The structure of the hip joint. Anatomical and functional features of the hip joint
Traumatic dislocation of the hip dislocations of the shoulder, forearm and clavicle are much less common, but more often dislocations of the hand, lower leg and foot bones. Their frequency fluctuates within 5-20% and is largely explained by anatomical and physiological features, the knowledge of which acquires significant practical value.
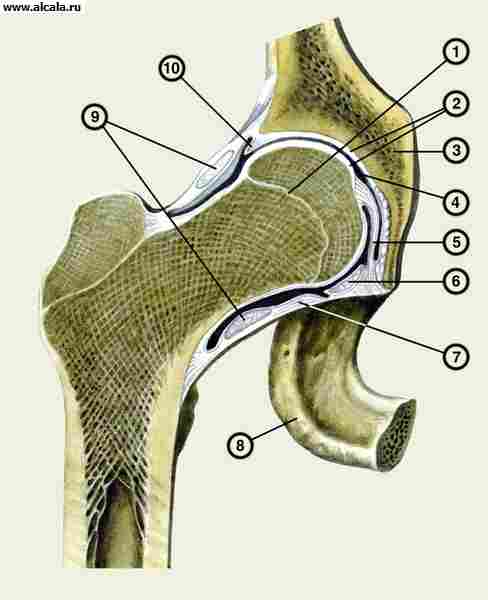
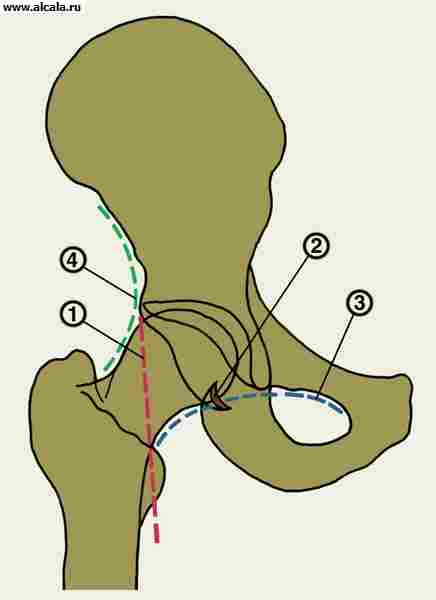
Hip joint(Fig. 109) is not only the largest, but also the most complex in its anatomical structure. It is formed by the articular surface of the femoral head, which, along its entire length, with the exception of a small depression located in the center, the place of attachment of the round ligament, is covered with hyaline cartilage and an acetabulum, which is covered only along the peripheral part of the semilunar surface. The lower central part of the acetabulum is devoid of cartilage. It is made of fatty tissue and covered with a synovial membrane. At the postero-lower edge of it there is a notch, over which the transverse ligament of the acetabulum is stretched. The articular cavity is formed by the fusion of the 3 pelvic bones. Its upper edge is the ilium, the inner one is the pubic and the lower one is the ischium. This is important to consider when locating the head in case of dislocation. The cartilaginous lip of the acetabulum, attaching itself along the entire free edge of the cavity and reaching a height of 0.5-0.6 cm, further increases the depth of the acetabulum, which on average reaches 3 cm with a width of 4.5 cm. In its shape, the acetabulum resembles half of the ball, and the head of the femur is about two-thirds of it. This anatomical ratio allows the femoral head to sink more than half deep into the acetabulum cavity, providing reliable protection against mechanical stress and good support for the lower limb. The congruence of the articular surfaces and the almost complete correspondence between the size and shape of the head, on the one hand, the shape, capacity and depth of the acetabulum, on the other, allow them to be transferred from the category of predisposing factors to those protecting the joint from possible dislocations.
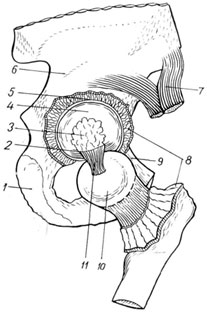
1 - os ischii;
2 - lig. Transversum acetabuli;
3 - fossa acetabuli is filled with adipose tissue;
4 - facies lunata;
5 - labrum acetabulare;
6 - os ilium
7 - m.rectus femoris;
8 - capsula articularis;
9 - os pubis;
10 - caput femoris;
11 - lig. Pubofemorale
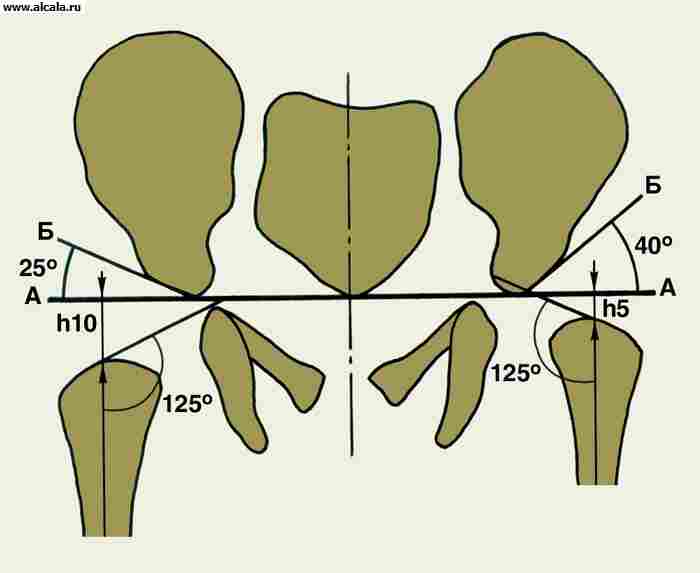
It should be borne in mind that the axis of the head and the neck, forming a cervico-diaphyseal angle of 125-127 ° in the frontal plane with the diaphyseal part of the femur, do not coincide. The axis of the head and neck is most often deflected anteriorly and less often posteriorly. Moreover, the angle of this deviation varies widely (from 10 to 22 °).
Joint capsule represents a very dense fibrous formation. Starting around the circumference of the bony edge of the acetabulum, it goes to the proximal end of the thigh and attaches in front to the intertrochanteric line, and posteriorly - somewhat proximal to the intertrochanteric crest. Because of this, the anterior surface of the femoral neck is completely in the joint cavity, and the posterior surface is only 2/3 of its surface. The helical direction of the capsule and its tight fit to the neck, on the one hand, as it were, screws the head into the cavity of the acetabulum, which protects it from damage, and on the other hand, it significantly limits the capacity of the hip joint (up to 15-20 ml), which causes sharp pain even with minor hemorrhages in the joint cavity. The superficial bundles of the outer fibrous layer of the capsule have a longitudinal direction, and the deeper bundles, intertwining with each other, create additional strength for the thinner synovial layer, at the places of attachment of which folds are formed, softening mechanical influences directed to the articular ends.
The strength of the joint capsule is not the same in different areas. Some of them have very strong reinforcement by the surrounding ligaments, while others do not have this reinforcement. The most important are those ligaments that approach the capsule from the side of the pelvic bones.
Iliofemoral ligament located on the front surface of the hip joint (Fig. 110). Starting with its wide base at the lower edge of the anterior-inferior iliac spine, it is directed in a fan-like manner downward and outward, with a lateral bundle attached to the greater trochanter and the upper part of the intertrochanteric line, creating a kind of overhang over the joint, and the medial, going more vertically, crossing the anterior section joint, attaches to the lesser trochanter and the lower part of the intertrochanteric line. The specified bond is the strongest. It limits hip extension, adduction and external rotation of the hip and takes part in keeping the trunk in a standing position.
The other two ligaments also have a helical direction. The pubo-femoral ligament extends from the superior branch of the pubic bone downward and laterally, woven into the joint capsule, and ends in its bundles at the inner edge of the intertrochanteric line. It limits extension, abduction, and internal rotation of the hip.
