higher activity than acetylcholine (an endogenous mediator). Atropine interacts with receptors, but since it has no internal activity, it will not cause a physiological effect. Due to the greater affinity for the receptor compared to acetylcholine, it will interfere with the action of the agonist, namely acetylcholine, and therefore be its antagonist.
Medicinal substances can act like or opposite to endogenous mediators. If a medicinal substance acts like a mediator (acetylcholine, norepinephrine, etc.), such a substance is called MIMETIC. Mim - the root "mime", pantomime, mimicry. Hence the cholinomimetic, adrenergic agonist.
A drug that prevents the interaction of a mediator with a receptor is called a blocker (anticholinergic, adrenergic blocker, histamine blocker, etc.).
In the literature, you can find the term "lytic" (lysis - dissolution, physical process). The term is rather old, but it is sometimes used (anticholinergic, adrenolytic). Thus, the terms "lytic" and "blocker" are used synonymously.
In medical practice, more and more wide application finds the simultaneous appointment of several drugs. At the same time, they can interact with each other, changing the severity and nature of the main effect, its duration, or weakening the side and toxic effects. In this regard, a special section of pharmacodynamics is devoted to the INTERACTION OF MEDICINES, which is classified as follows. Distinguish PHARMACOLOGICAL interaction and PHARMACEUTICAL interaction.
Pharmaceutical interactions are associated with pharmaceutical incompatibility of drugs during their manufacture or storage, as well as when mixed in one syringe. At the same time, the previously existing pharmacological activity of drugs decreases or disappears, and sometimes even new, toxic properties appear.
Pharmacological interaction of drugs is associated with changes in their pharmacokinetics, pharmacodynamics, or based on chemical and physicochemical interactions in the environments of the body. In this case, drugs can interact with each other at any stage of their passage through the patient's body: during absorption, in the transport phase, in the process of metabolism, as well as excretion (pharmacokinetic interaction).
Pharmacodynamic interaction reflects the change caused by each drug separately processes associated with the implementation of the effect. In other words, the pharmacodynamic type of interaction is based on the peculiarities of changes in the mechanisms and localization of the action of the drugs used, their main effects. If the interaction takes place at the receptor level, then it mainly concerns agonists and antagonists of various types of receptors. In this case, one medicinal substance can enhance or weaken the effect of another. If medicinal ve
The substances act in relation to the effect unidirectionally - these are synergistic drugs (syn - together, ergo - work). Thus, synergism is accompanied by an increase in the final effect. Typically, these drugs act on the same receptors. There are 2 variants of synergy:
1) The effects are the same on the principle of a simple sum. Summed up (or additive, - lat. - additio - addition). The effect is observed by simply adding the effects of each of the components. For example, this is how drugs for anesthesia interact (nitrous oxide + fluorothane). The variant of the additive effect is similar with the simultaneous use of aspirin and analgin. Why do you need to know this? If the patient is forced to take aspirin long time, then it should be taken into account that Aspirin acts ulcerogenically, that is, it causes ulceration of the gastrointestinal mucosa, and Analgin has such an undesirable effect as inhibition of hematopoiesis. Considering the additive analgesic effect, it is possible to reduce without significant risk of its occurrence, significantly reduce the dosage of both drugs taken by the patient.
2) The second version of synergy is potentiation or enhancement of the effect. This option occurs when, with the introduction of two substances, the total effect exceeds the sum of the effects of both agents. An example is the interaction of antipsychotics (chlorpromazine) and anesthetics, the interaction of antibiotics and antimicrobial sulfonylamides.
Sometimes the third (3) variant of synergism is distinguished - sensitization. Sensitization - when one drug in a minimum dose enhances the effect of another in their combination (the use of small doses of insulin in combination with KCl increases the level of potassium penetration into cells).
In addition to synergy, there is the phenomenon of antagonism. The ability of one substance to reduce the effect of another to one degree or another is called ANTAGONISM, that is, in this case, one drug prevents the action of the other.
There are physical, chemical and physiological antagonisms. This view interactions are most often used in case of overdose or acute drug poisoning. An example of PHYSICAL antagonism can be indicated by the ability of adsorbing agents to hinder the absorption of substances from digestive tract(activated carbon, which adsorbs poison on its surface; cholestyramine).
An illustration of the CHEMICAL interaction can be the formation of complexones (ions of some heavy metals - mercury, lead - bind penicylamine, EDTA), or this is how it interacts hydrochloric acid stomach and sodium bicarbonate (alkali).
PHYSIOLOGICAL antagonism is associated with drug interactions at the receptor level, the nature of which has already been discussed above.
By analogy with synergism, DIRECT (when both drug compounds act on the same receptors) and INDIRECT (different localization of drug action) antagonism are distinguished. In turn, direct antagonism is COMPETITIVE and NOT
COMPETITIVE. With competitive antagonism, the drug enters into a competitive relationship with natural regulators (mediators) for binding sites in specific receptors. Receptor blockade caused by a competitive antagonist can be relieved with high doses of an agonist or natural mediator.
Noncompetitive antagonism is a situation when a drug cannot displace a natural mediator from a receptor, but forms covalent bonds with it (mediator).
POINTS OF INTERACTION OF MEDICINES Main
the mass of receptors is located on the outer and inner sides of the cell membrane and its organelles. The most common points of drug interaction include: 1) mediators and hormonal receptors; 2) ATP-phase of the Na / K pump, Ca, K and Na - intramembrane channels.
The latter proves once again that drugs act on the available key mechanisms of biological reactions, that is, on phylogenetically determined processes, and not by creating some new reactions.
The interaction of drugs with the receptor occurs at the level of chemical or physicochemical processes. Most often, the nature of the reaction, its strength, reversibility and duration are due to the properties of the drug's connection with the receptor. The bond strength depends on the distance of electrostatic interaction between the two atoms. As a rule, the nature of the interaction is complex, it can involve different kinds connection, which is determined by the complementarity of the drug and the receptor, the degree of their convergence with each other.
The weakest bonds are van der Waals (determine the specificity of the interaction of substances with reactive systems). In most cases, ionic bonds arise between the drug and the receptor (reversible).
TYPES OF ACTION OF MEDICINES
1) LOCAL EFFECT - the action of a substance that occurs at the site of its application. Example: the use of local anesthetics - the introduction of a solution of dicaine into the conjunctival cavity. The use of a 1% solution of novocaine during extraction
tooth. This term (local action) is somewhat arbitrary, since a truly local action is observed extremely rarely, due to the fact that since substances can be partially absorbed, or have a reflex effect.
2) REFLECTIVE ACTION - this is when the drug acts on the pathways of the reflex, that is, it affects the extero- or interoreceptors and the effect is manifested by a change in the state of either the corresponding nerve centers or executive organs. So, the use of mustard plasters for pathology of the respiratory system improves their trophism reflexively (essential mustard oil stimulates the exteroreceptors of the skin). The drug cytiton (respiratory analeptic) has an exciting effect on the chemoreceptors of the carotid glomerulus and, by reflexively stimulating the center of respiration, increases the volume and frequency of respiration. Another example is the use of ammonia for fainting (ammonia), which reflexively improves
cerebral circulation and tonic vital centers.
3) RESORPTIVE ACTION - this is when the action of a substance develops after its absorption (resorption - absorption; Latin - resorbeo - I absorb), entering the general bloodstream, then into the tissues. Resorptive action depends on the route of administration of the drug and its ability to penetrate biological barriers. If a substance interacts only with functionally single-source receptors of a certain localization and does not affect other receptors, the action of such a substance is called SELECTIVE. So, some curariform substances (muscle relaxants) quite selectively block the end plate cholinergic receptors, causing skeletal muscle relaxation. The action of the drug prazosin is associated with a selective blocking of postsynaptic alpha-one adrenergic receptors, which ultimately leads to a decrease in blood pressure... The basis of the selectivity of the action of drugs (selectivity) is the affinity (affinity) of the substance to the receptor, which is determined by the presence of certain functional groups in the molecule of these substances and the general structural organization of the substance, which is most adequate for interaction with these receptors, that is, COMPLETENESS.
GENERAL CHARACTERISTIC OF THE EFFECT OF DRUGS ON THE BODY
Despite the abundance of medicines, all immense
caused by them in the body, have a certain commonality and
uniformity. Based on the concept of the reaction rate, there are 5
types of changes
caused by pharmacological agents (N.V. Vershinin):
1) toning (increasing the function to normal);
2) excitement (increased function above the norm);
3) sedative effect (sedative), that is, lowering enhanced function to the norm;
4) oppression (decrease in function below normal);
5) paralysis (termination of function). The amount of tonic and cart
an awakening effect is called an awakening action.
MAIN EFFECTS OF MEDICINES
First of all, there are:
1) physiological effects when drugs cause changes such as an increase or decrease in blood pressure, heart rate, etc.;
2) biochemical (increased levels of enzymes in the blood, glucose
Shl, etc.). In addition, there are BASIC (or main) and
SECONDARY (minor) effects of drugs. BASIC EF
FACT is the one on which the doctor bases his calculations in the treatment of this (!) Patient (analgesics - for an analgesic effect, antihypertensives - to lower blood pressure, etc.).
SUBSTANTIAL, or non-main effects, additional otherwise, those that are inherent this tool, but the development of which in this patient is not necessary (non-narcotic analgesics - in addition to the analgesic effect, they cause an antipyretic effect, etc.). Side effects may include ADVERSE and UNWANTED (or SIDE) effects.
Example. Atropine - relaxes the smooth muscles of the internal
organs. However, at the same time, it simultaneously improves the conduction in the AV node of the heart (with heart block), increases the diameter of the pupil, etc. All these effects must be considered individually in each case.
FACTORS AFFECTING THE VALUE OF THE EFFECT OF DRUGS
1) First of all, you need to remember about the pharmacokinetic factors inherent in each drug. This has already been mentioned above, I will only remind you that we are talking about its rate of absorption or absorption, biotransformation, excretion (drug, drug).
2) The second group of factors is physiological.
a) Age. Indeed, everyone is well aware that the patient's sensitivity to drugs changes with age. We stood out even in this regard:
Perinatal Pharmacology;
Pediatric Pharmacology;
Geriatric Pharmacology;
Reproductive Pharmacology;
b) The weight of the patient. It is known that the greater the mass, the higher
dose. Therefore, drugs are dosed in (mg / kg).
c) Gender. Revealed different sensitivity in men and women
certain substances, for example, nicotine, alcohol, etc.,
which is explained by the difference in metabolism, the difference in specific
body fat weight, etc.
c) The state of the organism. The effect of drugs on the body after su
physical exercise will be different than without it.
e) Biological rhythms(daily allowance, monthly, seasonal, year
vye, and now even population) have the most serious
influence on the action of drugs in the body. 3) Pathological facts
ry (for example, the level of hormonal activity). So with ba
toxic doses of morphine are more easily tolerated, but the sensitivity of the myocardium to adrenaline increases. 1 0 The effect of cardiac glycosides on blood circulation is manifested only against the background of heart failure. The effect of drugs changes significantly with hypo- and hyperthermia, with infectious diseases, with a change in the functional state of the central nervous system, etc.).
4) Genetic factors. It is known that the absence of the enzyme glucose-6-phosphate dehydrogenase (G-6-FDG) in thalassenia makes it impossible to prescribe antimalarial drugs such as primaquine. Deficiency of the enzyme butyrylcholinesterase in the blood, which occurs in one out of 2500 people, is the cause of prolonged muscle relaxation after the administration of ditilin.
5) The suggestibility of patients or placebo effect. In this regard, the antianginal effect of placebo drugs, for example, reaches 40%, and up to 81% of the placebo effect arises from the injection route of drug administration. This is probably why using vitamin preparations, tonics, tranquilizers are largely due to this effect.
6) The dose of the medicine. The effect of drugs is to a very large extent determined by their dose. Dose refers to the amount of medicinal substance
a single dose (usually referred to as a single dose). The dose of the drug depends not only on the effectiveness of treatment, but also on the safety of the patient. Back at the end of the 18th century, William Withering wrote: "Poison in small doses is the best medicine; a useful medicine in too large a dose is poison." This is all the more true in our time, when extremely active drugs have been introduced into medical practice, the dosages of which are measured in fractions of a milligram.
Indicate the dose in grams or fractions of a gram. For a more accurate dosage of drugs, their amount is calculated per 1 kg of body weight (or per 1 sq. M of body area), for example, 1 mg / kg; 1 mcg / kg, etc. The doctor needs to be oriented not only in the dose calculated for a single dose (pro dosi), but also in the daily dose (pro die).
The minimum doses in which drugs cause an initial biological (therapeutic) effect are called threshold, or minimum effective (therapeutic) doses. In practical medicine, average therapeutic doses are most often used, in which drugs have the necessary optimal pharmacotherapeutic effect. If, when prescribing them to the patient, the effect is not pronounced enough, the dose is increased to the highest therapeutic dose. Higher therapeutic doses can be single and daily. The highest single dose is the maximum amount of a drug that can be administered once without harm to the patient. These doses are rarely used, in extreme cases (in an urgent, emergency situation). Average therapeutic doses are usually 1 / 3-1 / 2 of the highest single dose.
Higher therapeutic doses of poisonous and potent substances are given in the State Pharmacopoeia of the USSR. In some cases, for example, when using chemotherapeutic agents, the dose of the drug is indicated for the course of treatment (course dose). If it becomes necessary to quickly create a high concentration of a drug in the body (sepsis, cardiovascular failure), then use the first dose, the so-called loading dose, which exceeds all subsequent ones. There are also toxic (dangerous effects) and lethal doses.
It is important for the doctor to know one more characteristic - namely, the concept of the breadth of the therapeutic action of the drug. The breadth of therapeutic action is understood as the distance, the range from the minimum therapeutic dose to the minimum toxic dose. Naturally, the greater this distance, the safer this drug is.
1/20 of the dose x the number of years of the child.
To quantitatively characterize and evaluate the effectiveness of a new pharmacological agent, two standard comparisons are usually used - either with a placebo or with an analo drug.
gic type of action, which is one of the most effective means in this group.
A placebo (dummy) is an indifferent substance in a dosage form that mimics a certain pharmacological or drug. The use of a placebo is necessary in the presence of: a) the effect of presumptiveness, influence of personality, expectation and bias by the patient or researcher; b) spontaneous changes in the course of the disease, symptoms, as well as phenomena not related to treatment.
Placebo is a Latin term meaning "I can please you."
The placebo effect is an effect caused not by the specific pharmacodynamic properties of a drug for a given pathology, but by the FACT OF USE of drugs, which affects psychologically. Placebo drugs are usually pharmacologically inert and contain inactive substances like starch or lactose. Placebos are used in clinical trials to determine the effect of suggestion on the part of both the patient and the doctor, especially if the drugs intended for treatment are to be studied. bronchial asthma, hypertension, angina pectoris, ischemic heart disease. In such cases, the placebo drug should not be in color or otherwise physical properties(smell, taste, shape) differ from the active preparation. A placebo is more effective when both the doctor and the patient are poorly informed about it.
EXAMPLE. At ischemic disease heart disease (IHD) if one group of patients with IHD is prescribed an active drug, and the other - a placebo, then in 40% of patients in the second group, angina attacks are stopped.
Most pronounced effect placebo (up to 81%) is observed with the injection route of its administration. Potions and pills are less effective.
The term PHARMACOTHERAPY (FT) is often used in the literature on patient drug exposure. Pharmacotherapy is a section of pharmacology that studies drug therapy of a patient.
Distinguish the following types pharmacotherapy:
1) ETIOTROPIC - perfect view pharmacotherapy. This type of FT is aimed at eliminating the cause of the disease. Examples of etiotropic PT can be the treatment of infectious patients with antimicrobial agents (benzylpenicillin for streptococcal pneumonia), the use of antidotes in the treatment of patients with toxic
substances. 2) PATHOGENETIC PHARMACOTHERAPY - directed
to eliminate or
suppression of the mechanisms of the development of the disease. Most of the currently used drugs belong specifically to the group of drugs of pathogenetic FT. Antihypertensive drugs, cardiac glycosides, antiarrhythmic, anti-inflammatory, psychotropic and many other drugs have a therapeutic effect by suppressing the corresponding mechanisms of the development of the disease.
3) SYMPTOMATIC THERAPY - aimed at eliminating or
limitation of individual manifestations of the disease. Symptomatic drugs include pain relievers that do not affect the cause or mechanism of the disease. Antitussives are also a good example of symptomatic remedies. Sometimes these remedies (elimination pain syndrome with myocardial infarction) can have a significant effect on the course of the main pathological process and at the same time play the role of means of pathogenetic therapy.
4) SUBSTITUTIONAL PHARMACOTHERAPY is used in case of deficiency of natural nutrients. Replacement therapy means include enzyme preparations (pancreatin, panzinorm, etc.), hormonal drugs (insulin for diabetes mellitus, thyroidin for myxedema), vitamin preparations (vitamin D, for example, for rickets). Substitution therapy drugs, without eliminating the causes of the disease, can ensure the normal existence of the body for many years. It is no coincidence that such a severe pathology as diabetes- is considered a special lifestyle among Americans.