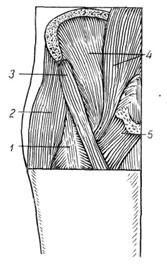
Ischio-femoral ligament reinforces the posterior part of the capsule (Fig. 111). It begins on the anterior surface of the body of the ischium, spirals over to the posterior surface, then the upper one, partially weaves into the joint capsule and reaches the bottom of the trochanteric fossa. This ligament limits adduction and internal rotation of the thigh. The fibers of these ligaments partially pass into the circular ligament, which is located in the thickness of the capsule and in the form of a loop covers the middle part of the femoral neck, heading towards the lower iliac spine.
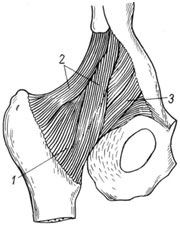
1 - capsula articularis
2 - lig. ileofemorale;
3 - lig. pubofemorale

1 - lig. ischiofemorale;
2 - lig. iliofemorale;
3 - capsula articularis
The helical direction of the ligaments of the hip joint, like the capsule itself, significantly increases its strength. However, the joint capsule also has its weak points. They are located at the anterior-inner edge, between the ilio-femoral and pubic-femoral ligaments, at the lower edge, near the obturator foramen, between the ischio-femoral and pubic-femoral and posteriorly between the ilio-femoral and ischio-femoral ligaments. These portions of the capsule are devoid of reinforcing ligaments. They are the weakest, and when they rupture, the femoral head leaves the joint cavity.
The hip joint is protected from all sides by powerful muscles (Fig. 112), which are directly adjacent to the joint capsule. The antero-outer surface of the joint is covered by the rectus femoris muscle, the lumbosacral and scallop muscles. More superficially is the muscle that strains the fascia lata of the thigh, and the sartorius muscle. These muscles have a longitudinal direction and when the hip is extended, straining, they fit tightly to the joint, especially the lumbar-iliac muscle, which covers almost the entire anterior part of the joint, and when flexed, they relax, which entails the loss of the function of protecting the joint from possible dislocation of the head anteriorly ... The back and partly the lower part of the joint is covered by muscles (Fig. 113), which run transversely. They are all relatively short and are attached in the region of the greater trochanter. The gluteus maximus muscle is adjacent to the upper edge of the capsule, the piriformis muscle is located slightly below, which almost completely overlaps the joint capsule. The middle layer is made up of the internal obturator muscle, the twins, the square muscle of the thigh and the gluteus medius muscle, and the superficial one is the gluteus maximus muscle. These muscles press the thigh against the acetabulum, and when it is dislocated, the head either pushes the muscles apart or breaks them.
112. Topography of the muscles of the hip joint in front:
1 - m. rectus femoris;
2 - m. tensor fasciae latae;
3 - m. sartorius;
4 - m. iliopsoas;
5 - m. pectineus
![]()
113. Topography of the muscles of the hip joint from behind:
1 - m. gluteus maximus
2 - m. gluteus medius;
3 - m. gluteus minimus;
4 -m. pyriformis;
5 - m. obturatorius internus;
6 - m. quadrates femoris;
7 - mm. gemlli
Numerous terminal vascular branches serve as sources of blood supply. An essential role in this is played by the medial circumflex artery of the thigh, as well as the ascending branch of the lateral circumflex artery of the thigh. These vessels freely anastomose, providing nutrition to the joint capsule, and through it the femoral neck. Type a vessels are also well developed here. nutritiae, as well as branches of the inferior gluteal artery extending from the intertrochanteric region. The branch of the obturator artery, which penetrates into the joint cavity under the transverse ligament, also takes part in the blood supply to the joint. The blood supply to the femoral head is much worse. Apparently, this explains the often arising aseptic necrosis of it, especially with chronic dislocations.
The innervation of the antero-external part of the joint is carried out by the branches of the femoral nerve, the antero-internal obturator and posterior - by the branches of the sciatic and upper gluteal nerves.
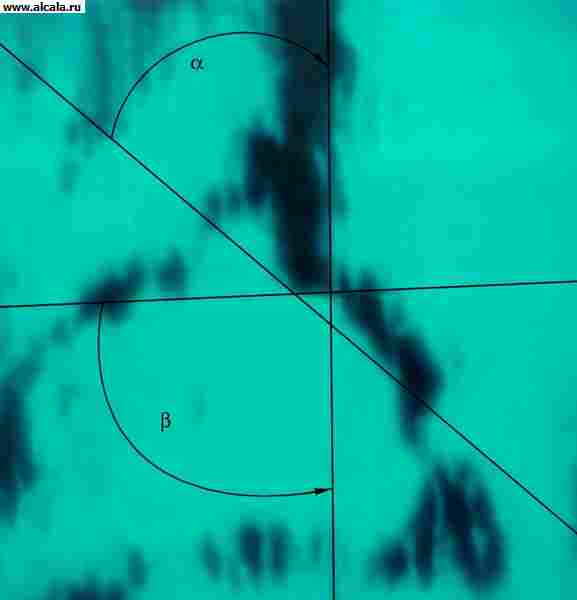
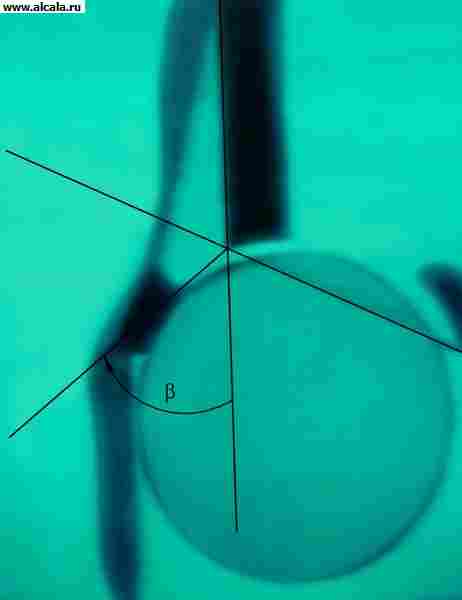
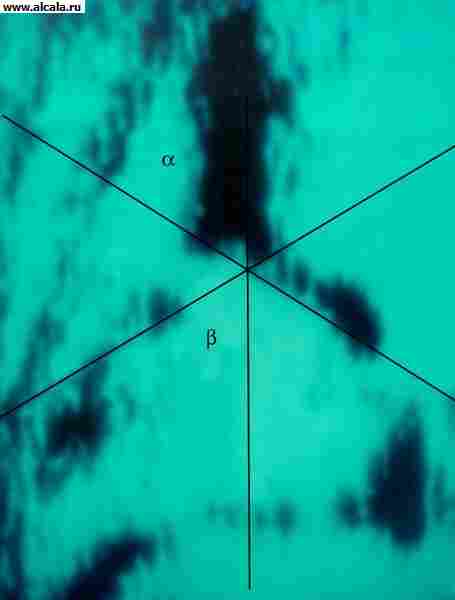
Hip joint refers to walnut, being a type of polyaxial spherical joints. It has 3 degrees of freedom of movement around 3 main axes (Fig. 114). Flexion and extension are performed around the frontal axis, abduction and adduction around the sagittal axis, and external and internal rotation around the vertical axis. Moreover, the rotational movements are performed in an arc of 49 ° (external rotation - by 13 °, and internal - by 36 °), and in the position of flexion of the thigh and lower leg at a right angle, their amplitude reaches 90 °.
Fig. 114 Range of motion in the hip joint: 1 - extension, 2 - flexion, 3 - internal rotation, 4 - external rotation
Movements in the sagittal plane are performed in an arc of 105-180 °, and in the frontal plane, flexion is possible until the front surface of the thigh touches the anterior abdominal wall, and overextension is up to 10-15 °. Movement in the hip joint is possible in all directions and in a large volume. However, in life, such a large functional capacity, which would put the hip joint in any forced position conducive to dislocation, is rarely used, since there is no need for this, that is, in this joint, large functionality does not correspond to their needs, which to a large extent reduces the likelihood of traumatic dislocations.