5) PREVENTIVE THERAPY is carried out to prevent diseases. Some are preventive antiviral agents(for example, during a flu epidemic - remantadine), disinfectants and a number of others. The use of anti-tuberculosis drugs such as isoniside can also be considered prophylactic FT. A good example carrying out preventive therapy is the use of vaccines.
CHEMOTHERAPY should be distinguished from pharmacotherapy. If FT deals with two participants in a pathological process, namely, a drug and a macroorganism, then during chemotherapy there are already 3 participants: a drug, a macroorganism (patient) and a causative agent of the disease.
Speaking of doses, we first of all had to point to allopathic doses, as opposed to homeopathic ones. Therefore, a few words about HOMEOPATHY. The term "homeopathy" is derived from two Greek words: homois - similar and pathos - suffering, illness. Literally, homeopathy is translated as a similar, similar disease. The founder of homeopathy, the German scientist Samuel Hahnemann, in his famous book "The Organon of the Art of Medicine or the Basic Theory of Homeopathic Treatment" back in early XIX century (1810) outlined the basic principles of this science. There are several principles, but 2 of them are basic:
1) This is the law of similarity, which states that the treatment of diseases must be carried out with a similar, similar means. According to this principle, Hahnemann advises "to imitate nature, which sometimes heals a chronic disease through another concomitant disease." Therefore, "against a disease to be cured (mainly chronic), one should use such a medicinal substance that is able to cause another, the most similar artificial disease, and the first one will be cured." Similia
similibus (like like). For example, jaundice should be treated with yellow, etc.
2) The second principle is to treat with super small doses. Dilutions of medicines used by homeopaths are counted in several orders of magnitude, sometimes reaching dozens of them: 10 in the fifth; 10 in the tenth; 10 to the eighteenth or more power (that is, million
and more than a fraction of grams). To explain the effect of using le
carbohydrate substances in
high dilutions Hahnemann put forward a speculative concept: "Small doses are distinguished by a special spiritual strength, greater activity, the ability to penetrate into the affected organs and tissues."
It is not known what about special spiritual power, but scientific life in the last decade has presented very strong evidence for the validity of Hahnemann's statement. So, for example, the experiments of the Frenchman Jacques Bekveniste, made by him with a dilution of substances 10 to the eightieth power, showed that water molecules have a "memory" for the presence of a given substance, causing a certain physiological effect. If this fact noted in the near future finds confirmation, that is, if it is established whether water molecules are a source of information, we will undoubtedly stand at the foundations of the greatest discovery that can explain the therapeutic efficacy of homeopathic remedies.
Next, consider the section concerning the PHARMACOLOGICAL ASPECTS OF THE TOXIC EFFECT OF DRUGS, namely the TOXICOLOGY OF DRUGS. Drug toxicology is a branch of pharmacology that studies the toxic effects of these drugs. However, now it is more correct to talk about adverse reactions the human body for medicines. This fact has been known for a long time, a wealth of factual material has been accumulated indicating that undesirable reactions varying degrees can occur with almost all medications.
There are many classifications of drug side effects and pharmacotherapy complications, although none are perfect. At the same time, based on the pathogenetic principle, all undesirable effects or reactions can be divided into 2 types:
1) adverse reactions associated with
a) drug overdose
b) poisoning;
2) toxic reactions associated with the pharmacological properties of drugs.
Overdose usually occurs when using high doses of drugs. Especially often, an overdose occurs when taking medications with a small latitude of therapeutic action. For example, toxicity is difficult to avoid when using aminoglycoside antibiotics (streptomycin, kanamycin, neomycin). These drugs cause vestibular disorders and deafness when treated in doses that are not much higher than therapeutic. For some drugs, it is simply impossible to avoid toxic complications (antineoplastic, cytotoxic drugs), which damage all rapidly dividing cells and
the inert brain does not disappear while effectively affecting the growth of tumor cells.
In addition, overdose can be associated not only with the use of high doses, but also with the phenomenon of cumulation (cardiac glycosides).
Poisoning can be accidental or deliberate. Intentional poisoning usually occurs with a suicidal purpose (with the aim of suicide). In the Omsk region, most often in general structure poisoning is occupied by cauterizing liquid poisoning, in second place are drug poisoning. These are, first of all, poisoning with sleeping pills, tranquilizers, FOS, alcohol, carbon monoxide.
Despite the difference in etiological factors, the measures of assistance at the stages of medical treatment are fundamentally similar.
These principles are as follows:
1) FIGHT WITH UNSUNGED POISON FROM THE GASTROINTESTINAL TRACT. This is most often required for oral poisoning. Most often acute poisoning is caused by ingestion of substances. A mandatory and urgent measure in this regard is gastric lavage through a tube even 10-12 hours after poisoning. If the patient is conscious, gastric lavage is carried out using a large number water and subsequent induction of vomiting. Induce vomiting mechanically... In an unconscious state, gastric lavage is carried out to the patient through a probe. It is necessary to direct efforts to adsorb the poison in the stomach, for which activated charcoal is used (1 tablespoon inside, or 20-30 tablets at the same time, before and after gastric lavage). The stomach is washed several times after 3-4 hours until it is completely cleared of the substance.
Vomiting is contraindicated in the following cases:
With coma;
In case of poisoning with corrosive liquids;
In case of poisoning with kerosene, gasoline (the possibility of hydrocarbonate pneumonia with necrosis lung tissue etc.).
If the victim is a small child, then it is better to use saline solutions in small volumes (100-150 ml).
It is best to remove poison from the intestines with the help of saline laxatives. Therefore, at the end of the lavage, 100-150 ml of a 30% sodium sulfate solution, and even better magnesium sulfate, can be introduced into the stomach. Saline laxatives are the most powerful, fast acting laxatives throughout the intestines. Their action obeys the laws of osmosis, therefore, they cease the action of the poison within a short period of time.
It is good to give astringents (tannin solutions, tea, bird cherry), as well as enveloping ones (milk, egg white, vegetable oil).
In case of skin contact with poison, it is necessary to thoroughly rinse the skin, preferably with cork water. If toxic substances enter through the lungs, their inhalation should be stopped by removing the victim from the poisoned atmosphere.
With the subcutaneous injection of a toxic substance, its absorption from the injection site can be slowed down by injections of an adrenaline solution
around the injection site, as well as cooling this area (ice on the skin at the injection site).
2) The second principle of assistance in acute poisoning is to influence the absorbed poison, REMOVING IT FROM THE BODY.
In order to remove the toxic substance from the body as soon as possible, forced diuresis is used first of all. The essence of this method lies in the combination of increased water load with the introduction of active, powerful diuretics. The body is flooded by drink plenty of water to the patient or intravenous administration of various solutions (blood substitute solutions, glucose, etc.). Of the diuretics, FUROSEMIDE (lasix) or MANNIT are most often used. By the method of forced diuresis, we kind of "wash" the patient's tissues, freeing them from the toxic substance. This method only manages to remove only free substances that are not associated with proteins and blood lipids. Consideration should be given to the electrolyte balance, which when using this method can be impaired due to the excretion of a significant amount of ions from the body.
In acute cardiovascular failure, severe renal dysfunction and the risk of developing cerebral or pulmonary edema, forced diuresis is contraindicated.
In addition to forced diuresis, hemodialysis and peritoneal dialysis are used, when blood (hemodialysis, or an artificial kidney) passes through a semipermeable membrane, freeing itself from toxic substances, or "washing" of the peritoneal cavity with an electrolyte solution is carried out.
EXTRACORPORAL DETOXIFICATION METHODS. A successful method of detoxification, which has become widespread, is the method of HEMOSORPTION (lymphosorption). In this case, toxic substances in the blood are adsorbed on special sorbents (granular carbon coated with blood proteins, allo spleen). This method allows you to successfully detoxify the body in case of poisoning with neuroleptics, tranquilizers, FOS, etc. The hemosorption method removes substances that are poorly removed by hemodialysis and peritoneal dialysis.
BLOOD SUBSTITUTION is used when bleeding is combined with donor blood transfusion.
3) The third principle of the fight against acute poisoning is the DISHARMING OF THE SUCKED POISON by the introduction of ANTAGONISTS and ANTIDOTES.
Antagonists are widely used in acute poisoning. For example, atropine for anticholinesterase poisoning, FOS; nalorphine - in case of poisoning with morphine, etc. Usually pharmacological antagonists competitively interact with the same receptors as the substances that caused the poisoning. In this regard, the creation of SPECIFIC ANTIBODIES (monoclonal) in relation to substances that are especially often the cause of acute poisoning (monoclonal antibodies against cardiac glycosides) looks very interesting.
For the specific treatment of patients with chemical poisoning, ANTIDOTE THERAPY is effective. ANTIDOTES are the means used for the specific binding of poison, neutral
licking, inactivating poisons, either through chemical or physical interaction.
So, in case of poisoning with heavy metals, compounds are used that form non-toxic complexes with them (for example, unitiol for arsenic poisoning, D-penicylamine, desferal for poisoning with iron preparations, etc.).
4) The fourth principle is to carry out SYMPTOMATIC THERAPY. Especially great importance symptomatic therapy is acquired in case of poisoning with substances that do not have special antidotes.
Symptomatic therapy supports vital functions: CIRCULATION and RESPIRATION. They use cardiac glycosides, vasotonics, agents that improve microcirculation, oxygen therapy, and respiratory stimulants. Convulsions are eliminated by injections of sibazon. With cerebral edema, dehydration therapy (furosemide, mannitol) is performed. use analgesics, correct the acid-base state of the blood. When breathing stops, the patient is transferred to artificial ventilation lungs with a complex of resuscitation measures.
Next, we will focus on the SECOND TYPE of ADVERSE REACTIONS, that is, adverse reactions associated with the pharmacological properties of drugs. Side effects of drugs are manifested in 10-20% of outpatients, and 0.5-5% of patients require hospitalization to correct disorders from drugs. These undesirable, from the point of view of pathogenesis, reactions can be: a) DIRECT and b) associated with the CHANGED SENSITIVITY of the patient's body.
Let us examine DIRECT TOXIC REACTIONS. They are called direct because drugs directly, directly toxic functional system... For example, antibiotics of the aminoglycoside series (streptomycin, kanamycin, gentamicin) exhibit NEUROTOXICITY, exerting a toxic effect on the hearing organ (ototoxicity) and the vestibular apparatus. Besides this class antibiotics have toxicity in relation to behavioral reactions, manifested by lethargy, apathy, lethargy, drowsiness.
Medicines can have DIRECT GLATOTOXIC REACTIONS. For example, fluorothane (anesthetic agent) with repeated applications in short time can have a pronounced toxic effect up to acute yellow dystrophy of the liver.
Direct toxic effects can be realized by NEPHROTOXICITY. This effect is possessed by mycin antibiotics-aminoglycosides. When prescribing drugs of this series, the patient needs constant monitoring of the state of urine tests (protein, blood in the urine, etc.).
The next direct toxic effect is ULTSEROGENIC (ulcerative). For example, the appointment of salicylates, glucocorticoids, the antihypertensive agent reserpine - leads to ulceration of the gastric mucosa, which must be taken into account when prescribing these classes of drugs, especially for patients already suffering from peptic ulcer disease.
Direct toxic effects can be expressed in EMBRYOTOXICITY. Let me remind you that embryotoxic is called an unfavorable
the effect of drugs, not associated with a violation of organogenesis, which occurs before 12 weeks of pregnancy. And the toxic effect of drugs in the later period of pregnancy is called FETOTOXIC. It is necessary to remember about this effect when prescribing medicines for pregnant women, conducting pharmacotherapy for them only according to strict indications.
Examples: 1) the appointment of streptomycin to pregnant women can lead to deafness in the fetus (damage to the VIII pair of cranial nerves); 2) tetracyclines adversely affect the development of bones in the fetus; 3) in a mother suffering from morphinism, the newborn may also be physically addicted to morphine.
Medicines can have TERATOGENICITY, that is, such a damaging effect on the differentiation of tissues and cells, which leads to the birth of children with various anomalies. For example, the use of TALIDOMIDE as a sedative and hypnotic, which has a pronounced teratogenic effect, has led to the birth in countries Western Europe several thousand children with various deformities (phocomelia - flipper-like limbs; amelia - absence of limbs; facial hemangions, gastrointestinal anomalies).
To study the teratogenic effect of substances, the effect of drugs on animals is investigated, although there is no direct correlation on the effect of drugs on animals and humans. For example, in the same thalidomide, teratogenicity in an experiment on mice was detected at a dose of 250-500 mg / kg of body weight, while in humans it was equal to 1-2 mg / kg.
The most dangerous in relation to teratogenic action is the first trimester (especially the period of 3-8 weeks of pregnancy), that is, the period of organogenesis. During these periods, it is especially easy to cause a severe anomaly in the development of the embryo.
When creating new drugs, one should also keep in mind the possibility of such serious negative effects as CHEMICAL MUTAGENCY and CARCINOGENICITY. MUTAGENCY is the ability of substances to cause permanent damage to the germ cell, but especially to its genetic apparatus, which manifests itself in a change in the genotype of the offspring. CARCINOGENICITY is the ability of substances to induce the development of malignant tumors... Estrogens contribute to the development of breast cancer in women of childbearing age.
Mutagenic and teratogenic effects can appear months or even years later, which makes it difficult to identify their true activity. Teratogenicity is inherent in antineoplastic drugs, corticosteroids, androgens, alcohol. Cyclophosphamide and some hormonal agents have a carcinogenic effect.
Adverse reactions when using drugs can be expressed by the development of DRUG DEPENDENCE or, more globally, DRUG ADDICTION. There are several main signs of addiction.
1) This is the presence of MENTAL DEPENDENCE, that is, such a state when the patient develops an irresistible mental attraction to the repeated administration of a medicinal substance, for example,
drug.
2) PHYSICAL DEPENDENCE - this term denotes the presence of severe physical ailment in a patient without repeated injection of a medicinal substance, in particular a drug. With an abrupt cessation of the administration of the drug that caused drug dependence, the phenomenon of DEPRIVATION or ABSTINENCE develops. Fear, anxiety, melancholy, insomnia appear. Perhaps motor restlessness, aggressiveness arises. Many physiological functions are impaired. In severe cases, withdrawal symptoms can be fatal.
3) Development of TOLERANCE, that is, addiction. Other species
The undesirable effects caused by the properties of the drugs themselves are disorders associated with shifts in the patient's immunobiological system when taking highly active drugs. For example, the use of broad-spectrum antibiotics can be manifested by a change in the normal bacterial flora of the body (intestines), realized by the development of superinfection, dysbiosis, candidiasis. Most often, the lungs and intestines are involved in these processes.
Corticosteroid and immunosuppressive therapy weaken the immune system, resulting in an increased risk of developing infectious diseases, first of all, of an opportunistic nature (pneumocystosis, cytomegalovirus, etc.).
This subgroup of reactions is of 2 types:
1) ALLERGIC REACTIONS;
2) Idiosyncrasy. It should be said that negative influences
related to
chemical reactions are very common in medical practice. Their frequency is increasing all the time. They arise regardless of the dose of the administered drug, and immune mechanisms are involved in their formation. Allergic reactions can be of 2 types: HYPERSENSITIVITY OF IMMEDIATE TYPE, HNT - associated with the formation of antibodies of the IgE and IgG4 classes) and SLOW (accumulation of sensitized T-lymphocytes and macrophages) types.
The clinical picture is very diverse: urticaria, skin rashes, angioedema, serum sickness, bronchial asthma, fever, hepatitis, etc. But the main thing is the possibility of developing anaphylactic shock. If the development of allergic reactions requires at least two contact of the patient with a drug, then the development of IDIOSYNCRASIA - intolerance to drugs during initial contact with a xenobiotic, is always associated with some kind of GENETIC DEFECT, usually expressed by the absence or extremely low activity of the enzyme. For example, the use of the antimalarial drug primaquine in individuals with genetic enzymopathy (deficiency of act. G-6-FDG) causes the formation of quinone, which has a hemolytic effect. In the presence of this fermentopathy, it is dangerous to prescribe drugs that are oxidizing agents, as this can lead to hemolysis
erythrocytes, drug hemolytic anemia (aspirin, chloramphenicol, quinidine, primaquine, furadonin).
A FEW WORDS ABOUT THE CREATION OF NEW DRUGS, THE EVALUATION OF DRUGS AND THEIR NOMENCLATURE. The progress of pharmacology is characterized by the continuous search and creation of new drugs. Drug creation begins with research by chemists and pharmacologists, whose creative collaboration is absolutely essential when discovering new drugs. At the same time, the search for new funds is developing in several directions.
The main way is CHEMICAL synthesis of drugs, which can be realized in the form of DIRECTED synthesis or have an EMPIRICAL way. If directed synthesis is associated with the reproduction of biogenic substances (insulin, adrenaline, norepinephrine), the creation of antimetabolites (PABA-sulfonamides), the modification of molecules of compounds with known biological activity (a change in the structure of acetylcholine - gongliobacter hygronium), etc., then the empirical path consists either from random finds, or search by screening, that is, sifting various chemical compounds for pharmacological activity.