Atlas of traumatic dislocations. M.I. Sinilo, 1979
formed by the acetabulum of the pelvic and the head of the femur. A fibro-cartilaginous lip passes along the edge of the acetabulum, due to which the congruence of the articular surfaces increases. T. p. reinforced by the intra-articular ligament of the femoral head, as well as by the transverse ligament of the acetabulum, covering the femoral neck ( rice. 12 ). Outside, the powerful ilio-femoral, pubic-femoral and sciatic-femoral ligaments are interwoven into the capsule. T. p. - a kind of spherical (so-called cup-shaped) joint. In it, movements are possible: around the frontal axis (flexion and extension), around the sagittal axis (abduction and adduction), around the vertical axis (external and internal rotation).
Blood supply T. with. it is carried out through the arteries that bend around the femur, by the branches of the obturator and (non-permanently) by the branches of the superior perforating, gluteal and internal genital arteries. The outflow of blood occurs through the veins surrounding the femur into the femoral vein and through the obturator veins into the iliac vein. Lymphatic drainage is carried out into the lymph nodes located around the external and internal iliac vessels. T. p. innervated by the femoral, obturator, sciatic, superior and inferior gluteal and genital nerves.
Research methods
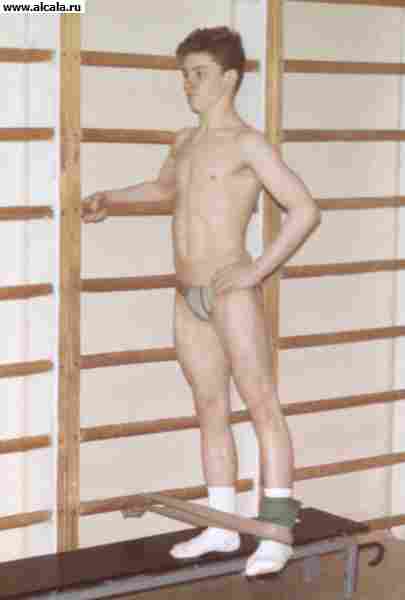
In an upright position, the patient's posture and gait, the severity of lumbar lordosis, the position of the limbs in relation to the pelvis and their length are checked. For example, with bilateral congenital hip dislocation, compensatory hyperlordosis may occur. Determine the presence of the Trendelenburg symptom, which is noted in violation of the support of the lower limb and weakness of the gluteal muscles - in a standing position on a sore leg and bent in the hip and knee joints, the other pelvis tilts towards the healthy side and the gluteal fold is located lower.
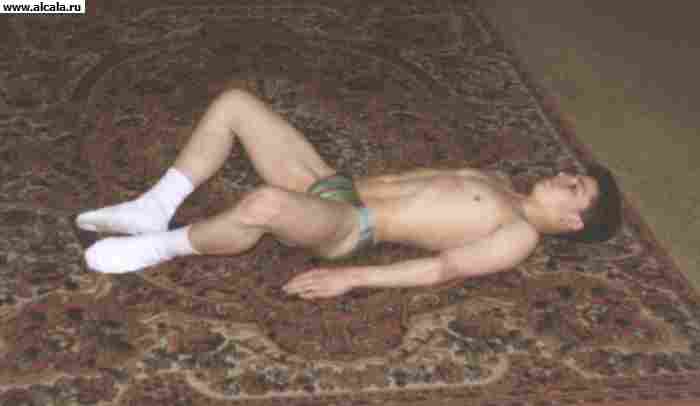
In the position of the patient on the back, the true position of the limb is established on the side of the lesion (in this case, it is necessary to eliminate hyperlordosis by bending in the hip and knee joints of the opposite limb).
The volume of active and passive movements in the hip joints is checked. Palpation determines the position of the greater trochanters. Normally, they are located symmetrically at the level of the Roser - Nelaton line, connecting the superior anterior iliac spine and the sciatic tubercle. When the greater trochanter is displaced upward, the symmetry of the arrangement of Shemaker's lines is also violated (they are drawn from the greater trochanter through the upper anterior iliac spine on each side to the intersection with the midline of the abdomen) and the isosceles of the Bryant triangle. The construction of the latter is carried out as follows: on a line that is a continuation of the axis of the thigh and passes along its outer surface through the greater trochanter, a perpendicular descends from the superior anterior iliac spine; the second line connects the superior anterior iliac spine and the apex of the greater trochanter. Normally, the distance from the apex of the greater trochanter to the point of intersection of the perpendicular with the line that is the continuation of the thigh axis is equal to the length of the lowered perpendicular. In newborns, in addition to measuring the length of the lower extremities and determining the range of motion in the hip joints, it is necessary to check the depth and symmetry of the inguinal, femoral and gluteal folds.
A significant role in the diagnosis of lesions of T. s. plays x-ray examination. Due to the fact that in the formation of T. s. bones with an irregular shape are involved, the X-ray projection image depends on the patient's positioning (Fig. 3). The correct placement is checked by the uniformity of the contours of the obturator openings, the symmetry of the position of the sacral openings, the uniformity of the X-ray slit of the sacroiliac joints and the size of the wings of the iliac bones. It is also necessary to take into account the age-related characteristics associated with the structural transformations of the bones that form the hip joint.
The head of the femur in newborns is cartilaginous. The nucleus of ossification appears in the first half of the year (by 4-6 months), increasing by about 10 times by the age of 5-6 years. The growth of the femoral neck lasts up to 18-20 years. In the first year of life, the cervico-diaphyseal angle averages 140 °. The acetabulum is formed by the ilium, pubic and ischial bones and the U-shaped cartilage that connects them. Complete synostosis of the bones in the acetabulum occurs by the age of 14-17.
To determine the ratio of the elements of T. with. various landmarks are used ( rice. 3, 4, 5 ). So, the inner wall (bottom) of the acetabulum and the wall that bounds the pelvic cavity in this area, form a "teardrop". The femoral heads are normally located at the same distance from the "tear figure". Also symmetrically projected onto the lower-inner quadrant of the femoral head is the "crescent shape" formed by the groove between the posterior part of the lunate surface and the body of the ilium. A vertical line (Ombredann's line), lowered from the outer point of the upper edge of the acetabulum, runs outside of the femoral head or through its outer segment. The arcuate line (Shenton's line) smoothly passes from the lower contour of the femoral neck to the upper edge of the obturator opening. The angle formed by the horizontal line (Hilgenreiner's line), drawn through the symmetrical sections of the Y-shaped cartilage on both sides, and by the line passing through the outer and inner points of the acetabular vault, does not exceed 22-26 ° (Fig. 5). An increase in the angle indicates a slope (underdevelopment) of the roof of the acetabulum. The displacement of the femoral head in relation to the listed landmarks indicates the presence of its subluxation or dislocation. Adults can normally have additional bone formations of T. page. (fig. 6).
Pathology
Developmental defects include T.'s dysplasia by page, congenital varus and hallux valgus deformities of the femoral neck.
Dysplasia of the hip joint is manifested by the underdevelopment of the acetabulum and the proximal femur. Among other orthopedic diseases in newborns, it occupies one of the first places (from 5 to 16 per 1000 newborns). The incidence of the birth of children with dysplasia T. s. increases with unfavorable heredity, elderly parents, infectious diseases of the mother, endocrinopathy, toxicosis of pregnant women, breech presentation of the fetus. More and more attention is paid to the teratogenic effect of ionizing radiation. Dysplasia occurs in utero and is primary, and the displacement of the femoral head (subluxation or dislocation) occurs a second time, usually in the postnatal period. With age, the number of subluxations and dislocations increases.