One of the examples of empirical findings can be the case of the obstruction of the hypoglycemic effect when using sulfonamides, which subsequently led to the creation of synthetic sulfonamide perforal antidiabetic agents (butamide, chlorpropamide).
Another variant of the empirical way of creating drugs, the SCREENING METHOD, is also very laborious. However, it is inevitable, especially if investigated new class chemical compounds, the properties of which, based on their structure, are difficult to predict (ineffective way). And here huge role computerization of scientific research is currently playing.
Currently, drugs are obtained mainly through directed chemical synthesis, which can be carried out a) by similarity (introduction of additional chains, radicals) b) by complementarity, that is, by correspondence to any receptors of tissues and organs.
In the arsenal of drugs, in addition to synthetic drugs, a significant place is occupied by drugs and individual substances from medicinal raw materials of plant or animal origin, as well as from various minerals. These are primarily galenic, novogalenic drugs, alkaloids, glycosides. So morphine, codeine, papaverine are obtained from opium, reserpine is obtained from serpentine serpentine, and cardiac glycosides - digitoxin, digoxin - are obtained from foxglove; from a number of endocrine glands of cattle - hormones, immunoactive drugs (insulin, thyroidin, taktivin, etc.).
Some medicines are waste products of fungi and microorganisms. An example is antibiotics. Medicinal substances of plant, animal, microbial, fungal origin often serve as the basis for their synthesis, as well as subsequent chemical transformations and the production of semi-synthetic and synthetic drugs.
The pace of drug development is gaining momentum by using
the development of genetic engineering methods (insulin, etc.).
A new drug, after passing through all these "sieves" (study of pharmacological activity, pharmacodynamics, pharmacokinetics, study of side effects, toxicity, etc.) is allowed for clinical trials. It uses the "blind control" method, the placebo effect, the double "blind control" method, when neither the doctor nor the patient knows when this placebo is used. Only the special commission knows. Clinical trials are carried out in humans, and in many countries they are carried out on volunteers. Here, of course, a lot of legal, deontological, moral aspects of the problem arise, which require their clear development, regulation and approval of laws in this regard.
NOMENCLATURE OF MEDICINES
Many drugs that are composed of a single active substance can be named for their chemical structure. But due to the great complexity of their memorization and the inconvenience of their use, chemical names are not used in medical practice.
Currently, 2 types of names are used to designate medicines:
1) NON-PATENTED international, which are approved by official health authorities and used in national and international pharmacopoeias;
2) COMMERCIAL, or brand names that are the commercial property of pharmaceutical companies. Moreover, one and the same drug can have many names. The tranquilizer diazenam has the brand names "seduxen", "sibazon", "relanium", etc. Some drugs have more than 100 names (for example, vitamin B12). Typically, a drug product has both the brand name and the international non-proprietary name on the package.
Generic prescribing of drugs is preferred, which reduces the possibility of medical errors... These drugs are cheaper than brand name drugs. In addition, prescribing drugs under their generic name enables a pharmacy to provide a patient with a drug from any company that manufactures this drug.
For clinicians, the most convenient classification of drugs is the one that is based on the NOSOLOGICAL PRINCIPLE (for example, drugs for the treatment of bronchial asthma, myocardial infarction, antidiabetic drugs, etc.). But best classifications take into account such signs of drugs as localization of action, pharmacological action, therapeutic use... One of such classifications, which is the most perfect, is the classification of Academician M.D. Mashkovsky, according to which his well-known reference book is also presented.
1. The concept of treatment as directed correction of physiological disorders in the body. The benefits and risks of using medications. The grounds for their application. Safety assessment.
Pharmacology- the theoretical basis of pharmacotherapy.
Reasons for using drugs:
1) to correct and eliminate the cause of the disease
2) in case of insufficient preventive measures
3) for health reasons
4) obvious need based on level of knowledge and experience
5) striving to improve the quality of life
Benefits in prescribing medications:
1) correction or elimination of the cause of the disease
2) relief of symptoms of the disease if it is impossible to treat it
3) substitution of medicinal substances for natural biologically active substances, not produced by organisms in sufficient quantities
4) implementation of disease prevention (vaccines, etc.)
Risk- the likelihood that harm or damage will result from exposure; is equal to the ratio of the number of adverse (aversive) events to the size of the risk group.
A) unacceptable (harm> benefit)
B) acceptable (benefit> harm)
B) insignificant (105 - security level)
D) conscious
Drug safety assessment starts at the level chemical laboratories synthesizing drugs. The preclinical assessment of drug safety is carried out by the Ministry of Health, FDA, etc. If the drug is successfully passed this stage, its clinical assessment begins, consisting of four phases: phase I - assessment of tolerance on healthy volunteers 20-25 years old, phase II - on sick volunteers of less than 100 people suffering from a specific disease, phase III - multicenter clinical trials on large groups of people ( up to 1000 people), IV phase - monitoring of the drug for 5 years after its official approval. If a drug successfully passes all of these phases, it is considered safe.
2. The essence of pharmacology as a science. Sections and fields of modern pharmacology. The main terms and concepts of pharmacology are pharmacological activity, action, effectiveness of chemicals.
Pharmacology- the science of medicines in all aspects - the theoretical basis of therapy:
A) the science of the interaction of chemicals with living systems
B) the science of managing the vital processes of the body with the help of chemicals.
Sections of modern pharmacology:
1) Pharmacodynamics- studies a) the effect of drugs on the human body, b) the interaction of various drugs in the body while prescribing them, c) the effect of age and various diseases on the effect of drugs
2) Pharmacokinetics- studies the absorption, distribution, metabolism and excretion of drugs (i.e., how the patient's body reacts to drugs)
3) Pharmacogenetics- studies the role of genetic factors in the formation of the body's pharmacological response to drugs
4) Pharmacoeconomics- evaluates the results of use and the cost of drugs for making a decision on their subsequent practical use
5) Pharmacoepidemiology- studies the use of drugs and their effects at the level of populations or large groups of people to ensure the use of the most effective and safe drugs
Pharmacological (biological) activity- the property of a substance to cause changes in the biosystem (human body). Pharmacological substances = biologically active substances (BAS)
pharmachologic effect- the influence of drugs on the object and its targets
Pharmacological effect- the result of the action of a substance in the body (modification of physiological, biochemical processes, morphological structures) - a quantitative, but not qualitative change in the state of biosystems (cells, tissues, organs).
The effectiveness of drugs- the ability of drugs to cause certain pharmacological effects necessary in this case in the body. Assessed on the basis of "substantial evidence" - adequate well-controlled studies and clinical trials conducted by experts with appropriate scientific training and experience in drug research of this type (FDA)
3. The chemical nature of drugs. Factors providing the therapeutic effect of drugs are pharmacological action and placebo effects.
There are drugs 1) vegetable 2) animal 3) microbial 4) mineral 5) synthetic
Synthetic drugs are represented by almost all classes of chemical compounds.
pharmachologic effect- the influence of drugs on the object and its targets.
Placebo- any component of therapy that does not have any specific biological effect on the disease being treated.
It is used for the purpose of control when assessing the effect of drugs and in order to benefit the patient without any pharmacological agents as a result of only psychological influence (i.e. Placebo effect).
All types of treatment have a psychological component, or a satisfying one ( Placebo effect) or disturbing ( Nocebo effect). An example of a placebo effect: a rapid improvement in a patient with a viral infection when using antibiotics that do not affect viruses.
The benefit of the placebo effect is related to the psychological impact on the patient. It will be maximum only when using it. Combined with therapies that have a pronounced specific effect. Expensive substances as a placebo also help to achieve a greater response.
Indications for placebo use:
1) weak mental disorders
2) psychological support for a patient with an incurable chronic disease or suspected of having a difficult diagnosis
4. Sources and stages of drug creation. Definition of the concepts of medicinal substance, medicinal product, medicinal product and dosage form. The name of the drugs.
Sources of drug creation:
A) natural raw materials: plants, animals, minerals, etc. (cardiac glycosides, pork insulin)
B) modified natural biologically active substances
B) synthetic compounds
D) genetic engineering products (recombinant insulin, interferons)
Stages of drug creation:
1. Synthesis of drugs in a chemical laboratory
2. Preclinical assessment of the activity and undesirable effects of drugs of the Ministry of Health and other organisms
3. Clinical trials of drugs (for more details see section 1)
Medicine- any substance or product used to modify or investigate physiological systems or pathological conditions for the benefit of the recipient (according to WHO, 1966); individual substances, mixtures of substances or compositions of unknown composition with proven medicinal properties.
Medicinal substance- an individual chemical compound used as a medicine.
Dosage form- a convenient form for practical use, given to a drug to obtain the required therapeutic or prophylactic effect.
Medicinal product- a medicinal product in a specific dosage form, approved by a government authority.
5. Ways of introducing drugs into the body and their characteristics. Presystemic elimination of drugs.
1. For systemic action
BUT. Enteral route of administration: oral, sublingual, buccal, rectal, tube
B. Parenteral route of administration: intravenous, subcutaneous, intramuscular, inhalation, subarachnoid, transdermal
2. For local exposure: cutaneous (epicutary), on mucous membranes, in the cavity (abdominal, pleural, articular), in tissue (infiltration)
|
Route of drug administration |
Advantages |
Flaws |
|
Orally - by mouth |
1. Convenient and easy for the patient 2. Sterility of drugs is not required |
1. The absorption of many drugs depends on food intake, the functional state of the gastrointestinal tract and other factors that are hardly taken into account in practice 2. Not all drugs are well absorbed in the digestive tract 3. Some drugs are destroyed in the stomach (insulin, penicillin) 4. Part of the drug has NLR on the gastrointestinal mucosa (NSAIDs - mucosal manifestations, antacids - suppress motor skills) 5. Not applicable for patients in an unconscious state and with impaired swallowing |
|
Sublingual and buccal |
1. Convenient and quick introduction 2. Fast absorption of drugs 3. The drug is not subject to presystemic elimination 4. The action of the drug can be quickly interrupted |
1. Inconvenience caused by frequent regular use of pills 2. Irritation of the oral mucosa, excessive salivation, facilitating the swallowing of drugs and reducing its effectiveness 3. Bad taste |
|
Rectally |
1. Half of the drugs are not subject to presystemic metabolism 2. The gastrointestinal mucosa is not irritated 3. Convenient when other routes of administration are unacceptable (vomiting, seasickness, babies) 4. Local action |
1. Unpleasant psychological moments for the patient 2. The absorption of drugs is significantly slowed down when the rectum is not emptied. |
|
Intravascular (usually intravenous |
1. Fast admission into the blood (emergency conditions) 2. Rapid creation of high systemic concentration and the ability to manage it 3. Allows the introduction of drugs that are destroyed in the gastrointestinal tract |
1. Technical difficulties of intravascular access 2. Risk of infection at the injection site 3. Vein thrombosis at the injection site of drugs (erythromycin) and pain(potassium chloride) 4. Some drugs are adsorbed on the walls of droppers (insulin) |
|
Intramuscularly |
Sufficiently fast absorption of the drug into the blood (10-30 min) |
Risk of local complications |
|
Subcutaneously |
1. The patient can inject independently after training. 2. Long-term effect of drugs |
1. Slow absorption and manifestation of the drug effect 2. Atrophy of adipose tissue at the injection site and a decrease in the rate of absorption of drugs |
|
Inhalation |
1. Quick start action and high concentration at the injection site in the treatment of respiratory diseases. ways 2. Good controllability of the action 3. Reduction of toxic systemic effects |
1. The need for a special device (inhaler) 2. Difficulty using pressurized aerosols for some patients |
|
Local PM |
1. High effective concentration of drugs at the injection site 2. Undesirable systemic effects of this drug are avoided |
If the integrity of the skin is violated, the drug can enter the systemic circulation - a manifestation of undesirable systemic effects. |
Presystemic elimination of drugs (first pass effect)- the process of biotransformation of the drug before the drug enters the systemic circulation. Enzymatic systems of the intestine, portal vein blood and hepatocytes are involved in presystemic elimination with oral administration of the drug.
When administered intravenously, there is no presystemic elimination.
In order for an orally administered drug to have useful action, it is necessary to increase its dose to compensate for losses.
6. Transport of drugs across biological barriers and its varieties. The main factors affecting the transport of drugs in the body.
Ways of absorption (transport) of drugs through biological membranes:
1) Filtration (water diffusion) - passive movement of molecules of a substance along a concentration gradient through pores filled with water in the membrane of each cell and between neighboring cells, typical for water, some ions, small hydrophilic molecules (urea).
2) Passive diffusion (lipid diffusion) is the main mechanism of drug transfer, the process of drug dissolution in membrane lipids and movement through them.
3) Transport with the help of specific carriers - the transfer of drugs with the help of carriers built into the membrane (usually proteins), is characteristic of hydrophilic polar molecules, a number of inorganic ions, sugars, amino acids, pyrimidines:
a) facilitated diffusion - carried out along the concentration gradient without the consumption of ATP
b) active transport - against the concentration gradient with the costs of ATP
Saturable process - that is, the rate of absorption increases only until the number of drug molecules becomes equal to the number of carriers.
4) Endocytosis and pinocytosis - the drug binds to a special recognizing component of the cell membrane, membrane invagination occurs and a vesicle is formed containing drug molecules. Subsequently, the drug is released from the vesicle into the cell or transported out of the cell. Typical for high molecular weight polypeptides.
Factors affecting the transport of drugs in the body:
1) physical and chemical properties of the substance (hydro- and lipophilicity, ionization, polarizability, molecular size, concentration)
2) structure of transfer barriers
3) blood flow
7. Transport through membranes of medicinal substances with variable ionization (Henderson-Hasselbalch ionization equation). Transfer control principles.
All drugs are weak acids or weak bases with their own values of the ionization constant (pK). If the pH value of the medium is equal to the pK value of the drug, then 50% of its molecules will be in the ionized state and 50% in the non-ionized state, and the medium for the drug will be neutral.
In an acidic environment (pH less than pK), where there is an excess of protons, the weak acid will be in the undissociated form (R-COOH), that is, it will be associated with a proton - protonated. This form of acid is uncharged and readily soluble in lipids. If the pH is shifted to the alkaline side (i.e., the pH becomes greater than pK), then the acid will begin to dissociate and lose a proton, passing into a non-protonated form, which has a charge and is poorly soluble in lipids.
In an alkaline medium, where there is a deficiency of protons, the weak base will be in the undissociated form (R-NH2), that is, it will be unprotonated and devoid of charge. This form of base is highly lipid soluble and rapidly absorbed. In an acidic medium, there is an excess of protons and the weak base will begin to dissociate, while binding the protons and forming the protonated, charged form of the base. This form is poorly soluble in lipids and poorly absorbed.
Consequently, The absorption of weak acids takes place mainly in an acidic medium, and of weak bases in an alkaline medium.
Features of the metabolism of weak acids (SC):
1) stomach: SA in the acidic contents of the stomach is non-ionized, and in the alkaline medium of the small intestine it will dissociate and the SA molecules will acquire a charge. Therefore, absorption of weak acids will be most intense in the stomach.
2) in the blood, the medium is sufficiently alkaline and the absorbed SC molecules will transform into an ionized form. The renal glomerulus filter allows both ionized and non-ionized molecules to pass through, therefore, despite the charge of the molecule, SCs will be excreted into the primary urine
3) if the urine is alkaline, then the acid will remain in an ionized form, will not be able to reabsorb back into the bloodstream and will be excreted in the urine; If urine is acidic, then the medicine will go into a non-ionized form, which is easily reabsorbed back into the bloodstream.
Features of the metabolism of weak bases: opposite to SC (absorption is better in the intestine; in alkaline urine they are reabsorbed)
That., To accelerate the elimination of a weak acid from the body, urine must be alkalized, and to accelerate the elimination of a weak base, it must be acidified (detoxification according to Popov).
The quantitative dependence of the drug ionization process at different pH of the medium allows one to obtain the equation Henderson— Hasselbach:
Where pKa corresponds to the pH value at which the concentrations of the ionized and non-ionized forms are in equilibrium .
The Henderson-Hasselbach equation makes it possible to estimate the degree of drug ionization at a given pH value and to predict the probability of its penetration through the cell membrane.
(1)For dilute acid, A,
HA ↔ H + + A -, where HA is the concentration of the non-ionized (protonated) form of the acid and A - is the concentration of the ionized (non-protonated) form.
(2) For weak base, B,
BH + ↔ H + + B, where BH + is the concentration of the protonated form of the base, B is the concentration of the non-protonated form
Knowing the pH of the medium and the pKa of the substance, it is possible to determine the degree of drug ionization by the calculated logarithm, and hence the degree of its absorption from the gastrointestinal tract, reabsorption or excretion by the kidneys at different pH values of urine, etc.
8. Transfer of drugs in the body. Water diffusion and diffusion in lipids (Fick's law). Active transport.
The transfer of drugs in the body can be carried out by water and lipid diffusion, active transport, endo - and pinocytosis.
Features of the transfer of drugs in the body by water diffusion:
1. Epithelial integuments (mucous membranes of the gastrointestinal tract, oral cavity, etc.) - water diffusion of only very small molecules (methanol, lithium ions, etc.)
2. Capillaries (except for cerebral ones) - filtration of substances with a molecular weight of up to 20-30 thousand. Yes.
3. Capillaries of the brain - basically do not have water pores, with the exception of the areas of the pituitary gland, pineal gland, zone IV ventricle, choroid plexus, median eminence
4. Placenta - has no water pores (although a controversial issue).
5. Binding of drugs to blood proteins prevents their release from the bloodstream, and hence water diffusion
6. Diffusion in water depends on the size of drug molecules and water pores
Features of lipid diffusion:
1. The main mechanism of drug transfer across cell membranes
2. Determined by the lipophilicity of the diffusible substance (ie, the "oil / water" distribution coefficient) and the concentration gradient, it can be limited by the very low solubility of the substance in water (which prevents the drug from penetrating into the aqueous phase of membranes)
3. Non-polar compounds diffuse easily, ions are difficult to diffuse.
Any diffusion (both water and lipids) obeys Fick's law of diffusion:
Diffusion rate - the number of drug molecules carried per unit time; C1 is the concentration of the substance outside the membrane; C2 is the concentration of the substance from the inside of the membrane.
Corollary from Fick's law:
1) the filtration of the drug is the higher, the greater its concentration at the injection site (S of the absorbed surface in the intestine is greater than in the stomach, therefore the absorption of the drug into the intestine is faster)
2) the higher the drug concentration at the injection site, the higher the drug filtration
3) the filtration of drugs is the higher, the less the thickness of the biological membrane to be overcome (the thickness of the barrier in the alveoli of the lungs is much less than that of the skin, therefore the absorption rate is higher in the lungs)
Active transport- transfer of drugs, regardless of the concentration gradient using the energy of ATP, is characteristic of hydrophilic polar molecules, a number of inorganic ions, sugars, amino acids, pyrimidines. Characterized by: a) selectivity for certain compounds b) the possibility of competition of two substances for one transport mechanism c) saturation at high concentrations of the substance d) the possibility of transport against the concentration gradient e) energy consumption.
9. The central postulate of pharmacokinetics is the concentration of a drug in the blood - the main parameter for controlling the therapeutic effect. Tasks solved on the basis of knowledge of this postulate.
The central postulate (dogma) of pharmacokinetics: the drug concentration in blood plasma determines (quantitatively determines) the pharmacological effect.
In most cases, the rate of absorption, distribution, metabolism and excretion of drugs is proportional to their concentration in blood plasma (obeys the law of mass action), therefore, knowing it is possible:
1) determine the half-life (for drugs with first-order kinetics)
2) explain the duration of some toxic effects of drugs (for drugs in high doses with saturation kinetics)
10. Bioavailability of drugs - definition, essence, quantitative expression, determinants. Bioavailability
Bioavailability (F) - characterizes the completeness and rate of absorption of drugs with extra-systemic routes of administration - reflects the amount of unchanged substance that has reached the systemic circulation, relative to the initial dose of the drug.
F is 100% for drugs that are administered intravenously. When administered by other routes, F is usually less due to incomplete absorption and partial metabolism in peripheral tissues. F is 0 if the drug is not absorbed from the lumen of the gastrointestinal tract.
To estimate F, a curve is plotted as a function of the drug concentration in the blood versus time after its intravenous administration, as well as after administration by the investigated route. This is the so-called. pharmacokinetic curves of the relationship "time-concentration". By integration, the values of the area under the pharmacokinetic curve are found and F is calculated as the ratio:
![]() ≤ 1, where AUC is the Area Under Curve
≤ 1, where AUC is the Area Under Curve
Bioavailability> 70% is considered high, below 30% - low.
Determinants of bioavailability:
1) suction speed
2) completeness of absorption - insufficient absorption of drugs due to its very high hydrophilicity or lipophilicity, metabolism by intestinal bacteria when administered enterally, etc.
3) presystemic elimination - with high biotransformation in the liver F drugs are low (nitroglycerin when administered orally).
4) dosage form - sublingual tablets and rectal suppositories help drugs to avoid presystemic elimination.
11. Distribution of drugs in the body. Compartments, ligands. Main determinants of distribution.
Distribution Drugs - the process of spreading drugs through organs and tissues after they enter the systemic circulation.
Distribution bays:
1. Extracellular space (plasma, intercellular fluid)
2. Cells (cytoplasm, membrane of organelles)
3. Adipose and bone tissue (deposition of drugs)
 In a person weighing 70 kg, the volume of liquid media is 42 liters in total, then if:
In a person weighing 70 kg, the volume of liquid media is 42 liters in total, then if:
[Vd = 3-4 l, then all the medicine is distributed in the blood;
[Vd = 4-14 L, then all the drug is distributed in the extracellular fluid;
[Vd = 14-42 l, then all the drug is approximately evenly distributed in the body;
[Vd> 42 L, then all the drug is located mainly in the extracellular space.
Molecular ligands of drugs:
A) specific and non-specific receptors
B) blood proteins (albumin, glycoprotein) and tissues
C) connective tissue polysaccharides
D) nucleoproteins (DNA, RNA)
Distribution determinants:
· The nature of drugs- how smaller sizes molecules and lipophilic drugs, the faster and more uniform its distribution.
· Organ size- how bigger size organ, the more a drug can enter it without a significant change in the concentration gradient
· Organ blood flow- in well perfused tissues (brain, heart, kidneys), the therapeutic concentration of the substance is created much earlier than in poorly perfused tissues (fatty, bone)
· The presence of histohematogenous barriers- drugs easily penetrate tissues with poorly expressed GHB
· Plasma protein binding- the larger the bound drug fraction, the worse its distribution in the tissue, since only free molecules can leave the capillary.
· Deposition of the drug in tissues- the binding of drugs with tissue proteins contributes to its accumulation in them, since the concentration of free drugs in the perivascular space decreases and a high concentration gradient between blood and tissues is constantly maintained.
A quantitative characteristic of drug distribution is the apparent volume of distribution (Vd).
Apparent volume of distributionVd Is a hypothetical volume of fluid in which the entire administered dose of the drug can be distributed in order to create a concentration equal to the concentration in the blood plasma.
Vd is equal to the ratio of the administered dose (the total amount of the drug in the body) to its concentration in the blood plasma:
 .
.
The larger the apparent volume of distribution, the more drugs are distributed into the tissue.
12. Elimination constant, its essence, dimension, relationship with other pharmacokinetic parameters.
Elimination rate constant(kel, min-1) - shows what part of drugs is eliminated from the body per unit of time Þ Kel = Avid / Atot, where Avid is the amount of drugs released in units. time, Absh - the total amount of drugs in the body.
The kel value is usually found by solving a pharmacokinetic equation describing the process of drug elimination from the blood; therefore, kel is called a model kinetic index. Kel is not directly related to the planning of the dosage regimen, but its value is used to calculate other pharmacokinetic parameters.
The elimination constant is directly proportional to the clearance and inversely proportional to the volume of distribution (from the definition of clearance): Kel = CL / Vd; = hour-1 / min-1 = fraction per hour.
13. The half-life of drugs, its essence, dimension, relationship with other pharmacokinetic parameters.
Half-elimination period(t½, min) is the time required to reduce the concentration of drugs in the blood by exactly half. In this case, it does not matter in what way a decrease in concentration is achieved - with the help of biotransformation, excretion, or due to a combination of both processes.
The half-life is determined by the formula:
![]()
The half-life is the most important pharmacokinetic parameter that allows:
B) determine the time of complete elimination of the drug
C) predict the concentration of drugs at any time (for drugs with first-order kinetics)
14. Clearance as the main pharmacokinetic parameter for dosing regimen management. Its essence, dimension and relationship with other pharmacokinetic parameters.
Clearance(Cl, ml / min) - the volume of blood that is cleared from drugs per unit of time.
Since plasma (blood) is the "visible" part of the volume of distribution, the clearance is the fraction of the volume of distribution from which the drug is released per unit of time. If we denote the total amount of the drug in the body through General, and the amount that was allocated after Avyd, then:
![]() On the other hand, it follows from the definition of the volume of distribution that the total amount of the drug in the body is Absh =Vd´
CTer / plasma... Substituting this value into the clearance formula, we get:
On the other hand, it follows from the definition of the volume of distribution that the total amount of the drug in the body is Absh =Vd´
CTer / plasma... Substituting this value into the clearance formula, we get:
![]() .
.
Thus, clearance is the ratio of the rate of elimination of a drug to its concentration in blood plasma.
In this form, the clearance formula is used to calculate the maintenance dose of the drug ( DNS), that is, the dose of the drug that should compensate for the loss of the drug and maintain its level at a constant level:
Injection rate = Excretion rate =Cl´ CTer(dose / min)
DNS= injection rate´ T (T- the interval between taking the medication)
Ground clearance is additive, that is, the elimination of a substance from the body can occur with the participation of processes in the kidneys, lungs, liver and other organs: Clsystem = Clrenal. + Cl liver + Cld.
Clearance bound With drug half-life and volume of distribution: t1 / 2 = 0.7 * Vd / Cl.
15. Dose. Types of doses. Drug dosage units. Drug dosing targets, administration methods and options, administration interval.
The effect of drugs on the body is largely determined by their dose.
Dose- the amount of a substance introduced into the body at one time; expressed in weight, volume or conventional (biological) units.
Dose types:
A) single dose - the amount of substance per dose
B) daily dose - the amount of the drug prescribed per day in one or more doses
C) course dose - the total amount of the drug for the course of treatment
D) therapeutic doses - doses in which the drug is used for therapeutic or prophylactic purposes (threshold, or minimum effective, average therapeutic and higher therapeutic doses).
E) toxic and lethal doses - doses of drugs at which they begin to have pronounced toxic effects or cause death of the body.
E) loading (introductory) dose - the number of injected drugs, which fills the entire volume of distribution of the body in the effective (therapeutic) concentration: VD = (Css * Vd) / F
G) maintenance dose - a systematically administered amount of drugs that compensates for the loss of drugs with clearance: PD = (Css * Cl * DT) / F
Pharmaceutical dosage units:
1) in grams or fractions of a gram of drugs
2) the number of drugs per 1 Kg body weight (for example, 1 Mg / kg) or per unit surface area of the body (for example, 1 Mg / m2)
Drug dosing goals:
1) determine the amount of drugs required in order to cause the desired therapeutic effect with a certain duration
2) avoid the phenomena of intoxication and side effects with the introduction of drugs
Methods of drug administration: 1) enteral 2) parenteral (see section 5)
Drug administration options:
A) continuous (by long-term intravascular infusion of drugs by drop or through automatic dispensers). With continuous administration of drugs, its concentration in the body changes smoothly and does not undergo significant fluctuations.
B) intermittent administration (by injection or non-injection methods) - the introduction of a drug at regular intervals (dosing intervals). With intermittent administration of drugs, its concentration in the body constantly fluctuates. After taking a certain dose, it first rises, and then gradually decreases, reaching minimum values before the next administration of the drug. Fluctuations in concentration are the more significant, the larger the administered dose of the drug and the interval between injections.
Introduction interval- the interval between the administered doses, ensuring the maintenance of the therapeutic concentration of the substance in the blood.
16. Administration of drugs at a constant rate. Kinetics of drug concentration in blood. Stationary concentration of the drug in the blood ( Css), time of its achievement, calculation and management of it.
 The peculiarity of the introduction of drugs at a constant rate is a smooth change in its concentration in the blood upon administration, while:
The peculiarity of the introduction of drugs at a constant rate is a smooth change in its concentration in the blood upon administration, while:
1) the time to reach a steady-state drug concentration is 4-5t½ and does not depend on the infusion rate (the size of the administered dose)
2) with an increase in the infusion rate (injected dose), the СSS value also increases in a proportional number of times
3) elimination of the drug from the body after the termination of the infusion takes 4-5t½.
WITHSs- equilibrium stationary concentration- the concentration of drugs achieved at the rate of administration equal to the rate of excretion, therefore:
![]() (from the definition of clearance)
(from the definition of clearance)
For each subsequent half-life, the drug concentration increases by half of the remaining concentration. All drugs that obey the first order elimination law are Will reachCssafter 4-5 half-lives.
Level C Management ApproachesSs: change the administered dose of drugs or the interval of administration
17. Intermittent administration of drugs. Kinetics of drug concentration in blood, therapeutic and toxic concentration range. Calculation of the stationary concentration ( CSs), the boundaries of its oscillations and its control. Adequate discrete dosing interval.
 Fluctuations in the concentration of drugs in blood plasma: 1 - with constant intravenous drip; 2 - with a fractional introduction of the same daily dose with an interval of 8 hours; 3 - with the introduction of a daily dose with an interval of 24 hours.
Fluctuations in the concentration of drugs in blood plasma: 1 - with constant intravenous drip; 2 - with a fractional introduction of the same daily dose with an interval of 8 hours; 3 - with the introduction of a daily dose with an interval of 24 hours.
Intermittent drug administration- the introduction of a certain amount of drugs at intervals.
The steady-state equilibrium concentration is reached after 4-5 half-elimination periods, the time to reach it does not depend on the dose (at the beginning, when the drug concentration level is low, the rate of its elimination is also low; as the amount of the substance in the body increases, the rate of its elimination also increases, therefore, early or a moment will come late when the increased rate of elimination will balance the administered drug dose and further increase in concentration will stop)
Css is directly proportional to the drug dose and inversely proportional to the injection interval and drug clearance.
Css Swing Boundaries: ![]() ; Cssmin = Cssmax × (1 - email). Fluctuations in drug concentration are proportional to T / t1 / 2.
; Cssmin = Cssmax × (1 - email). Fluctuations in drug concentration are proportional to T / t1 / 2.
Therapeutic range (safety corridor, therapy window)- This is the range of concentrations from the minimum therapeutic to causing the first signs of side effects.
Toxic range- concentration range from the highest therapeutic to lethal.
Adequate administration of discrete doses: a mode of administration in which the fluctuation of the drug concentration in the blood falls within the therapeutic range. To determine an adequate regimen of drug administration, it is necessary to calculate. The difference between Cssmax and Cssmin should not exceed 2Css.
Oscillation controlCss:
Swing rangeCssdirectly proportional to the dose of drugs and inversely proportional to the interval of its administration.
1. Change the dose of drugs: with an increase in the dose of a drug, the range of fluctuations of its Css proportionally increases
2. Change the interval of drug administration: with an increase in the interval of drug administration, the range of fluctuations of its Css proportionally decreases
3. Simultaneously change the dose and the interval of administration
18. Introductory (loading) dose. Therapeutic meaning, calculation by pharmacokinetic parameters, conditions and limitations of its use.
Introductory (loading) dose- a dose administered at a time and fills the entire volume of distribution in the current therapeutic concentration. VD = (Css * Vd) / F; = mg / l, = l / kg
Therapeutic meaning: the introductory dose quickly provides an effective therapeutic concentration of drugs in the blood, which makes it possible, for example, to quickly stop an attack of asthma, arrhythmias, etc.
The introductory dose can be administered at a time only when The process of substance distribution is ignored
Limiting the use of VD: if the drug is distributed Significantly slower than its entry into the bloodstream, the introduction of the entire loading dose at once (especially intravenously) will create a concentration significantly higher than the therapeutic one and will cause the occurrence of toxic effects. VD use condition: therefore, the introduction of loading doses Should always be slow or fractional.
19. Maintenance doses, their therapeutic meaning and calculation for optimal regime dosing.
Maintenance dose- the dose of drugs administered systematically, which fills the clearance volume, that is, the Vd fragment that is cleared of drugs during the DT interval: PD = (Css * Cl * DT) / F.
Therapeutic meaning: PD compensates for losses with clearance over the interval between drug injections.
Calculation for the optimal dosage of drugs (for quick relief of an attack):
1. Calculate VD: VD = (Css * Vd) / F
2. Select the interval for the introduction of DT (usually most drugs are prescribed with an interval close to t1 / 2) and calculate the PD: PD = (Css * Cl * DT) / F
3. We check whether the drug fluctuations in the blood do not go beyond the therapeutic range by calculating Cssmax and Cssmin: ![]() ; Cssmin = Cssmax × (1 - email). The difference between Cssmax and Cssmin should not exceed two Css.
; Cssmin = Cssmax × (1 - email). The difference between Cssmax and Cssmin should not exceed two Css.
The fraction to be eliminated is found according to the graph (see section 16) or according to the formula: ![]()
4. If, at the interval of drug administration we have chosen, its fluctuations go beyond the therapeutic range, change DT and repeat the calculation (point 2 - point 4)
NB! If the drug is not intended for the relief of emergency conditions or is taken in pills, the VD is not calculated.
20. Individual, age and sex differences in drug pharmacokinetics. Corrections for the calculation of individual values for the volume of distribution of drugs.