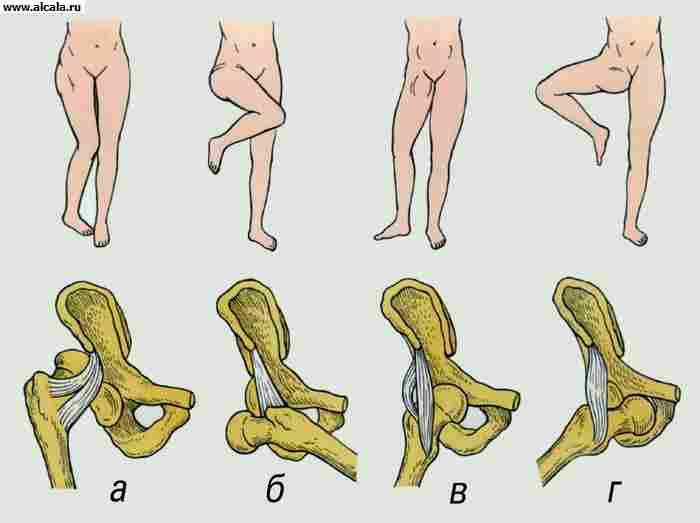
There are three degrees of dysplasia T. page: preluxation, subluxation and dislocation. The most common clinical signs of hip dysplasia, which can be detected in the first months of a child's life, are the symptom of slipping, or the symptom of "click", restriction of passive abduction of the hip on the affected side, asymmetry of skin folds on the child's thighs, shortening of the entire lower limb, installation of the lower limb to the external rotation position.
In children over 1 year old, with unilateral dislocation, instability or lameness is noted when walking, and with bilateral dislocation, a waddling, so-called duck, gait. The classic sign of a formed dislocation is a positive Trendelenburg symptom. In addition, with pressure on the calcaneus, an increase in the mobility of the greater trochanter in the longitudinal direction and its upward displacement is determined. Normally, the femoral head is palpated at the level of the femoral artery pulsation; in case of hip dislocation, the head is not palpable in this place.
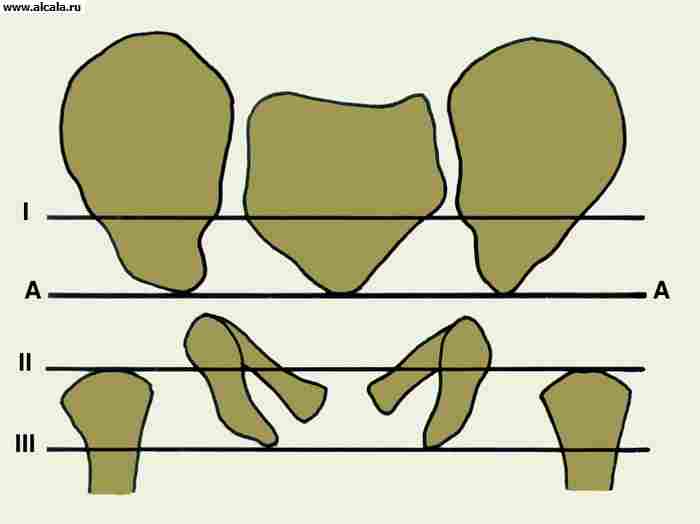
In the diagnosis of dysplasia T. p. X-ray examination plays a significant role. The early radiological signs of this pathology are considered to be an increase in the slope of the roof of the acetabulum, displacement of the proximal end of the femur outward and upward relative to the acetabulum, late appearance and hypoplasia of the ossification nucleus of the femoral head.
In children older than 1 year, 5 degrees of T.'s dysplasia are distinguished: the head of the femur is located laterally, but at the level of the cavity (I degree); the head is located above the horizontal line of the Y-shaped cartilage at the top of the acetabulum (grade II); the head is located above the visor of the acetabulum, the formation of a neo-cavity is possible (III degree); the entire head is covered with the shadow of the wing of the ilium (IV degree); extremely high position of the femoral head at the top of the iliac wing (grade V).
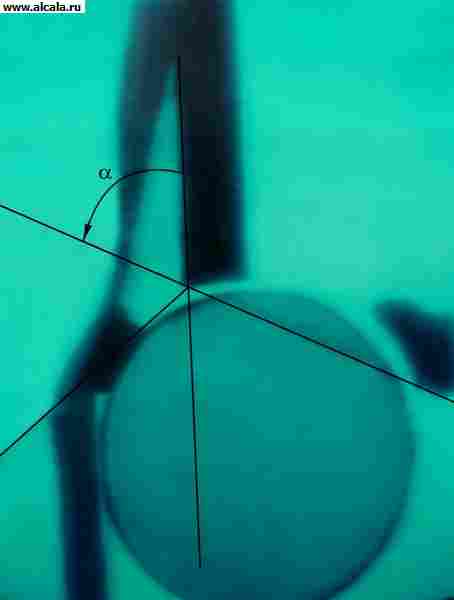
In newborns and children under 1 year of age, to determine developmental disorders of T. s. also use ultrasound (ultrasonography). The main advantages of this method are its harmlessness to the patient, visualization of the soft tissue structures that form the joint at this age. With the help of ultrasonography, the development of the joint is dynamically monitored during the child's growth and treatment. An ultrasonogram determines the degree of formation of the bone and cartilaginous parts of the roof of the acetabulum, the location of the limbus (the cartilaginous part of the acetabulum), as well as the appearance of ossification nuclei in the head of the femur. For a quantitative assessment of the data of ultrasonographic research, 3 auxiliary lines are drawn: the main line parallel to the wing of the ilium; line from the lower bone edge of the cavity to the upper; line from the upper bony edge of the roof of the acetabulum to the middle of the limbus. The angle formed by the main line and the bone roof line characterizes the degree of development of the bone roof. The angle formed by the main line and the line of the cartilaginous roof characterizes the degree of development of the cartilaginous part of the roof of the acetabulum. Depending on the ultrasonographic picture T. s. and the ratio of the values of these angles, all joints are divided into 4 types, in each of which subtypes are distinguished. A normally formed joint corresponds to type 1, subtypes A and B ( rice. 7, 8 ). Type 2 A (Fig. 9) is detected in children under 3 months of age with a physiological delay in ossification of the acetabular roof. Type 2 B ( rice. 9, g ) is determined in children after the age of 3 months, the development of the joint in these children requires the supervision of an orthopedist. Type 2 C corresponds to hip pre-dislocation, these children need treatment to ensure proper development of the joint. Type 3 A (Fig. 10) corresponds to a subluxation of the hip, in which case the normal structure of the cartilaginous part of the acetabular roof is determined ultrasonographically. In type 3 B (Fig. 11), there are signs of changes in this structure, which is a poor prognostic sign. Type 4 - dislocation, the head of the femur is outside the acetabulum (Fig. 12).
Treatment of dysplasia T. page. start from the moment pathological changes are detected. Newborns from the very first days to eliminate the contracture of the adductor muscles undergo therapeutic exercises, which consists in abducting the legs bent at the knee and hip joints. Swaddling legs should be loose. To keep them in a divorced position, various pads, a pillow and a Freyki envelope are used. For the same purpose, abduction (abduction) sliding functional tires CITO and others are used, which retain the possibility of movement in the joints of the lower extremities (except for adduction of the hips), which contributes to the formation of the roof of the acetabulum. The most favorable age for starting functional treatment of children is from 2-3 weeks to 5-6 months. The abduction splint is removed on average after 4-7 months. The duration of treatment is determined by the timing of the formation of the roof of the acetabulum. With an early start of treatment, patients with dysplasia or subluxation get on their feet and begin to walk at the same time as healthy children. Satisfactory results can be achieved with the use of an abduction splint in the second year of a child's life.
In case of hip dislocation with a high head position and a sharp contracture of the adductor muscles (i.e., most often with late diagnosis), treatment should be started immediately with vertical traction using an abduction splint. Gradually build up the load and increase the degree of limb dilution. Stretching should start with a small weight (300-500 g) for each leg, increasing it daily by 100-200 g. The maximum weight is determined by the position of the buttocks (when lifting them above the bed). The period of application of traction is from 3 to 12 weeks. With the early treatment of congenital hip dislocation, patients stand on their feet while still wearing an abduction splint at the age of 8-11 months. They begin to walk either with the splint or after removing it, usually at the age of 12-15 months. However, conservative methods of treatment of T.'s dysplasia with. not always effective, for example in the case of interposition of the joint capsule. Surgical interventions for most dislocations are performed in children over 2 years of age. Surgical treatment is also indicated for irreducible dislocations already at the age of 1-2 years, as well as for complications that are noted after dislocations previously reduced using conservative methods.