1. Age differences pharmacokinetics of drugs.
|
1. The stratum corneum is thinner, therefore, when applied to the skin, drugs are better absorbed. The absorption of drugs by rectal administration is also better. 2. The volume of fluid in the body of children is 70-80%, while in adults it is only »60%, therefore, the Vd of hydrophilic drugs they have is higher and higher doses are required. 3. In a newborn, the level of albumin in plasma is lower than in adults, therefore, the binding of drugs to protein is less intense in them. 4. Newborns have low intensity of cytochrome P450 systems and conjugating enzymes, but high activity of methylating systems. 5. The rate of glomerular filtration in the kidneys of children under 6 months is 30-40% of the rate of adults, therefore, renal excretion of drugs is reduced. |
1. There is a decrease in the concentration of albumin in the blood plasma and the fraction of the drug associated with the protein 2. The water content in the body decreases from 60% to 45%, therefore, the accumulation of lipophilic drugs increases. 3. The glomerular filtration rate can drop to 50-60% of the rate of a mature patient, therefore renal elimination of drugs is sharply limited. |
2. Sex differences in the action of drugs... Women are characterized by a lower body weight than men, therefore, the size of the drug doses for them should, as a rule, be at the lower limit of the therapeutic dose range.
3. Pathological conditions of the body and the effect of drugs
A) liver diseases: F drugs due to the shutdown of the first-pass metabolism, a fraction of unbound drugs due to a lack of albumin synthesis, the effects of drugs are prolonged due to their biotransformation.
B) kidney pathology: the elimination of drugs that are excreted through the kidneys slows down
4. Genetic factors- a deficiency of certain enzymes of drug metabolism can contribute to the prolongation of their action (pseudocholinesterase, etc.)
Corrections for calculating individual values of the volume of distribution of drugs:
A) for obesity, lipophobic drugs are insoluble in adipose tissue Þ it is necessary to calculate ideal weight by height (Broca's formula: ideal weight = height (in cm) - 100) and recalculate Vd by the ideal weight by height.
B) with edema, you need to calculate the excess volume of water = overweight- ideal, Vd should be increased per liter of each excess kilogram of water.
Dependence of the main pharmacokinetic parameters on various factors:
1. Absorption of drugs: at age ¯ drug absorption, its metabolism in the course of presystemic elimination, the bioavailability of drugs changes.
2. Volume of distribution Vd: ¯ with age and with obesity, with edema
3. Half-life: changes with age and obesity (since Vd decreases)
4. Clearance: determined by the functional state of the kidneys and liver
21. Renal clearance of drugs, mechanisms, their quantitative and qualitative characteristics.
Renal clearance is a measure of the volume of blood plasma, which is cleared of a medicinal substance per unit of time by the kidneys: Cl (ml / min) = U × V / P, where U is the concentration of drugs in ml of urine, V is the volume of urine excreted in min and P = drug concentration in ml of plasma.
Renal clearance mechanisms and their characteristics:
1. Filtration: Drugs emitted Filtration only(insulin) will have a clearance equal to GFR (125-130 ml / min)
Determined by: renal blood flow, unbound drug fraction and kidney filtration capacity.
Most drugs have low molecular weights and are therefore freely filtered from the plasma in the glomerulus.
2. Active secretion: Drugs emitted Filtration and total secretion(paraaminogippuric acid), will have a clearance equal to renal plasma clearance (650 ml / min)
The renal tubule contains two transport systems that can separate drugs into an ultrafiltrate, one for organic acids and another for organic bases. These systems require energy to actively transport against the concentration gradient; they are a place of competition for a carrier of some drugs with others.
Determined by: maximum secretion rate, urine volume
3. Reabsorption: clearance values between 130 and 650 ml / min suggest that the drug is Filtered, excreted, and partially reabsorbed
Reabsorption occurs throughout the entire renal canal and depends on the polarity of the drug, non-polar, lipophilic are reabsorbed.
Determined by: primary pH value and drug ionization
A number of indicators such as Age, joint use of several drugs, diseases significantly affect renal clearance:
A) renal failure ® decrease in drug clearance high level Drugs in blood
B) glomerulonephritis ® loss of serum protein, which was usually available and associated with drugs ® increase in the level of the free fraction of drugs in plasma
22. Factors affecting the renal clearance of drugs. Dependence of clearance on the physicochemical properties of drugs.
Factors affecting renalCl:
A) glomerular filtration
B) renal blood flow rate
B) maximum rate of secretion
D) urine volume
E) fraction unbound in blood
Dependence of renal clearance on the physicochemical properties of drugs:
General patterns: 1) polar drugs are not reabsorbed, non-polar drugs are reabsorbed 2) ionic drugs are secreted, non-ionic drugs are not secreted.
I. Non-polar non-ionic substances: filtered only in unbound forms, not secreted, reabsorbed
Renal clearance is small and is determined by: a) the fraction of drugs unbound in the blood b) the volume of urine
II. Polar non-ionic substances: filtered in unbound form, do not secrete, do not reabsorb
Renal clearance is high, determined by: a) the fraction of drugs unbound in the blood b) the rate of glomerular filtration
III. Non-polar ionized in urine in non-ionic form: filtered, actively secreted, non-polar reabsorbed
Renal clearance is determined by: a) the fraction of drugs unbound in the blood b) the fraction of drugs ionized in the urine c) the volume of urine
IV. Polar ionized in urine in non-ionized form: filtered, actively secreted, not reabsorbed
Renal clearance is determined by: a) renal blood flow and glomerular filtration rate b) maximum secretion rate
23. Hepatic drug clearance, its determinants and limitations. Enterohepatic drug cycle.
Mechanisms of hepatic clearance:
1) metabolism (biotransformation) by oxidation, reduction, alkylation, hydrolysis, conjugation, etc.
The main strategy of xenobiotic metabolism: non-polar substances ® polar (hydrophilic) metabolites excreted in the urine.
2) secretion (excretion of non-transformed substances into bile)
Only polar substances with a molecular weight> 250 active are transported into bile (organic acids, bases).
Determinants of hepatic clearance:
A) The rate of blood flow in the liver
B) Maximum speed excretion or metabolic conversion
B) Km - Michaelis constant
D) Non-protein bound fraction
Limitations of hepatic clearance:
1. If Vmax / Km is large → Cl pecs = blood flow velocity in the liver
2. If Vmax / Km mean values → Cl = the sum of all factors
3. If Vmax / Km is small → Cl furnace is small, limited
Enterohepatic drug cycle - A number of drugs and products of their transformation in significant quantities are excreted with bile into the intestines, from where they are partially excreted with excrement, and partly - Reabsorbed into the blood, again enters the liver and is excreted into the intestines.
Hepatic elimination of drugs can be significantly altered Liver disease, age, diet, genetics, duration of drug prescription(for example, due to the induction of hepatic enzymes), and other factors.
24. Factors that change the clearance of medicinal substances.
1. Drug interactions at the level of: renal secretion, biochemical transformation, phenomena of enzymatic induction
2. Kidney disease: blood flow disorders, acute and chronic kidney damage, outcomes of long-term renal disease
3. Liver diseases: alcoholic cirrhosis, primary cirrhosis, hepatitis, hepatomas
4. Diseases of the gastrointestinal tract and endocrine organs
5. Individual intolerance (lack of acetylation enzymes - aspirin intolerance)
25. Correction of drug therapy for liver and kidney diseases. General approaches. Correction of the dosage regimen under the control of the total clearance of the drug.
1. Cancel drugs that are not necessary
2. For kidney disease, use drugs excreted in the liver and vice versa.
3. Reduce the dose or increase the interval between injections
4. Close monitoring of side effects and toxic effects
5. In the absence of a pharmacological effect, the dose must be increased slowly and under the control of pharmacological and toxic effects.
6. If possible, determine the concentration of the substance in the plasma and correct the therapy according to the Cl of the drug individually
7. Use an indirect method of assessing Cl.
Correction of the dosage regimen under the control of the total clearance of the drug:
Dose adjustment : Dind = Dtyp. × Clind. / Cltyp.
With continuous intravenous administration of the drug: Individual rate of administration = Typical rate of administration × Cl ind. / Cl typical
With intermittent administration: 1) change the dose 2) change the interval 3) change both parameters. For example, if the clearance is reduced by 50%, you can reduce the dose by 50% and keep the interval, or double the interval and keep the dose. It is preferable to reduce the dose and maintain the interval of administration.
26. Correction of the dosage regimen under the control of the residual renal function.
Creatinine clearance- the most important quantitative indicator of renal function, on the basis of which it is possible to adjust the dosage regimen
We know:
A) residual renal function, determined by creatinine clearance in a given patient Clcr / patient
B) the total clearance of a given drug (CLP / total) and the proportion of renal drug clearance in the total clearance
C) normal creatinine clearance Clcr / normogram
3) Css and F for this LAN (from the reference)
To find: drug dose for this patient
ClPS / renal norm = ClPS / total X share of renal drug clearance in total clearance
CLP / renal patient = Clcr / patient / Clcr / norm * ClLS / renal norm
ClPP / non-renal rate = ClPP / total - ClPP / renal rate
ClPS / total patient = CLPS / renal patient + ClPS / non-renal norm
The dose of this drug inside with normal renal function is: PD norm = Css X Cl / F
The dose of this drug inside for our patient is equal to: PD of the patient = PD norm X СlPS / general patient / СlPS / total
Answer: PDbolny
27. Correction of drug therapy for liver damage and other pathological conditions.
Liver disease can reduce clearance and lengthen the half-life of many drugs. However, in some drugs that are eliminated by the liver, these parameters do not change in case of liver dysfunction, therefore Liver disease does not always affect intrinsic hepatic clearance... There is currently no reliable marker that can be used to predict hepatic clearance similar to creatinine clearance.
For correction of the dosage regimen for kidney disease, see paragraph 26 above, for general principles of correction, see paragraph 25.
28. Strategy for individual drug therapy.
Recognition of the important role of concentration as a link between pharmacokinetics and pharmacodynamics contributes to the creation of a target concentration strategy - dose optimization in a given patient based on the measurement of drug concentration. It consists of the following stages:
1. Choice of target concentration
2. Calculate Vd and Cl based on typical values and make adjustments for factors such as body weight and renal function.
3. Entering the loading dose or maintenance dose, calculated taking into account the values of TC, Vd and Cl.
4. Registration of the patient's reaction and determination of drug concentration
5. Revision of Vd and Cl based on the results of concentration measurements.
6. Repeat steps 3-6 to adjust the maintenance dose required for optimal drug response.
29. Biotransformation of drugs, its biological meaning, main direction and influence on the activity of drugs. The main phases of metabolic transformations of drugs in the body.
Biotransformation of drugs- chemical transformations of drugs in the body.
The biological meaning of biotransformation of drugs: creation of a substrate convenient for subsequent disposal (as an energy or plastic material) or in accelerating the elimination of drugs from the body.
The main direction of metabolic transformations of drugs: non-polar drugs → polar (hydrophilic) metabolites excreted in the urine.
There are two phases of metabolic reactions of drugs:
1) Metabolic transformation (non-synthetic reactions, phase 1)- transformation of substances due to microsomal and extra-microsomal oxidation, reduction and hydrolysis
2) conjugation (synthetic reactions, phase 2)- biosynthetic process, accompanied by the addition of a number of chemical groups or molecules of endogenous compounds to a drug or its metabolites by a) the formation of glucuronides b) glycerol esters c) sulfoesters d) acetylation e) methylation
The effect of biotransformation on the pharmacological activity of drugs:
1) most often, biotransformation metabolites do not have pharmacological activity or their activity is reduced in comparison with the initial substance
2) in some cases, metabolites can retain activity and even exceed the activity of the parent substance (codeine is metabolized to more pharmacologically active morphine)
3) sometimes toxic substances are formed during biotransformation (metabolites of isoniazid, lidocaine)
4) sometimes during biotransformation, metabolites with opposite pharmacological properties are formed (metabolites of nonselective agonists of b2-adrenergic receptors have the properties of blockers of these receptors)
5) a number of substances are prodrugs that initially do not give pharmacological effects, but in the course of biotransformation they are converted into biologically active substances (inactive L-dopa, penetrating through the BBB, turns into active dopamine in the brain, while there are no systemic effects of dopamine).
30. Clinical significance of drug biotransformation. Influence of gender, age, body weight, environmental factors, smoking, alcohol on the biotransformation of drugs.
Clinical significance of drug biotransformation: since the dose and frequency of administration required to achieve an effective concentration in the blood and tissues may vary in patients due to individual differences in the distribution, metabolic rate and elimination of drugs, it is important to take them into account in clinical practice.
The influence of various factors on the biotransformation of drugs:
BUT) Functional state liver: in case of her diseases, the clearance of drugs usually decreases, and the elimination half-life increases.
B) Influence of environmental factors: smoking promotes the induction of cytochrome P450, as a result of which the metabolism of drugs is accelerated during microsomal oxidation
IN) Vegetarians biotransformation of drugs is slowed down
D) elderly and young patients are characterized by hypersensitivity to the pharmacological or toxic effect of drugs (in the elderly and in children under 6 months of age, the activity of microsomal oxidation is reduced)
E) in men, the metabolism of some drugs is faster than in women, since androgens stimulate the synthesis of microsomal liver enzymes (ethanol)
E) High protein content and intense exercise stress : acceleration of drug metabolism.
F) Alcohol and obesity slow down the metabolism of drugs
31. Metabolic drug interactions. Diseases affecting their biotransformation.
Metabolic interaction of drugs:
1) induction of enzymes of drug metabolism - an absolute increase in their number and activity due to exposure to certain drugs. Induction leads to an acceleration of drug metabolism and (as a rule, but not always) to a decrease in their pharmacological activity (rifampicin, barbiturates - cytochrome P450 inducers)
2) inhibition of enzymes of drug metabolism - inhibition of the activity of metabolic enzymes under the influence of some xenobiotics:
A) competitive metabolic interaction - drugs with high affinity for certain enzymes reduce the metabolism of drugs with a lower affinity for these enzymes (verapamil)
B) binding to a gene that induces the synthesis of certain isoenzymes of cytochrome P450 (cymedin)
C) direct inactivation of cytochrome P450 isoenzymes (flavonoids)
Diseases affecting the metabolism of drugs:
A) kidney disease (impaired renal blood flow, acute and chronic diseases kidney, outcomes of long-term renal disease)
B) liver disease (primary and alcoholic cirrhosis, hepatitis, hepatoma)
C) diseases of the gastrointestinal tract and endocrine organs
C) individual intolerance to some drugs (lack of acetylation enzymes - intolerance to aspirin)
32. Ways and mechanisms of drug excretion from the body. Possibilities of drug elimination management.
Ways and mechanisms of drug excretion: elimination of drugs by the liver and kidneys and some other organs:
A) by the kidneys by filtration, secretion, reabsorption
B) by the liver by biotransformation, excretion with bile
C) through the lungs, saliva, sweat, milk, etc. by secretion, evaporation
Possibilities for managing the processes of drug withdrawal:
1. pH control: in alkaline urine, the excretion of acidic compounds increases, in acidic urine, the excretion of basic compounds
2.use of choleretic drugs (cholenzyme, allochol)
3.hemodialysis, peritoneal dialysis, hemosorption, lymphosorption
4.Forced diuresis (IV NaCl or glucose for water load + furosemide or mannitol)
5.gastric lavage, use of enemas
33. The concept of receptors in pharmacology, the molecular nature of receptors, signaling mechanisms of drug action (types of transmembrane signaling and secondary mediators).
Receptors - Molecular components of a cell or organism that interact with drugs and induce a number of biochemical events leading to the development of a pharmacological effect.
The concept of receptors in pharmacology:
1. Receptors determine the quantitative patterns of drug action
2. Receptors are responsible for the selectivity of drug action
3. Receptors mediates the action of pharmacological antagonists
The concept of receptors is the basis for the targeted use of drugs that affect regulatory, biochemical processes and communication.
Molecular nature of receptors:
1.regulatory proteins, mediators of the action of various chemical signals: neurotransmitters, hormones, autocoids
2.enzymes and transmembrane transporter proteins (Na +, K + ATPase)
3.structural proteins (tubulin, cytoskeletal proteins, cell surface)
4.nuclear proteins and nucleic acids
Signaling mechanisms of drug action:
1) the penetration of lipid-soluble ligands through the membrane and their effect on intracellular receptors.
2) the signaling molecule binds to the extracellular domain of the transmembrane protein and activates the enzymatic activity of its cytoplasmic domain.
3) the signaling molecule binds to the ion channel and regulates its opening.
4) the signaling molecule binds to a receptor on the cell surface, which is coupled to the effector enzyme via the G-protein. The G-protein activates a secondary messenger.
Types of transmembrane signaling:
A) through 1-TMS receptors with and without tyrosine kinase activity
B) through 7-TMS receptors associated with G-protein
B) through ion channels (ligand-dependent, voltage-dependent, gap contacts)
Secondary intermediaries: cAMP, Ca2 + ions, DAG, IF3.
34. Physicochemical and chemical mechanisms of action of medicinal substances.
BUT) Physicochemical interaction with a biosubstrate- non-electrolytic action.
The main pharmacological effects: 1) narcotic 2) general depressive 3) paralyzing 4) locally irritating 5) membranolytic action.
Chemical nature of substances: chemically inert hydrocarbons, ethers, alcohols, aldehydes, barbiturates, gas drugs
The mechanism of action is the reversible destruction of membranes.
B) Chemical(molecular-biochemical) mechanism of action of drugs.
The main types of chemical interaction with a biosubstrate:
- Weak (non-covalent, reversible interactions) (hydrogen, ionic, monodipole, hydrophobic).