All surgical interventions for congenital hip dislocation are divided into intra-articular and extra-articular. Intra-articular operations include anterior capsulotomy according to Ludloff, open reduction without deepening of the cavity, open reduction with depressions of the cavity, open reduction with corrective osteotomy of the hip, Scagletti operation, etc. Extra-articular operations are reconstructive operations on the basis of the ilium, reconstructive operations at the upper end (varizing and detorsion-varising osteotomies), palliative operations.
With a well-formed acetabulum and a developed femoral head, simple open reduction is possible. The operation is effective at the age of 2-4 years with mild antetorsion of the femoral neck. In case of underdevelopment of T. s. open reduction of dislocation is combined with deepening of the depression or the formation of its upper edge.
With residual hip subluxation, T.'s instability. in children aged 3 to 5 years, in 2/3 of cases it is caused by a violation of the development of the proximal femur and only in 1/3 - by the underdevelopment of the anterior superior edge of the acetabulum. By the age of 7-8, already in 50% of cases, and by the age of 10-12, in almost 100% of cases, surgical intervention is indicated not only on the femoral, but also on the pelvic component of the joint.
With moderate underdevelopment of the acetabulum in children under 7-8 years of age, complete osteotomies in the area of the base of the ilium are effective. The Chiari operation provides after osteotomy to displace the femoral head together with the acetabulum inwards, Salter's operation - to turn the cavity outwards (in recent years it has been preferred). With a shallow depression, a double osteotomy of the pelvis according to Pozdnikin (also at the age of up to 7 years) and pericapsular acetabuloplasty according to Pemberton, Korzh and others (up to 8-12 years) are used. In adolescents and adults with subluxation of the femoral head, satisfactory results were observed with corrective osteotomy of the femur for centering the head and osteotomy of the pelvis according to Andrianov (plastic of the roof of the cavity).
With a high head position, formed neoarthrosis, its operative reduction from the age of 8-10 is not very promising.It is more expedient to carry out a corrective subtrochanteric double osteotomy with lengthening according to Shants - Ilizarov - Kaplunov, which allows creating an additional point of support, maintaining mobility in neoarthrosis and eliminating functional shortening of the limb.
Physiotherapy exercises are used at all stages of both conservative and surgical treatment of congenital hip dislocation. The general tasks of using remedies for exercise therapy are the activation of the activity of the main systems of the body and the prevention of complications associated with hypokinesia; improvement of circulatory conditions in the joint and lower extremities: restoration of static-dynamic disorders of the musculoskeletal system (restoration of mobility in the hip joint and strengthening of periarticular muscle groups). The child's parents should be informed about the need to perform special exercises repeatedly throughout the day throughout the course of treatment.
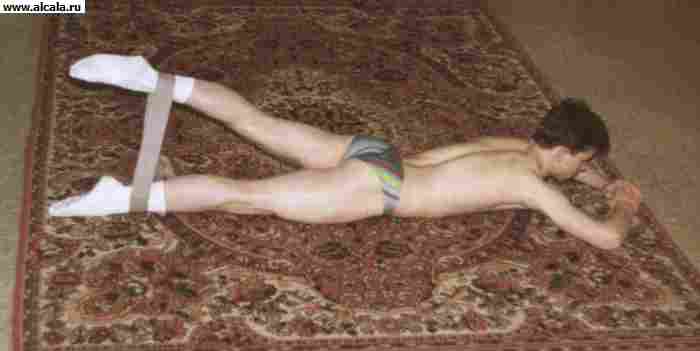
During the period of fixing the child's limbs with various orthoses or splints, special physical exercises are aimed at strengthening the abductor muscles of the thigh. Children under 3 years of age are recommended to use passive and active-passive movements in T. with. for abduction. In the first months of life, reflex exercises are used. At an older age, the exercises are performed independently with a gradually increasing load, for example, the free dilution of the legs bent at the knee joints is carried out with additional external resistance to movement at the expense of the hands of the methodologist or the mother, stretching the rubber bandage with which the hips are tied at the level of the knee joints. Special exercises are done several times a day in combination with light relaxing massage (superficial stroking, shaking) of the adductor muscles of the thigh. In addition to the special exercises described above, breathing and general developmental exercises for the belt of the upper extremities are performed.
After completing the treatment with orthoses or abduction splints, it is necessary to carry out a course of manual massage (12-15 procedures) of the gluteal muscles and legs. Cycling with widely spaced pedals, exercise in warm water, swimming, and regular exercise are recommended. Therapeutic gymnastics is aimed at restoring the function of the joint and increasing its stability. Free exercises are used for flexion, extension, abduction, and internal rotation in T. with. in the prone position: At the same time, exercises are prescribed to strengthen the abductor muscles of the thigh. You should not force your child to walk. He will get up and walk on his own when his neuromuscular apparatus is ready for vertical loading.
The main purpose of rehabilitation treatment after intra-articular operations on T. page. is to create conditions for the restructuring of the structural elements of the joint and its functions. The special tasks of the remedies used for exercise therapy are the restoration of joint mobility, training of the periarticular muscles, gradual preparation for the performance of the supporting and locomotor functions.
In surgical methods of treating congenital hip dislocation in the postoperative period (immobilization), general developmental breathing exercises, isometric muscle tension under a plaster cast, free and free movement in non-immobilized joints are used.
After the termination of immobilization or the use of stable osteosynthesis for osteotomy of the hip or pelvis, physical exercises are aimed at the fastest restoration of joint function. For this, facilitated (active with self-help) movements in the hip joint, physical exercises in a hydrokinesisotherapy bath in combination with manual and underwater massage are performed. As mobility in the joint is restored, exercises aimed at strengthening the periarticular muscle groups and electrical stimulation of the gluteal muscles are added. It must be remembered that as a result of a femoral osteotomy, the attachment points of the abductor muscles of the thigh and external rotators may move, which leads to their functional failure. Therefore, much attention is paid to special physical exercises aimed at training the hip abductors with gradually increasing resistance. Therapeutic exercises are carried out in the supine position, on the side, on the stomach, as well as in the knee-wrist position (on all fours). The axial load on the leg is gradually increased with good mobility, gluteal muscle function, and restoration of the bone structure of the femoral head.
Varus deformity of the femoral neck(sokha vara) is manifested by a functional decrease in the cervico-shaft angle. It is based on pathological restructuring along the neck of the femur or directly in the area of the growth zone. Lameness, relative shortening of the lower limb, its external rotation and adduction are clinically noted. Trendelenburg's symptom is positive. The greater trochanter is displaced above the Roser - Nelatin line, the symmetry of the Shemaker line and the isosceles of the Bryant triangle are broken. Movements in T. s. limited, especially internal rotation and abduction.
In early childhood, attempts are made to stop the progression of pathological restructuring in the femoral neck region by prolonged unloading of the joint in combination with therapeutic exercises, physiotherapy and spa treatment. Conservative treatment is effective only with early diagnosis. In older children and adults, corrective osteotomies of the proximal femur or operations aimed at restoring its support are performed.
Congenital hallux valgus(plow valga) is characterized by an increase in the cervico-diaphyseal angle, is much less common. Clinically, there is a lower location of the greater trochanter, some lengthening of the limb. In case of dysfunction, an intertrochanteric varizing osteotomy is indicated.
Damage hip joint - bruises, traumatic dislocations of the hip, fractures of the head and neck of the femur, acetabulum. Contusions are manifested by local soreness, limited mobility in the joint. Bleeding into soft tissues, intermuscular hematomas are possible. Treatment is conservative.
Traumatic dislocation of the hip is usually the result of an indirect injury. Depending on the position of the femoral head in relation to the acetabulum, posterior, anterior and central dislocations are distinguished (Fig. 13). In addition to pain and limitation of the function of the joint, the forced position of the limb is noteworthy (see Dislocations). In posterior dislocations, the limb is in the position of flexion, adduction and internal rotation; in the front, it is straightened (or slightly bent), abducted and rotated outward. Often it is possible to palpate the head of the femur. With a central dislocation with protrusion of the head, the retraction of the greater trochanter is noted.
On radiographs, the femoral head is found outside the acetabulum. Posterior dislocations are characterized by an increase in the length of the x-ray image of the femoral neck (as a result of its internal rotation), for anterior dislocations, an increase in the size of the lesser trochanter, a projection decrease in the neck length, and an increase in the cervico-diaphyseal angle (signs of external rotation of the femur). With central dislocations, cracks in the bottom of the cavity and comminuted fractures with protrusion of the head are distinguished.
The victims are treated in a hospital. Before transportation, immobilization is carried out without changing the fixed position of the limb. With fresh hip dislocations, reduction is more often performed using the Kocher method. Subsequent unloading of the joint is carried out using skeletal traction with a load of 3-4 kg. Walking with crutches is allowed after 5-6 weeks, loading the limb - no earlier than 3-4 months. With cracks in the bottom of the acetabulum, unloading skeletal traction is used along the axis of the thigh. In case of fractures with protrusion of the head, to extract it, they resort to traction along the axis of the femoral neck.
During the period of the patient's stay on skeletal traction after traumatic dislocation of the hip, physical exercises are aimed at preventing hypostatic complications, improving blood circulation in the limb. Against the background of general developmental exercises, free movements are used in all joints of the intact limbs and the ankle joint of the injured leg, short-term isometric tension of the thigh muscles, gluteal muscles on the affected side.
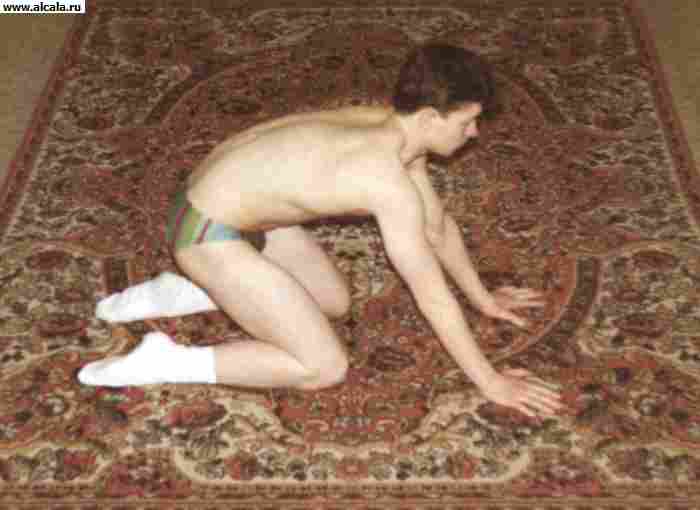
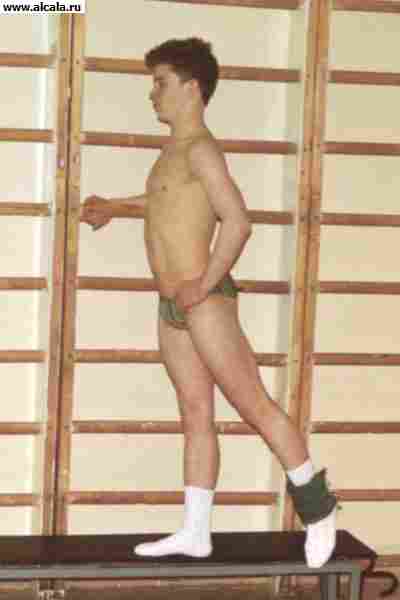
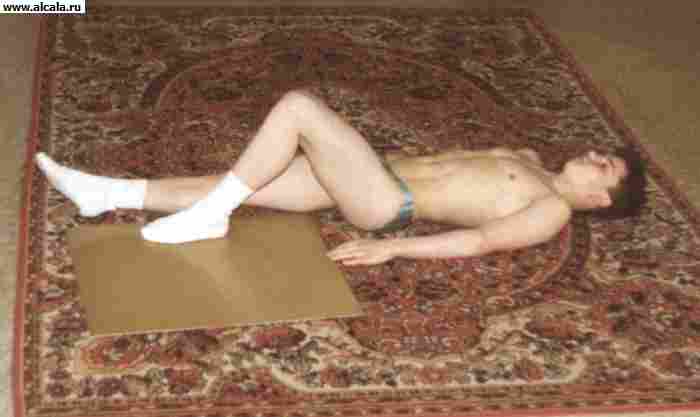
After removing the traction, walking with crutches with a partial load on the leg is allowed. The restoration of joint mobility is carried out in parallel with an increase in its stability by strengthening the ligamentous-muscular apparatus. To increase the mobility in the joint in the initial lying position, free movements (flexion, extension, abduction, rotation) are performed in the hip joint without lifting the foot from the bed or couch (Fig. 14). To strengthen the muscles, prolonged isometric tension of the gluteal muscles and muscles of the thigh, static holding of the raised, abducted, unbent legs, etc. are used (Fig. 15). It is not allowed to perform swinging movements and to stretch the ligamentous apparatus of the joint, as well as muscle training with an axial load on the leg.
With fracture dislocations T. s. therapeutic gymnastics is aimed at preventing the development of post-traumatic coxarthrosis. Longer unloading of the joint with crutches is recommended (up to 6 months after injury). In the future, with prolonged walking and the presence of pain syndrome, it is recommended to walk with additional support on the cane.
After the termination of immobilization, physical exercises in water are shown using exercises at the side of the pool and swimming elements, underwater and manual massage of the gluteal muscles and thigh muscles, heat therapy, ultrasound. Therapeutic gymnastics is carried out in the supine position, on the side, abdomen with the use of free movements in the hip joint. To strengthen the muscles of the thigh, an initial position of standing on a healthy leg on a dais is applied. The raised leg is held forward (to the side, back) for 3-5 s, alternating with free swinging movements of the relaxed leg. In the future, when carrying out these exercises on the ankle joint, the cuff is strengthened with a load of 250-500 g. In outpatient settings, it is necessary to repeat the courses of treatment 1-2 times a year.
Diseases. Inflammatory changes in T. with. predominantly of infectious origin (see. Coxitis), can proceed with a predominance of exudative or proliferative processes. Possible primary lesion of the synovium with subsequent involvement of the femoral head and acetabulum in the process, or secondary (primary bone forms of coxitis).
The earliest clinical manifestations are pain in the joint area, limitation of mobility with the formation of myogenic contracture, and an increase in local temperature. With purulent and tuberculous coxitis, further destruction of bone structures occurs, often with dislocation of the hip, shortening of the limb and strengthening of its vicious position. The consequence of purulent coxitis is often bone ankylosis in the vicious position of the limb. For tuberculous coxitis, fibrous ankylosis is more characteristic. With the destruction of the articular capsule, an abscess or phlegmon of paraarticular tissues is formed. A transition to a chronic form with the formation of fistulas is possible.
One of the first radiological signs is osteoporosis. The presence of foci of destruction in the bone elements of the joint indicates an active inflammatory process. Subsequently, the destruction of the articular surfaces is observed. Bacteriological examination of exudate is of great importance. The joint is punctured from the front in the projection of the femoral head or outside above the greater trochanter.
In the acute period, antibiotic therapy is indicated in combination with joint immobilization. Surgical intervention is often used for acute and purulent coxitis (arthrotomy with joint drainage). With extensive destruction, the affected sections are resected, usually the head and neck of the femur (i.e., draining resection). in the vicious position of the limb, extra-articular interventions are used (corrective osteotomies (osteotomy)).
Dystrophic processes in the joint develop more often against the background of dysplasia, the consequences of trauma, inflammatory processes and metabolic disorders (see Coxarthrosis).
Chondromatosis T. s. rare; manifests itself as intermittent blockage and severe pain. Surgical treatment - removal of intra-articular bodies (see Chondromatosis (Chondromatosis of bones and joints)).