- Covalent bonds (alkylation).
The importance of non-covalent drug interactions: the action is nonspecific, does not depend on the chemical structure of the substance.
Significance of drug covalent interactions: action is specific, critically depends on chemical structures, is realized by influencing the receptors.
35. Terms and concepts of quantitative pharmacology: effect, efficacy, activity, agonist (full, partial), antagonist. Clinical difference between the concepts of activity and effectiveness of drugs.
 Effect (response)- quantitative yield of the reaction of interaction of a cell, organ, system or organism with a pharmacological agent.
Effect (response)- quantitative yield of the reaction of interaction of a cell, organ, system or organism with a pharmacological agent.
Efficiency- the measure of the reaction along the axis of the effect - the magnitude of the response of the biological system to the pharmacological effect; This is the ability of drugs to provide the maximum possible effect for it.... That is, in fact, this is the maximum size of the effect that can be achieved with the introduction of a given drug. It is numerically characterized by the value of Emax. The higher the Emax, the higher the effectiveness of the drug.
Activity- a measure of sensitivity to drugs along the concentration axis, characterizes the affinity (affinity of the ligand for the receptor), Shows what dose (concentration) of the drug is capable of causing the development of a standard effect equal to 50% of the maximum possible for this drug. Numerically characterized by the value of EC50 or ED50. The higher the drug activity, the lower its dose is required to reproduce the therapeutic effect.
Efficiency: 1 = 2> 3
Activity: 1> 3> 2
In clinical practice, it is more important to know the effectiveness, rather than the activity, since we are more interested in the ability of drugs to cause a certain action in the body.
Agonist- a ligand that binds to the receptor and causes a biological response, the activation of the physiological system. Full agonist- maximum response, Partial- cause less reaction even when all receptors are occupied.
Antagonist- ligands that occupy receptors or change them in such a way that they lose the ability to interact with other ligands, but do not themselves cause a biological reaction (block the action of agonists).
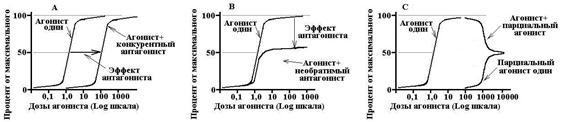 Competitive antagonists- interact with receptors reversibly and thus compete with agonists. Increasing the concentration of the agonist can completely eliminate the effect of the antagonist. The competitive antagonist shifts the dose-response curve for the agonist, increases the EC50, does not affect Emax.
Competitive antagonists- interact with receptors reversibly and thus compete with agonists. Increasing the concentration of the agonist can completely eliminate the effect of the antagonist. The competitive antagonist shifts the dose-response curve for the agonist, increases the EC50, does not affect Emax.
Non-competitive antagonists- irreversibly change the affinity of receptors for the agonist, binding often does not occur with the active site of the receptor, an increase in the concentration of the agonist does not eliminate the effect of the antagonist. A noncompetitive antagonist decreases Emax, does not change the EC50, and the dose-response curve is compressed about the vertical axis.
36. Quantitative patterns of drug action. The law of decreasing the response of biological systems. Clark's model and its consequences. General view of the dependence concentration - effect in normal and lognormal coordinates.
Clark-Ariens model:
1. The interaction between ligand (L) and receptor (R) is reversible.
2. All receptors for a given ligand are equivalent and independent (their saturation does not affect other receptors).
3. The effect is directly proportional to the number of occupied receptors.
4. The ligand exists in two states: free and bound to the receptor.
BUT) ![]() , where Kd is the equilibrium constant, Ke is the internal activity.
, where Kd is the equilibrium constant, Ke is the internal activity.
B) Since with an increase in the number of ligands at some point in time, all receptors will be occupied, the maximum possible number of ligand-receptor complexes formed is described by the formula:
= [R] × ![]() (1)
(1)
The effect is determined by the probability of activation of the receptor upon binding to the ligand, i.e., by its intrinsic activity (Ke), therefore E = Ke ×. In this case, the effect is maximum at Ke = 1 and minimum and Ke = 0. Naturally, the maximum effect is described by the ratio Emax = Ke ×, where is the total number of receptors for a given ligand
The effect also depends on the concentration of the ligand on the [C] receptors, therefore
E = Emax ![]() (2)
(2)
It follows from the above relations that EC50 = Kd
![]()
Emax is the maximum effect, Bmax is the maximum number of bound receptors, EC50 is the drug concentration at which an effect equal to half of the maximum occurs, Kd is the constant of dissociation of the substance from the receptor, at which 50% of the receptors are bound.
The law of decreasing response the parabolic dependence "concentration - efficiency" corresponds. The response to low doses of drugs usually increases in direct proportion to the dose... However, as the dose is increased, the increase in response decreases and ultimately a dose can be reached at which there is no further increase in response (due to the occupation of all receptors for a given ligand).
37. Changing the effect of drugs. Gradual and quantum evaluation of the effect, essence and clinical applications. Measures quantify activity and effectiveness of drugs in experimental and clinical practice.
All pharmacological effects can be roughly divided into two categories:
BUT) Gradual (continuous, integral) effects- such effects of drugs that can be measured quantitatively (the effect of antihypertensive drugs - by the level of blood pressure). A gradual "dose-effect curve" (see p. 36) is described, on the basis of which it is possible to estimate: 1) individual sensitivity to drugs 2) drug activity 3) maximum drug efficacy
B) Quantum Effects- such effects of drugs, which are a discrete value, a qualitative sign, that is, they are described by only a few variants of states (headache after taking an analgesic, either present or not). A quantum dose-effect curve is described, where the dependence of the manifestation of the effect in the population on the value of the taken drug dose is noted. The dose-effect plot is dome-shaped and is identical to the Gaussian normal distribution curve. Based on the quantum curve, one can: 1) assess the population sensitivity of drugs; 2) note the presence of an effect at a given dose; 3) select an average therapeutic dose.
Differences between gradual and quantum dose-effect characteristics:
A quantitative assessment of the activity and effectiveness of drugs is carried out on the basis of constructing dose-effect curves and their subsequent assessment (see Clause 35)
38. Types of drugs action. Changes in the action of drugs when they are re-administered.
Types of drug action:
1. Local action- the effect of a substance that occurs at the site of its application (anesthetic - on the mucous membrane)
2. Resorptive (systemic) action- the action of a substance that develops after its absorption, entry into the general bloodstream, and then into the tissues. Depends on the routes of drug administration and their ability to penetrate biological barriers.
With both local and resorptive action, drugs can have either Direct or Reflex influence:
A) direct influence - direct contact with the target organ (adrenaline on the heart).
B) reflex - a change in the function of organs or nerve centers by influencing extero - and interoreceptors (mustard plasters with respiratory pathology reflexively improve their trophism)
Changes in the action of drugs when they are reintroduced:
1. Cumulation- an increase in the effect due to the accumulation of drugs in the body:
a) material cumulation - the accumulation of an active substance in the body (cardiac glycosides)
b) functional cumulation - increasing changes in the function of body systems (changes in the function of the central nervous system in chronic alcoholism).
2. Tolerance (addiction) - Decrease in the body's response to repeated injections of drugs; in order to restore the reaction to drugs, it has to be administered in larger and larger doses (diazepam):
A) true tolerance - observed both with enteral and parenteral administration of drugs, does not depend on the degree of its absorption into the bloodstream. It is based on pharmacodynamic mechanisms of addiction:
1) desensitization - a decrease in the sensitivity of the receptor to the drug (b-adrenergic agonists, with prolonged use, lead to phosphorylation of b-adrenergic receptors, which are unable to respond to b-adrenergic agonists)
2) Down-regulation - a decrease in the number of drug receptors (with repeated administration of narcotic analgesics, the number of opioid receptors decreases and more and more doses of the drug are required to induce the desired response). If a drug blocks receptors, then the mechanism of tolerance to it may be associated with up-regulation - an increase in the number of drug receptors (b-blockers)
3) the inclusion of compensatory mechanisms of regulation (with repeated injections of antihypertensive drugs, collapse occurs much less often than with the first administration due to the adaptation of baroreceptors)
B) relative tolerance (pseudo-tolerance) - develops only with the introduction of drugs inside and is associated with a decrease in the rate and completeness of drug absorption
3. Tachyphylaxis- a condition in which frequent administration of drugs causes the development of tolerance after a few hours, but with rather rare administrations of drugs, its effect is fully preserved. The development of tolerance is usually associated with the depletion of the effector systems.
4. Drug addiction- an irresistible desire to take a substance previously administered. Allocate mental (cocaine) and physical (morphine) drug addiction.
5. Hypersensitivity- an allergic or other immunological reaction to drugs with repeated administration.
39. The dependence of the action of drugs on age, gender and individual characteristics organism. The meaning of circadian rhythms.
BUT) From age: in children and the elderly, the sensitivity to drugs is increased (since children have a deficiency of many enzymes, renal function, increased BBB permeability, absorption of drugs is slowed down in old age, metabolism is less efficient, the rate of excretion of drugs by the kidneys is reduced):
|
1. Newborns have reduced sensitivity to cardiac glycosides, since they have more Na + / K + -ATPases (targets of glycoside action) per unit area of the cardiomyocyte. 2. Children have lower sensitivity to succinylcholine and atracuria, but increased sensitivity to all other muscle relaxants. 3. Psychotropic drugs can cause abnormal reactions in children: psychostimulants - can increase concentration and reduce motor hyperactivity, tranquilizers - on the contrary, can cause so-called. atypical agitation. |
1. The sensitivity to cardiac glycosides increases sharply due to a decrease in the number of Na + / K + -ATPases. 2. Decreases sensitivity to b-blockers. 3. The sensitivity to calcium channel blockers increases, since the baroreflex is weakened. 4. There is an atypical reaction to psychotropic drugs, similar to the reaction of children. |
B) From the floor:
1) antihypertensive drugs - clonidine, b-blockers, diuretics can cause a violation sexual functions in men, but do not affect work reproductive system women.
2) anabolic steroids are more effective in women than in men.
IN) From the individual characteristics of the organism: deficiency or excess of certain enzymes of drug metabolism leads to an increase or decrease in their action (deficiency of blood pseudocholinesterase - abnormally prolonged muscle relaxation when using succinylcholine)
G) From circadian rhythms: change in the effect of drugs on the body, quantitatively and qualitatively, depending on the time of day (maximum effect with maximum activity).
40. Variability and variability of drug action. Hypo - and hyperreactivity, tolerance and tachyphylaxis, hypersensitivity and idiosyncrasy. Reasons for the variability of drug action and rational therapy strategy.
Variability reflects the differences between individuals in response to a given drug.
The reasons for the variability of the drug action:
1) a change in the concentration of a substance in the receptor zone - due to differences in the rate of absorption, its distribution, metabolism, elimination
2) variations in the concentration of the endogenous ligand of the receptor - propranolol (β-blocker) slows down the heart rate in people with increased levels of catecholamines in the blood, but does not affect the background heart rate in athletes.
3) changes in the density or function of receptors.
4) changes in the reaction components located distal to the receptor.
Rational therapy strategy: the appointment and dosage of drugs, taking into account the above reasons for the variability of drug action.
Hyporeactivity- a decrease in the effect of a given dose of drugs in comparison with the effect that is observed in most patients. Hyperreactivity- an increase in the effect of a given dose of drugs in comparison with the effect that is observed in most patients.
Tolerance, tachyphylaxis, hypersensitivity - see item 38
Idiosyncrasy- a perverse reaction of the body to this drug, associated with the genetic characteristics of drug metabolism or with individual immunological reactivity, including allergic reactions.
41. Assessment of drug safety. Therapeutic index and standard safety margins.
Safety assessment is carried out at two levels:
A) preclinical (obtaining information about the toxicity of drugs, the effect on reproductive functions, embryotoxicity and teratogenicity, long-term effects)
B) clinical (further assessment of the effectiveness and safety of drugs)
If, after the effect plateau is reached, the dose of the drug continues to grow, then after a certain period of time its toxic effect will begin to manifest itself. The dependence of the toxic effect on the dose (concentration) of the drug is of the same nature as its beneficial effect and can be described by gradual or quantum curves. These curves can also be used to determine the value TD50 or TC50- toxic dose (concentration) of drugs, which causes a toxic effect equal to 50% of the maximum (for a quantum curve - toxic effect in 50% of individuals in the population). Sometimes, instead of TD50, they use the indicator LD50 - lethal dose, which causes the death of 50% of objects in the population.
The assessment of drug safety is characterized on the basis of gradule or quantum dose-effect curves and the following indicators:
BUT) Therapeutic index Is the ratio between the toxic and effective doses of the drug that cause the appearance of a half-maximal effect: TI = TD50 / ED50. The higher the value of the therapeutic index, the safer the medicine is.
B) Therapeutic latitude (therapeutic window) Is the dose range between the minimum therapeutic and minimum toxic doses of drugs. It is a more correct indicator of drug safety, since it allows one to take into account the degree of increase in undesirable effects on the dose-effect curve.
IN) Reliable security factor- This is the ratio of the minimum toxic dose to the maximum effective dose (PNF = TD1 / ED99), shows how many times the therapeutic dose of the drug can be exceeded without the risk of intoxication (unwanted effects).
G) Therapy corridor Is the range of effective concentrations of a drug in the blood that must be created and maintained in the body in order to achieve the desired therapeutic effect.
42.46. Interaction of drugs. Incompatibility of drugs (since the questions are interrelated, choose according to the circumstances)
Drug interaction- this is a change in the severity and nature of the effects with the simultaneous or preliminary use of several drugs.
Reasons for unwanted interactions:
1) polypharmacy - 6 or more drugs give 7 times more side effects than if drugs are less than 6.
2) doctors' mistakes
3) violation of the dosage regimen
Rationale for combination therapy:
1. Monotherapy is not effective enough.
2. Absence of etiotropic therapy in most diseases Þ the need for drug action on different links of pathogenesis
3. Polymorbidity - than older person, the more diseases he has that occur at the same time
4. The need to correct the unwanted effects of drugs
5. Reducing the number of receptions and administration of drugs (convenience for the patient, saving the labor of health workers)
Types of interaction:
I. Pharmaceutical interaction - The type of interaction associated with a physicochemical reaction between drugs during the manufacture of a medicinal product, even before the introduction of these agents into the human body
A) typical mistakes leading to pharmaceutical incompatibility: writing out complex prescriptions, improper storage, the possibility of adsorption of drugs on the surface of plastic (organic nitrates) is not taken into account
B) problems with infusion therapy: mixing of soluble salts, derivatives of insoluble weak acids or bases leads to their precipitation; in liquid dosage forms, cardiac glycosides and alkaloids are hydrolyzed, AB is destroyed; pH of the medium (alkaloids precipitate in an alkaline medium)
C) recommendations: 1) It is better to prepare all mixtures ex tempore 2) The most reliable solution is with one drug 3) All solutions must be checked for suspensions before use 4) Interaction can occur without visible changes in solutions 5) Drugs cannot be added to blood and AK solutions 6) In the absence of special instructions, the preparations should be dissolved in 5% glucose solution (pH 3.5-6.5), isotonic NaCl solution (pH 4.5-7.0).
HCl-stabilized glucose solution is incompatible with epinephrine, benzylpenicillin, apomorphine, kanamycin, vitamin C, oleandomycin, cardiac glycosides. Cardiac glycosides are incompatible with atropine, papaverine, platifillin. AB are incompatible with heparin, hydrocortisone. Vitamins of group B are incompatible with each other, with vitamins PP, C. Vitamin PP and C are also incompatible with each other.
Cannot be mixed with any other drugs: phenothiazide, chlorpromazine, barbiturates, vitamin C preparations, amphotericin B, furosemide, sulfadiazine, aminophylline, adrenomimetics.
II... Pharmacological- drug interaction, which manifests itself only in the human body after their combined use
A) pharmacokinetic
1) during the suction phase.
When introducingPer Osinteraction is determined by:
1.acidity of the environment
2.direct interaction in the digestive tract
Tetracyclines interact with calcium, aluminum, iron, magnesium to form chelate complexes. Cholestyramine interferes with the absorption of acid derivatives, calcium preparations, varvarine, digoxin, digitoxin, fat-soluble vitamins, trimethoprim, clindamycin, cephalexin, tetracycline. Iron preparations are better absorbed with vitamin C. Iron preparations with carbonates, tetracyclines are poorly absorbed.
3.Gastrointestinal motility
Slow down peristalsis: some antidepressants, antihistamine drugs, phenothiazine antipsychotic drugs, narcotic drugs, increase the absorption of digoxin, corticosteroids, anticoagulants, reduce the absorption of levodopa. Strengthen peristalsis and increase evacuation from the gastrointestinal tract: metoclopramide, laxatives. Reduce drug absorption: phenobarbital - griseofulvin, aspirin - indomethacin and diclofenac, PASK - rifampicin.
Methods for controlling absorption during parenteral administration: local anesthetics + epinephrine + phenylephrine - absorption of local anesthetics decreases
4.intestinal flora
5.changing the suction mechanism
2) when distributing and depositing:
1.direct interaction in blood plasma: gentamicin + ampicillin or carbenicillin - reduce the activity of gentamicin
2. competitive displacement from the connection with albumin in the blood plasma: indomethacin, digitoxin, warfarin are associated with blood proteins by 90-98%, therefore, a twofold increase in the free fraction of drugs is a sharp increase in toxic effects; NSAIDs are replacing: warfarin, phenytoin, methotrexate.
Determinants that determine the clinical significance of this interaction:
ü Vd value (large - no problem, small - possible)
ü the effect of one drug substance on the activity of transport mechanisms through the mechanisms of other drugs: the drug transport increases dose-dependently - insulin, ACTH, angiotensin, kinins, etc .; insulin increases the concentration of isoniazid only in the lungs, and the concentration of cottonromazine - only in the SMC.
3.Displacement from tissue protein binding: quinidine displaces digoxin + reduces renal excretion, therefore increasing the risk of digoxin toxicity
3) in the process of metabolism
Drugs can increase or decrease the activity of cytochrome P450 and its enzymes (ethanol increases the activity of certain cytochrome isoenzymes)
Frequently interacting enzyme inhibitors:
1. AB: ciprofloxacin, erythromycin, isoniazid, metronidazole
2. Cardiovascular drugs: amiodarone, diltiazem, quinidine, verapamil
3. Antidepressants: fluoxetine, sertralene
4. Antisecretory drugs: cimetidine, omeprazole
5. Antirheumatic drugs: allopurinol
6. Fungicides: fluconazole, intracanazole, ketoconazole, miconazole
7. Antivirals: indinavir, retonavir, saquinavir
8. Others: disulfiram, sodium valproate
Drugs that give toxic effects in MAO inhibition: adrenomimetics, sympathomimetics, antiparkinsonian, narcotic analgesics, phenothiazines, sedatives, antihypertensive diuretics, hypoglycemic drugs
4) In the process of hatching- more than 90% of drugs are excreted in the urine.
Effect on urine pH and on the degree of drug ionization, on their lipophilicity and their reabsorption
1. interaction during passive diffusion: part of the drug is excreted unchanged, part of the drug is ionized at urine pH 4.6-8.2. Alkalinization of urine is clinically important: poisoning with acetylsalicylic acid or phenobarbital, when taking sulfonamides (reducing the risk of crystalluria), taking quinidine. Increased urine acidity: increased excretion of amphetamine (of practical importance for the detection of this drug in athletes)
2.interaction during the period of active transport: probenezid + penicillin increases the duration of the movement of penicillin, probenecid + salicylates - elimination of the uricosuric action of probenecid, penicillin + CA - a decrease in the excretion of penicillin
Influence of urine composition on drug excretion:
An increase in sugar in urine - an increase in excretion of: vitamin C, chloramphenicol, morphine, isoniazid, glutathione and their metabolites.
B) pharmacodynamic Is the interaction of drugs associated with a change in the pharmacodynamics of one of them under the influence of the other (under the influence of thyroid hormones, the synthesis of b-adrenergic receptors in the myocardium increases and the effect of adrenaline on the myocardium increases).
Examples of clinically significant undesirable synergistic interactions:
NSAIDs + varvarine - increased risk of bleeding
Alcohol + benzodiazepines - potentiation of the sedative effect
ACE inhibitors + K + -saving diuretics - increased risk of hyperkalemia
Verapamil + b-blockers - bradycardia and asystole
Alcohol is a strong inducer of microsomal enzymes, leads to the development of tolerance to drugs (especially to anesthetic and hypnotics), increases the risk of drug dependence.
43. Drug interaction. Antagonism, synergy, their types. The nature of the change in the effect of drugs (activity, effectiveness) depending on the type of antagonism.
With the interaction of drugs, the following conditions may develop: a) enhancement of the effects of a combination of drugs b) weakening of the effects of a combination of drugs c) drug incompatibility
Strengthening the effects of a combination of drugs is implemented in three ways:
1) Summation of effects or additive interaction- view drug interactions in which the effect of the combination is equal to the simple sum of the effects of each of the drugs separately. Ie. 1+1=2 ... Typical for drugs from one pharmacological group that have a common target of action (acid-neutralizing activity of a combination of aluminum and magnesium hydroxide is equal to the sum of their acid-neutralizing abilities separately)
2) synergism - a type of interaction in which the effect of a combination exceeds the sum of the effects of each of the substances taken separately. Ie. 1+1=3 ... Synergy can relate to both the desired (therapeutic) and undesirable effects of drugs. The combined administration of the thiazide diuretic dichlothiazide and the ACE inhibitor enalapril leads to an increase in the hypotensive effect of each of the drugs, which is used in the treatment of hypertension. However, the simultaneous administration of aminoglycoside antibiotics (gentamicin) and the loop diuretic furosemide causes a sharp increase in the risk of ototoxic action and the development of deafness.
3) potentiation is a type of drug interaction in which one of the drugs, which in itself does not have this effect, can lead to a sharp increase in the effect of another drug. Ie. 1+0=3 (clavulanic acid does not have an antimicrobial effect, but it can enhance the effect of the b-lactam antibiotic amoxicillin due to the fact that it blocks b-lactamase; adrenaline does not have a local anesthetic effect, but when added to the ultracaine solution, it sharply lengthens its anesthetic effect by slowing down absorption anesthetic from the injection site).
Attenuating Effects Drugs when used together are called antagonism:
1) Chemical antagonism or antidote- chemical interaction of substances with each other with the formation of inactive products (chemical antagonist of iron ions deferoxamine, which binds them into inactive complexes; protamine sulfate, the molecule of which has an excess positive charge - a chemical antagonist of heparin, the molecule of which has an excess negative charge). Chemical antagonism underlies the action of antidotes (antidotes).
2) Pharmacological (direct) antagonism- antagonism caused by the multidirectional action of 2 medicinal substances on the same receptors in the tissues. Pharmacological antagonism can be competitive (reversible) and non-competitive (irreversible):
A) competitive antagonism: a competitive antagonist reversibly binds to the active center of the receptor, i.e. shields it from the action of the agonist. Since the degree of binding of a substance to a receptor is proportional to the concentration of this substance, the effect of a competitive antagonist can be overcome by increasing the concentration of the agonist. It will displace the antagonist from the active site of the receptor and induce a full tissue response. That. a competitive antagonist does not alter the maximum effect of the agonist, but a higher concentration is required for the agonist to interact with the receptor. Competitive antagonist Shifts the dose-response curve for the agonist to the right relative to the initial values and increases the EC50 for the agonist without affecting the E value Max.
Competitive antagonism is often used in medical practice. Since the effect of a competitive antagonist can be overcome if its concentration falls below the level of the agonist, during treatment with competitive antagonists it is necessary to constantly maintain its level sufficiently high. In other words, the clinical effect of a competitive antagonist will depend on its elimination half-life and the concentration of the full agonist.
B) non-competitive antagonism: a non-competitive antagonist binds almost irreversibly with the active center of the receptor or interacts in general with its allosteric center. Therefore, no matter how the concentration of the agonist increases, it is not able to displace the antagonist from its connection with the receptor. Since some of the receptors that are associated with a non-competitive antagonist are no longer able to be activated , the value of EMax decreases, the affinity of the receptor for the agonist does not change, so the EC50 value remains the same. On the dose-effect curve, the action of a non-competitive antagonist manifests itself as a compression of the curve relative to the vertical axis without shifting it to the right.
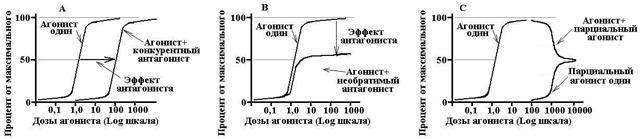
Scheme 9. Types of antagonism.
A - the competitive antagonist shifts the dose-effect curve to the right, that is, it reduces the tissue sensitivity to the agonist without changing its effect. B - a noncompetitive antagonist reduces the magnitude of the tissue response (effect), but does not affect its sensitivity to the agonist. C - a variant of using a partial agonist against the background of a full agonist. As the concentration increases, the partial agonist displaces the complete one from the receptors and, as a result, the tissue response decreases from the maximum response to the full agonist, to the maximum response to the partial agonist.
Non-competitive antagonists are used less frequently in medical practice. On the one hand, they have an undoubted advantage, since their effect cannot be overcome after binding to the receptor, and therefore does not depend on the half-elimination period of the antagonist or on the level of the agonist in the body. The effect of a non-competitive antagonist will be determined only by the rate of synthesis of new receptors. But on the other hand, if an overdose of this medication occurs, it will be extremely difficult to eliminate its effect.
|
Competitive antagonist |
Non-competitive antagonist |
|
Similar in structure to an agonist |
Structurally different from an agonist |
|
Binds to the active center of the receptor |
Binds to the allosteric site of the receptor |
|
Shifts the dose-response curve to the right |
Shifts the dose-response curve vertically |
|
The antagonist reduces tissue sensitivity to the agonist (EC50), but does not affect the maximum effect (Emax) that can be achieved at a higher concentration. |
The antagonist does not alter the tissue sensitivity to the agonist (EC50), but decreases the internal activity of the agonist and the maximum tissue response to it (Emax). |
|
Antagonist action can be reversed with a high dose of the agonist |
The action of the antagonist cannot be reversed with a high dose of the agonist. |
|
The effect of the antagonist depends on the dose ratio of the agonist and the antagonist |
The effect of the antagonist depends only on its dose. |
Losartan is a competitive antagonist against the AT1 receptors of angiotensin; it disrupts the interaction of angiotensin II with receptors and helps to lower blood pressure. The effects of losartan can be overcome by administering a high dose of angiotensin II. Valsartan is a non-competitive antagonist for the same AT1 receptors. Its effect cannot be overcome even with the administration of high doses of angiotensin II.
Interesting is the interaction that takes place between the full and partial receptor agonists. If the concentration of the full agonist exceeds the level of the partial one, then the maximum response is observed in the tissue. If the level of the partial agonist begins to rise, it displaces the full agonist from binding to the receptor, and the tissue response begins to decrease from the maximum for the full agonist to the maximum for the partial agonist (i.e., the level at which it occupies all receptors).
3) Physiological (indirect) antagonism- antagonism associated with the influence of 2 medicinal substances on various receptors (targets) in tissues, which leads to a mutual weakening of their effect. For example, physiological antagonism is observed between insulin and adrenaline. Insulin activates insulin receptors, as a result of which the transport of glucose into the cell increases and the level of glycemia decreases. Epinephrine activates the b2-adrenergic receptors of the liver, skeletal muscles and stimulates the breakdown of glycogen, which ultimately leads to an increase in glucose levels. This type of antagonism is often used in the emergency care of patients with an insulin overdose that has led to hypoglycemic coma.
44. Side and toxic effects of drugs. Teratogenic, embryotoxic, mutagenic effects of drugs.
Side effects- those effects that occur when substances are used in therapeutic doses and constitute the spectrum of their pharmacological action (the analgesic morphine in therapeutic doses causes euphoria) can be primary and secondary:
A) primary side effects - as a direct consequence of the effect of this drug on a certain substrate (hyposalivation when using atropine to eliminate bradyarrhythmia)
B) secondary side effects - indirectly occurring adverse effects (AB, suppressing normal microflora, can lead to superinfection)
Toxic effects- undesirable effects manifested in this drug when it leaves the therapeutic range (drug overdose)
The selectivity of the drug action depends on its dose. The higher the dose of the drug, the less selective it becomes.
Teratogenic action- the ability of drugs, when administered to a pregnant woman, to cause anatomical anomalies of fetal development (thalidomide: phocomelia, antiblastoma drugs: multiple defects)
Embryotoxic action- adverse effects not associated with organogenesis disorders in the first three months of pregnancy. At a later date, it appears Fetotoxic action.
Mutagenic effect of drugs- damage to the germ cell and its genetic apparatus of drugs, which is manifested by a change in the genotype of the offspring (adrenaline, cytostatics).
Carcinogenic effect of drugs- the ability of some drugs to induce carcinogenesis.
45. Medical and social aspects of combating drug dependence, drug addiction and alcoholism. The concept of substance abuse.
« It is unlikely that humanity as a whole will ever do without an artificial paradise. Most men and women lead such a painful life that in best case so monotonous, miserable and limited that the desire to "get away" from her, to disconnect at least for a few moments, is and has always been one of the main Wished Ny soul"(Huxley, work" The Doors of Perception ")
1) Drug addiction- a state of mind and / or a physical state, which is a consequence of the effect on the body of drugs and is characterized by specific behavioral reactions, it is difficult to overcome the desire to re-take drugs in order to achieve a special mental effect or to avoid discomfort in the absence of drugs in the body. Drug dependence is characterized by:
BUT) Psychological addiction- the development of emotional distress when you stop taking drugs. A person feels empty, plunges into depression, experiences a feeling of fear, anxiety, his behavior becomes aggressive. All these psychopathological symptoms arise against the background of thoughts about the need to inject yourself with drugs that have caused addiction. The desire to take drugs can range from a simple desire to a passionate thirst for taking drugs, which absorbs all other needs and turns into the meaning of a person's life. It is believed that psychological dependence develops when a person becomes aware that he can achieve optimal well-being solely through the introduction of drugs. The basis of psychological dependence is a person's belief in the action of the drug (cases of the development of psychological dependence on placebo are described in the literature).
B) Physical addiction- violation of the normal physiological state of the body, which requires the constant presence of drugs in it to maintain a state of physiological balance. Stopping the medication causes the development of a specific symptom complex - withdrawal syndrome - a complex of mental and neurovegetative disorders in the form of a dysfunction in the direction opposite to that which is characteristic of the action (morphine eliminates pain, depresses the respiratory center, narrows the pupils, causes constipation; with withdrawal symptoms, the patient develops excruciating pain, frequent noisy breathing, pupils are dilated and persistent diarrhea develops)
IN) Tolerance... Tolerance to drugs that cause drug dependence is often cross-cutting, that is, it arises not only to a given chemical compound, but also to all structurally similar compounds. For example, in patients with drug dependence to morphine, tolerance arises not only to it, but also to other opioid analgesics.
For the development of drug dependence, the presence of all 3 criteria is not a necessary condition; Table 3 shows the main types of drug dependence and its constituent components.
Opioids, barbiturates, alcohol cause strong physical and psychological dependence and tolerance. Anxiolytics (diazepam, alprazolam) predominantly cause psychological dependence.
2) Addiction (drug addiction)- This is an extremely severe form of drug dependence, compulsive use of drugs, characterized by an ever-increasing, irresistible urge to administer this drug, increasing its dose. Desire compulsiveness means that the patient's need to administer the drug dominates all other (even vital) needs. From the standpoint of this definition, craving for morphine is drug addiction, while craving for nicotine is drug dependence.
3) Addicted to medicine- characterizes a less intense urge to take medications, when refusal from the medication causes only a feeling of mild discomfort, without the development of physical dependence or a detailed picture of psychological dependence. That. addiction encompasses that part of drug addiction that does not fit the definition of addiction. For example, the aforementioned drug addiction to nicotine is a form of addiction.
4) Drug abuse- unauthorized use of drugs in such doses and in such ways that differ from the accepted medical or social standards in a given culture and at a given time. That. drug abuse covers only the social aspects of drug use. An example of abuse is the use of anabolic steroids in sports or to improve physique by young men.
5) Alcoholism- chronic abuse of alcohol (ethyl alcohol), leading nowadays to damage to a number of organs (liver, gastrointestinal tract, central nervous system, cardiovascular system, immune system) and accompanied by psycho-physical dependence.
6) Substance abuse- chronic abuse of various drugs (including drugs, alcohol, hallucinogens), manifested by a variety of mental and somatic disorders, behavioral disorders, social degradation.
Drug addiction treatment difficult and thankless task. Until now, no effective method has been created that would ensure the success of treatment in more than 30-40% of patients. Achievement of any noticeable results is possible only with the full cooperation of the efforts of the patient, the doctor and the social environment in which the sick person is (the principle of voluntariness and individuality). Modern techniques are based on the following principles:
ü psychotherapeutic and occupational therapy methods;
ü group treatment and rehabilitation (society of alcoholics anonymous, drug addicts)
ü gradual or abrupt withdrawal of the drug against the background of detoxification therapy
ü carrying out substitution therapy (replacement of a narcotic drug with slow and long-acting analogues with their subsequent cancellation; for example, the so-called methadone substitution therapy program for heroin addicts)
ü treatment with specific antagonists (naloxone and naltrexone) or sensitizing agents (teturam)
ü neurosurgical methods of cryodestruction of the cingulate gyrus and hippocampus
47. Types of pharmacotherapy. Deontological problems of pharmacotherapy.
Pharmacotherapy (FT) - a set of treatment methods based on the use of drugs. The main types of FT:
1.etiotropic PT - correction and elimination of the cause of the disease (AB in infectious diseases)
2.pathogenetic FT - impact on the mechanism of disease development (ACE inhibitors in hypertension)
3.symptomatic FT - elimination of the symptoms of the disease if it is impossible to influence its cause or pathogenesis (NSAIDs for influenza)
4.Substitution FT - the use of drugs in case of insufficiency of natural biologically active substances (insulin in diabetes)
5.prophylactic FT (vaccines, serums, acetylsalicylic acid for ischemic heart disease)
Society's attitude to drugs on the present stage : 1) desire to get benefits without risk 2) hope for a miracle, visions 3) lack of understanding of the risk of drug use 4) indignation and "righteous indignation", hasty drug assessments 5) desire to get new drugs
Doctor's attitude to drugs: therapeutic optimism (reliance on drugs as a powerful component of therapy), therapeutic nihilism (denial of new drugs, adherence to certain drugs, distrust of new drugs)
Compliance (adherence) of the patient to treatment 1) understanding the doctor's instructions and treatment goals 2) striving to follow the doctor's prescriptions exactly.