The causes of aseptic necrosis (see. Aseptic bone necrosis) of the femoral head are different. It manifests itself in pain, lameness, limited movement (see Perthes disease). In case of ineffectiveness of conservative treatment (unloading of the joint, physiotherapeutic procedures), they resort to surgical intervention (corrective osteotomies, endoprosthetics, arthrodesis).
Tumors can come from the capsule of the joint (see Synovioma), cartilage and bone tissue. In the proximal femur, osteoblastoclastoma, osteoma, chondroblastoma, chondroma, chondrosarcoma, osteosarcoma are observed (see. Joints, tumors). Surgical treatment: resection with osteoplastic replacement of the defect or endoprosthetics of the proximal femur, disarticulation of the femur.
Operations
For drainage and revision, arthrotomy is used. Osteosynthesis or Endoprosthetics are performed for medial fractures of the femoral neck. In order to improve statics, corrective osteotomies of the proximal femur are performed. Arthroplasty is used to restore joint mobility. For this purpose, various options for endoprosthetics are being carried out. To restore the support of the thigh, arthrodesis is performed (see. Joints). With dysplasia T. page. in addition to corrective osteotomies of the proximal femur, reconstructive operations on the pelvic component are shown in order to increase the coverage of the femoral head.
See also Thigh.
Bibliography: Human Anatomy, ed. M.R. Sapina, vol. 1, p. 144, M., 1986; Vilensky V.Ya. Diagnostics and functional treatment of congenital hip dislocation, M., 1971, bibliogr .; Volkov M.V., Ter-Egiazarov G.M. and Yukina G.P. Congenital dislocation of the hip, M., 1972; Kaplan A.V. Damage to bones and joints, p. 355, 359, M., 1979; Conservative treatment of children with diseases of the musculoskeletal system., Ed. E.S. Tikhonenkova, s. 73, L., 1977; A.A. Korzh and other Dysplastic coxarthrosis, M., 1986; Marx V.O. Orthopedic diagnostics, p. 355, Minsk, 1978; Mirzoeva I.I., Goncharova M.N. and Tikhonenkov E.S. Surgical treatment of congenital dislocation of the hip in children, L., 1976; Orthopedic and traumatological care for children, ed. V.L. Andrianova, p. 39, 44, L., 1982; Pathology of the hip joint, ed. V.L. Andrianova, p. 4, L., 1983; Shkolnikov L.G., Selivanov V.P. and Tsodyks V.M. Injury to the pelvis and pelvic organs, M., 1966.













![]()









formed by the acetabulum and the head of the femur. Both articular surfaces are covered with cartilage. The acetabulum is part of the pelvis, located at the confluence of the ilium, ischium and pubic bones. The bursa runs along the edge of the glenoid cavity, passes to the femur and is attached over its trochanters, therefore, most of the femoral neck is located in the cavity of the hip joint. The articular bag is very strong, reinforcing ligaments are woven into it. T. p. refers to polyaxial joints - flexion and extension, adduction and abduction, rotation of the hip outward and inward are possible. It is supplied with blood from regional vessels.
First aid is provided for injuries of the hip joint of various severity. So, with Bruises in the area of T. s. pain is noted, swelling and hemorrhage are usually mild, movements in the joint are not limited. In this case, it is enough to apply cold and relieve the joint until the pain subsides. For small superficial wounds in the joint area, a sterile pressure bandage is applied. Intra-articular fractures and dislocations of the hip joint are severe injuries. Unlike a bruise with fractures of the bones that form the T. page, the leg is in a forced position, for example, turned outward, the victim cannot lift the injured leg, when trying to move, the pain intensifies. With some fractures of the femoral neck (for example, hammered in), swelling in the T. with. expressed slightly, sometimes the victims can even move independently. In trochanteric fractures, the swelling and hemorrhage is more extensive and extends to the upper third of the thigh. Due to the fact that it is possible to finally establish the diagnosis only after a special examination, and the external manifestations of an extensive contusion of the T.'s area of page. and fractures are very similar, the volume of first aid should be the same as in a fracture. It is very important to immobilize the hip joint well before transporting the victim to the hospital. It is better to use the Dieterichs bus for this (see. rice. 4 to the article Thigh), and in its absence - improvised tires of a sufficiently long length.
Dislocations in the hip joint are relatively rare. As a rule, they occur in case of severe mechanical injury, for example. as a result of a road accident or a fall from a height. The head of the femur, displacing, tears the articular capsule with the ligaments that strengthen it and is located in the periarticular tissues. The leg is in a forced position ( rice. ), movement in T. s. are impossible, severe pain appears immediately after the injury. When providing first aid, you should not try to "correct" the position of the leg. The victim urgently needs to be taken to the hospital for examination and reduction of the dislocation. Immobilization of the damaged joint is carried out in the position in which it is located after dislocation. At the same time, unnecessary movements should be avoided, because they increase pain and can cause additional trauma, eg. sciatic nerve damage.
With open damage to the area T. s. a sterile bandage is applied to the wound. A pressure bandage is applied to small wounds; in case of more extensive damage to soft tissues, the joint is immobilized as in a fracture.
Splinting- see Thigh.
Bandages, used in the provision of first aid in connection with injuries of the T.'s area of page, more often bandages, less often use a mesh bandage. For small wounds, you can apply an adhesive bandage. Depending on which area is covered, a unilateral (right, left) or bilateral spike-shaped pelvic bandage can be applied, as well as an anterior one that closes the groin area, an external (lateral) one that closes the greater trochanter area, and a posterior one that closes the buttock area. When applying the right-sided anterior (inguinal) spike-shaped dressing of the pelvis, the first round of the bandage is made around the body at the level of the navel, leading the bandage from left to right, the next round is performed obliquely from behind to front along the lateral, and then along the front surface of the right thigh to its posterior semicircle and turn obliquely upwards and medially, crossing the previous round of bandage in the groin area. Further, the bandage is carried over the pelvic bones on the left side, and from there it is directed to the posterior semicircle of the body and again to the groin area, repeating the previous rounds of the bandage and overlapping them by 2/3 of the diameter. Finish the bandage with circular rounds of the bandage around the body. Subsequent rounds of bandage can be ascending (each next round is higher than the previous one) or descending. When a similar bandage is applied to the left groin area, the bandage also goes from left to right, but after the first fixing rounds around the body, it goes obliquely from behind to the front surface of not the right, but the left thigh, bypasses its back surface and then goes obliquely up the thigh, crossing with by the previous round, it goes around the back of the body and again goes to the front surface of the left thigh, repeating the previous rounds and covering each of them by 2/3 of its width. Finish applying the bandage also with circular rounds of the bandage around the body. For greater strength, each eight-shaped bandage (ear) can be fixed with one circular round.
If necessary, cover with a bandage T. c. a slightly different version of the spike-shaped bandage is used on all sides - the spike-shaped bandage of the thigh, which begins in a circular motion not on the body, but on about the middle third of the thigh. By the method of application, it is similar to a spike-shaped bandage of the shoulder, that is, having fastened the bandage on the thigh, the bandage is carried along the outer surface of the T. page. to the lower back, make a fixing circular round around the body and continue bandaging in the same way as when applying a pelvic spike bandage, gradually overlapping the previous rounds.
In emergency cases or in the absence of other dressing material, you can use kerchiefs on the T. with. To do this, use two kerchiefs. One middle is placed over the damaged area of tissue, the ends are wrapped around the thigh and tied, and the third end (top) is brought under the belt formed from the other scarf, folded back and fastened with a pin. If a second gusset is not available, a belt can be used.