Currently, there are about 100,000 drugs in the world, more than 4,000 are registered in the Republic of Belarus, of which about 300 are vital drugs. The study of pharmacology helps not to drown in the sea of drugs.
48. Basic principles of treatment and prevention of drug poisoning. Antidote therapy.
Classification of toxic substances (OM):
1. By belonging to certain classes of chemical compounds: barbiturates, benzodiazepines, cyanides.
2. By origin: non-biological nature (acids, alkalis, salts of heavy metals), toxic waste products of some MB (botulinum toxin), plant origin (alkaloids, glycosides), animal origin (snake and bee venoms)
3. According to the degree of toxicity: a) extremely toxic (DL50< 1 мг/кг) б) высоко токсические (1-50) в) сильно токсические (50-500) г) умеренно токсические (500-5000) д) мало токсические (5000-15000) е) практически нетоксические (> 15.000)
4. By toxicological action: a) nerve-paralytic (bronchospasm, suffocation) b) skin-resorptive c) general toxic (hypoxic convulsions, coma, paralysis) d) suffocating e) lacrimal and irritating e) psychotropic (impaired mental activity, consciousness)
5. Depending on the area of preferential use: industrial poisons, pesticides, household poisons, chemical warfare agents, medicinal substances.
6. Depending on the toxicity of drugs: List A - drugs, the purpose, use, dosing and storage of which, due to their high toxicity, should be done with great care. The same list includes drugs that cause drug addiction; list B - drugs, the appointment, use, dosing and storage of which should be carried out with caution in connection with possible complications when using them without medical supervision.
Selectively toxic effect of drugs.
A) cardiotoxic: cardiac glycosides, potassium supplements, antidepressants
B) neurotoxic: psychopharmacological agents, oxyquinolines, aminoglycosides
B) hepatotoxic: tetracyclines, chloramphenicol, erythromycin, paracetamol
D) nephrotoxic: vancomycin, aminoglycosides, sulfonamides
E) gastroenterotoxic: steroid anti-inflammatory drugs, NSAIDs, reserpine
E) hematotoxic: cytostatics, chloramphenicol, sulfonamides, nitrates, nitrites
G) pneumotoxic
Toxicokinetics - studies the absorption, distribution, metabolism and excretion of drugs taken in toxic doses.
The entry of toxic substances into the body is possible a) enterally b) parenterally. The speed and completeness of absorption reflects the rate of development of the toxic effect and its severity.
Distribution in the body: Vd = D / Cmax - the actual volume in which the poisonous substance is distributed in the body. Vd> 5-10 l / kg - OM is difficult to allow for its removal (antidepressants, phenothiazines). Vd< 1 л/кг – ОВ легче удалить из организма (теофиллин, салицилаты, фенобарбитал).
Overdose- changes in pharmacokinetic processes: solubility, connection with proteins, metabolism ® significant increase in the free fraction of drugs ® toxic effect.
The kinetics of the first order with an increase in the concentration of the drug transforms into the kinetics of the zero order.
The toxigenic stage is detoxification therapy, the somatogenic stage is symptomatic therapy.
Toxicodynamics . The main mechanisms of toxic action:
A) mediator: direct (by the type of competitive blockade - FOS, psychomimetics) and indirect (activators or inhibitors of enzymes)
B) interaction with biomolecules and intracellular structures (hemolytic substances)
C) metabolism by the type of lethal synthesis (ethyl alcohol, thiophos)
D) enzymatic (snake venoms, etc.)
Types of action: local, reflex, resorptive.
Poisoning classification:
1. Etiopathogenetic:
a) accidental (self-medication, mistaken reception)
b) deliberate (with the aim of suicide, murder, development of a helpless state in the victim)
2. Clinical:
a) depending on the rate of development of poisoning: acute (intake of a single dose or with a short time interval of a toxic dose of a substance), subacute (delayed development of the clinical picture after a single dose), chronic
b) depending on the manifestation of the main syndrome: damage to the CVS, damage to the DS, etc.
c) depending on the severity of the patient's condition: mild, moderate, severe, extremely severe
3. Nosological: takes into account the name of the drug, the name of the group of substances
General mechanism of death in case of poisoning:
A) defeat of the CVS:
1) lowering blood pressure, hypovolemia of peripheral vessels, collapse, brady - or tachycardia (tricyclic antidepressants, beta-blockers, calcium channel blockers)
2) arrhythmias (ventricular tachycardia, fibrillation - tricyclic antidepressants, theophylline, amphetamine)
B) damage to the central nervous system: stupor, coma ® respiratory depression (drugs, barbiturates, alcohol, hypno-sedative drugs)
C) convulsions, muscle hyperreactivity and rigidity ® hyperthermia, myoglobinuria, renal failure, hyperkalemia
Toxicological triad:
1) duration of use, dose and substance ® history.
2) assessment of the state of consciousness by symptoms: respiration, blood pressure, body temperature
3) laboratory data
Basic principles of treatment:
I. First aid: artificial respiration, heart massage, anti-shock therapy, control of water-electrolyte balance
II... Delayed absorption and removal of non-absorbed OM from the body:
Purpose: to end contact with OV
1. Parenteral route:
a) through the lungs:
1) stop inhalation
2) irritating substances (ammonia, formaldehyde) ® to consolidate active movements, warm up, give oxygen and antifoam agents (for ammonia, the defoamer is vinegar, and for formaldehyde, a diluted solution of ammonia)
b) through the skin: wash off with a copious amount of warm water with soap or detergent, specific antidotes, neutralize and stop the exposure of the OM to the skin (FOS: wash with water, remove with 10-15% ammonia or 5-6% sodium bicarbonate solution with water; phenolcresol: vegetable oil or ethylene glycol, but not vaseline oil, KMNO4: 0.5-1% ascorbic acid solution or equal volumes of 3% hydrogen peroxide and 3% acetic acid solution, CCl4, turpentine, gasoline: warm soapy water )
c) when injected into a limb: a tourniquet above the injection site
d) in case of contact with eyes: rinse with warm saline or milk for 10-20 minutes, drip a local anesthetic; in case of contact with acids and alkalis, it cannot be neutralized. Consultation with an ophthalmologist is required.
2. Enteral route: to free the stomach from OM, accelerate the passage
a) removal of OM:
1) preliminary intake of water. Do not take milk (with the exception of caustic poisonous substances) and ethanol (with the exception of methanol).
2) vomiting - indicated mainly in case of poisoning with large tablets or capsules that cannot pass through the probe. Can be provoked by reflex or emetic (NaCl: 1 tablespoon per 1 glass of water; Ipecac syrup: adults 2 tablespoons, children 2 teaspoons; mustard: 1-2 teaspoons per glass of water; apomorphine: 5-10 mg / kg subcutaneously , except for children under 5 years old). Do not induce vomiting after ingestion: organic solvents - danger of inhalation, detergents - foaming, convulsive substances - danger of aspiration, caustic substances - damage to the esophagus)
3) probe gastric lavage - is an emergency and mandatory measure. The stomach is washed if no more than 4-6 hours have passed since the poisoning, sometimes up to 10 hours; in case of poisoning with acetylsalicylic acid - after 24 hours. The patient is pre-intubated with a tube with an inflatable cuff: in a coma in the absence of a cough and laryngeal reflex. The stomach is washed with water or saline solution 30 ° C, the procedure takes 4 hours or more. At the end of the wash, activated carbon and sodium sulfate.
b) decrease in absorption from the gastrointestinal tract: activated charcoal inside after gastric emptying + sodium or magnesium sulfate. Features of measures to reduce absorption:
1) organic solvents: do not induce vomiting, gastric lavage after intubation, activated carbon + liquid paraffin
2) detergents: do not induce vomiting and wash out the stomach, it is necessary to give a lot of water + antifoaming agents (simethicone)
3) acids and alkalis: vomiting cannot be induced, gastric lavage through a tube lubricated with vegetable oil after the administration of a narcotic analgesic is the only indication for giving milk. For acid poisoning - antacids, for alkali poisoning - citric or acetic acid.
III... Removal of absorbed OM from the body
a) forced diuresis (conditions: sufficient renal blood flow and glomerular filtration; pour in-pour out 20-25 liters in 24 hours)
b) peritoneal hemodialysis
c) hemosorption
d) exchange blood transfusion
e) forced hyperventilation
IV... Symptomatic therapy of functional disorders.
Antidotes: 1) toxicotropic - binding, neutralizing and preventing absorption of substances: acting on the principle activated carbon acting on a chemical basis (unitiol, penicillamine, pentacin)
2) toxicokinetic - accelerate the biotransformation of OM (trimedoxime bromide, sodium thiosulfate, ethanol, AO)
3) pharmacological - atropine, naloxone
4) immunological antidotes
Unithiol, succimer - binds heavy metals, metalloids, cardiac glycosides. Esmolol binds theophylline, caffeine. Calcium trisodium pentotate - forms complexes with bivalent and trivalent metals.
49. The recipe and its structure. General rules writing a prescription. State regulation of the rules for prescribing and dispensing drugs.
Recipe- this is a written appeal from a doctor to a pharmacist with a requirement to release the medicine in a certain form and dosage indicating the method of its use
The following parts are distinguished in the recipe:
1. Inscriptio - title, inscription. The date of issue of the prescription, surname, initials and age of the patient, surname and initials of the doctor are written here.
2. Invocatio - contacting a pharmacist. It is expressed by the word “Recipe” (take) or by an abbreviation (Rp.)
3. Designatio materiarum - designation or name of medicinal products with indication of their doses. IN complex recipe the listing of medicinal substances is done in a specific sequence. The first is the main drug substance (basis). Then the adjuvans are written. After that, the ingredients that correct the taste, smell, color of the medicine (corrigens) are indicated. The last to write are the substances that give the drug a certain dosage form (constituens).
4. Subscriptio - prescription (indication) to the pharmacist. It indicates the dosage form, pharmaceutical operations required for its manufacture, the number of dispensed doses of the drug.
5. Signatura - instructing the patient on how to use the medicine.
6. Subscriptio medici - signature of the doctor who wrote the prescription, his personal seal.
A doctor's appeal to a pharmacist, the name of the drugs included in the prescription, the name dosage form and the nature of pharmaceutical operations are written in Latin... The name of medicines, botanical names of plants are written with capital letter... The prescription for the patient is written in Russian or national languages.
General rules for prescribing:
1. The prescription is written on a special form, depending on the prescribed medicine, in clear handwriting, ink or ballpoint pen no fixes.
2. The prescription indicates the date, month, year, surname, name, patronymic and age of the patient, surname, name and patronymic of the doctor. Then comes the text of the recipe, which lists the names of the substances included in the recipe in the genitive case, indicating their amount
3. The unit of mass in recipes is gram or UNIT.
4. If the maximum dose of poisonous and potent substances is exceeded, it is confirmed in words
5. The prescription is confirmed by the signature and personal seal of the doctor
In the Republic of Belarus, there is State regulation of the rules for prescribing and dispensing drugs.
50. Rules for prescribing poisonous, narcotic and potent drugs.
List A includes drugs, the appointment, use, dosing and storage of which, due to their high toxicity, should be carried out with great care. The same list includes drugs that cause drug addiction.
List B includes drugs, the appointment, use, dosing and storage of which should be carried out with caution in connection with possible complications when using them without medical supervision.
For poisonous and potent drugs, the maximum higher single and daily doses have been established. These doses are for adults over 25 years of age. When recalculating doses for people over 60 years old, age sensitivity To different groups LS. Doses of drugs that depress the central nervous system, as well as cardiac glycosides and diuretics are reduced by 50%, the doses of other poisonous and potent drugs are reduced to 2/3 of the adult dose. Doses of AB, sulfonamides and vitamins are usually the same for everyone age groups starting at the age of 25.
1. Narcotic drugs (list A) are prescribed for prescription form Form 2. One form - one medicine. There must be: the signature and seal of the attending physician, the signature of the head physician of the healthcare facility, the round stamp of the healthcare facility.
2. Poisonous drugs (list A), potent (list B) are prescribed on the form 1 prescription form. There must be a signature and personal seal of the doctor, the seal of the healthcare facility.
51. Medicines under control. Prescription drugs.
Narcotic, poisonous and potent drugs are under control (see section 20)
A) Medicines not registered in the Republic of Belarus and not authorized for official use
B) drugs at the request of patients and their relatives without examining the patient and establishing a diagnosis
C) prescriptions for narcotic drugs for injection, anesthetic ether, chloroethyl, pentamine, fluorothane, sodium oxybutyrate in ampoules, lithium oxybutyrate, barium sulfate for fluoroscopy.
52. Pharmacokinetic models (one-chamber and two-chamber), quantitative laws of drug absorption and elimination.
![]() Single chamber model.
Single chamber model.
The whole organism is a single homogeneous container. Assumptions:
1) a rapid dynamic development is established between the content of the drug in the bloodstream and its concentration in extravascular tissues
2) The drug is quickly and evenly distributed throughout the blood volume
3) Elimination of drugs obeys first-order kinetics: the rate of decrease in the drug content in the blood is proportional to its concentration
If the mechanisms for elimination of the drug (biotransformation in the liver, renal secretion) are not saturated with the introduction of a therapeutic dose, a lognormal graph of changes in plasma concentration over time will be linear.
Incline lognormal axis - Kel, where Kel is the rate constant of elimination and has the dimension of time-1. The C0 value is obtained by extrapolating the graph to the intersection with the ordinate axis. Plasma drug concentration(Ct) at any time t after administration into the body is:
Ln Ct = Ln C0 - kt. The elimination constant Kel, Vd, and the total clearance (CL) are related by the expression: CL = k × Vd
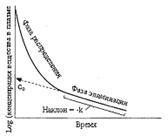 Two-chamber model.
Two-chamber model.
Often, after the drug enters the body, it is not possible to quickly achieve a balance between the drug content in the blood and its concentration in the extravascular fluid. Then it is believed that in the aggregate of tissues and biological fluids of the body, two chambers can be distinguished, which differ in the degree of accessibility for the penetration of drugs. The central chamber includes blood (often with intensively perfused organs - liver, kidneys), the peripheral chamber - interstitial fluid internal organs and fabrics.
The resulting graph shows the initial The distribution phase ( The time required for the drug to reach an equilibrium state between the central and peripheral chambers and the following slow Elimination phase First order.
C0 value, obtained by extrapolation Elimination phases before crossing the ordinate. C0 is used to calculate the volume of distribution and the elimination constant. The formulas for calculating Ct and Cl given for the single chamber model are also applied during the elimination phase for drugs that satisfy the conditions of the two chamber model.
53. Selectivity and specificity of drug action. Therapeutic, side and toxic effects of drugs, their nature from the standpoint of the concept of receptors. A therapeutic strategy for combating side and toxic effects of drugs.
Specificity- this is when a drug binds to a type of receptor that is strictly specific to it.
Selectivity- this is when a drug is able to bind to one or more types of receptors more accurately than others.
It is more preferable to use the term selectivity, since it is unlikely that any drug molecule can bind to only one type of receptor molecule, since the number of potential receptors in each patient is of astronomical significance.
Therapeutic action- the main desired pharmacological effect expected from a given pharmacological preparation.
Side effects- those effects that occur when substances are used in therapeutic doses and constitute the spectrum of their pharmacological action.
Toxic effects- undesirable effects manifested in this drug when it leaves the therapeutic range.
Relationships between the therapeutic and toxic effects of drugs based on the analysis of receptor-effector mechanisms:
1) therapeutic and toxic effects mediated by the same receptor-effector mechanism (prazosin acts as an alpha-selective antagonist on vascular SMC receptors and has a hypotensive effect in essential hypertension, but at a high dose, the patient may experience postural hypotension)
2) therapeutic and toxic effects mediated by identical receptors, but different tissues or different effector pathways (cardiac glycosides are used to increase myocardial contractility, at the same time they disrupt the function of the gastrointestinal tract, vision due to blockade of Na + / K + -ATPase of the cell membrane)
3) therapeutic and toxic effects mediated by various types of receptors (for example, norepinephrine has a hypertensive effect through a1-Ap, but at the same time causes tachycardia through b1-Ap)
Therapeutic strategy to combat the therapeutic and side effects of drugs:
1. The drug should always be administered in the lowest dose that produces an acceptable therapeutic effect.
2. Reduction of the dose of one drug due to the appointment of another drug with a similar effect, but through different receptors and with a different toxicity profile.
3. The selectivity of the drug action can be increased by controlling the drug concentration in the region of the receptors of various parts of the body (local use of drugs - inhalation use of salbutamol in bronchial asthma)