INJURIES AND DISEASES OF THE HIP JOINT
R.M. Tikhilov, V.M. Mashkov, G.G. EpsteinAnatomical and functional features
Biomechanics of the hip joint
Methodology for assessing the level of compensation for violations of static-dynamic function
Gradation of indicators of compensation for violations of the static-dynamic function
Comprehensive assessment of the violation of static-dynamic function
Hip bruises (E.G. Gryaznukhin)
Hip dislocations (E.G. Gryaznukhin)
Fractures of the head and neck of the femur
Deforming arthrosis
Aseptic necrosis of the femoral head of the joint
Examination of patients with diseases of the hip joint ,
Non-operative treatment
General principles of surgical treatment of coxarthrosis
Principles of Conservation Hip Surgery
General provisions for planning surgery
Surgical treatment of patients with dysplastic coxarthrosis
The proximal part of the femur consists of the head, neck, and greater and lesser trochanters (Fig. 1). SDU is on average 126-127 ° (115-135 °). A decrease in the SAD (from 126 ° to 90 °) weakens the resistance of the neck to mechanical stress, which contributes to fractures, especially in the elderly (Fig. 2). The femoral head is approximately 2/3 of a ball, with an average radius of 20 to 22 mm. The acetabulum is half a ball. It deepens due to the cartilaginous ring covering the entire edge of the cavity. Thus, the head deeply enters the glenoid cavity, which is a good, strong and reliable support for the lower limb. The cavity itself is located at the junction of the three pelvic bones, which, in fact, form it. This is an important detail to consider when classifying hip dislocations based on the location of the dislocated head.

The acetabulum is supplemented with a fibrous-cartilaginous rim (labrum glenoidale) 5-6 mm high, which increases the depth of the cavity. The cartilaginous lip in the area of incisurae acetabuli grows together with the transverse ligament of the acetabuli stretched between its edges (ligamentum transversum acetabuli). In the glenoid cavity, its marginal part (facies lunata) is covered with cartilage, and its central part (fossa acelabuli) is made of fatty tissue and the base of the round ligament, covered with synovial membrane. The articular cavity almost completely corresponds to the head of the femur, which is covered with hyaline cartilage, with the exception of the fovea capitis femoris, where the ligament of the head is attached.
From the point of view of the surgical anatomy of the acetabulum, there are functional columns that provide support for the femoral head (Fig. 3). Most often, the anterior column (pubic) and the posterior (ilio-ischial) are differentiated. The anterior column goes from the anterior superior iliac spine obliquely downward, inward and anteriorly towards the pubic symphysis, the posterior (more powerful and massive) descends from the greater ischial notch to the tuberosity of the ischium. The apex of the convergence angle is represented by a compact bone, which forms the roof of the acetabulum.
However, four columns are often distinguished:
- external, which corresponds to the roof of the acetabulum;
- anterior and posterior, which are formed by the pubic and ischial bones, respectively;
- the inner, least durable, which is the bottom of the acetabulum.

The acetabulum has a certain spatial orientation, it is inclined outward and downward by 45 ° and rotated anteriorly by 15 °.
The femur is curved in three mutually perpendicular planes:
- sagittal (bending of the diaphysis anteriorly),
- frontal (tilt of the femoral neck in the medial direction),
- horizontal (rotation of the femoral neck around the longitudinal axis). The inclination of the femoral neck in the medial direction forms an angle with the longitudinal axis of the femur - SHDU (in adults it is 127-130 °).
The deviation of the femoral neck in the horizontal plane is measured by the angle formed by the intersection of the central axis of the neck and head with the transcondylar axis of the femur. If the neck with the head of the femur is turned anteriorly, then they speak of anteversion, if posteriorly, of retroversion. In adults, the angle of anteversion is usually 10-15 °.
On the border of the neck and body of the femur there are two powerful bony tubercles, called trochanters. The greater trochanter is damp above and outside, on its inner surface facing the neck is the trochanteric fossa. The lesser trochanter lies at the lower edge of the neck, medially and posteriorly. An intertrochanteric line connects both trochanters in front, and an intertrochanteric crest in the back.
The fibrous bag of the joint consists of connective tissue fibers running in longitudinal and transverse directions. The interlacing of the fibers gives the bag its durability. The bag is attached to the pelvic bones around the acetabulum with a wide rim from 10 to 28 mm in front and from 10 to 33 mm in the back.
On the anterior surface of the femoral neck, the fibrous bursa extends 10-20 mm below the transitional fold of the synovium and is attached near the intertrochanteric line.

Behind, the capsule covers almost 2/3 of the femoral neck, attaching itself to the greater trochanter at the top, and to the small one at the bottom. The density and strength of the capsule in different parts of it are not the same. It depends on the intimate connection of the capsule with the auxiliary, reinforcing ligaments passing through it, the fibers of which are woven into the capsule and are practically inseparable from it. These ligaments approach the capsule from three sides and are named according to the gas bones (Fig. 4).
The most durable of them - the ilio-femoral - begins below the anterior lower iliac spine with a wide base, descends outward and downward in a fan-like manner and is attached along the entire intertrochanteric line. This ligament surrounds the upper-antero-inferior part of the joint in a semi-helical manner.
The screw arrangement of the ligamentous apparatus of the hip joint is also expressed in the direction of the fibers of the second ligament - the sciatic-femoral ligament. This ligament, starting at the back of the acetabulum on the body of the ischium, twists, passes to the upper surface and attaches to the bottom of the trochanteric fossa.
The third ligament - pubic-femoral - begins on the pubic bone and is woven from the bottom medially behind into the joint capsule, reaching the lesser trochanter.
The ilio-femoral ligament inhibits flexion, adduction, and external rotation;
ischio-femoral limits adduction and extension;
The pubo-femoral one inhibits extension, abduction, and internal rotation.
In the "middle position", the capsule with all the ligaments relaxes. With full extension of the hip, the capsule tenses, and the ligaments, twisting around the joint in a screw-like manner, screw the head into the glenoid cavity. This position is so strong that further extension of the hip is possible only with the pelvis.
The helical direction of the fibers of the ligaments of the hip joint significantly strengthens the already strong capsule, which, therefore, seems to be an important factor protecting the joint from traumatic effects on it. However, in the capsule of the hip joint there is a less protected place: this is the lower posterior and lower anterior parts of it. The first is located outward from the edge of the ischio-femoral ligament, the second is located between the horizontal and vertical parts of the ilio-femoral ligament. In these places, with traumatic dislocations, the capsule ruptures, passing the shifting head of the femur.
The hip joint is surrounded by powerful muscles that also protect the joint from violence. The main role in this respect belongs to the following of them.
The iliopsoas muscle covers the entire front of the joint; when the hip is extended, it is passively tense and tightly attached to the joint.
The large middle and small gluteus muscles, as well as the piriformis, twin and obturator muscles, press the femur against the glenoid cavity and cover (except for the gluteal muscles) the back and lower part of the joint. Due to the muscles, movement is carried out around three main axes: flexion-extension, adduction-abduction, rotation, as well as complex combinations obtained by adding these movements.
From the muscles that originate in the spine and pelvis,
large lumbar,
pear-shaped and
the gluteus maximus attaches to the femur and provides movement in the hip joint. The psoas major muscle, connecting with the iliac muscle, attaches to the lesser trochanter and flexes the thigh, and with a fixed leg, it flexes the lumbar spine and tilts the pelvis along with the torso forward.
An internal obturator muscle is attached to the inner surface of the greater trochanter, originating from the edges of the obturator foramen, to which, when leaving the lesser sciatic foramen, the superior and inferior twin muscles are attached, which also attach to the greater trochanter and, together with the piriformis muscle, rotate the thigh outward.
The external muscles of the pelvis are located in the gluteal region and on its lateral surface and follow from the bones of the pelvic girdle to the femur. They form three layers
- superficial (gluteus maximus and tendon fascia tensor),
- middle (gluteus medius, square thigh muscle; this also includes the extra-pelvic parts of the piriformis, internal obturator muscle and both twin muscles) and
- deep (gluteus maximus and external obturator muscles).
A very powerful gluteus maximus muscle has a wide origin from the iliac crest, the posterior surface of the sacrum and coccyx, the sacro-tuberous ligament, runs obliquely downward and outward and attaches to the gluteal tuberosity of the femur. Part of its bundles goes over the greater trochanter and passes into the iliotibial tract of the fascia lata. The main function of the muscle is to extend the thigh and rotate it outward, in addition, individual bundles take part in the abduction of the thigh (anterior-superior bundle) and hold the knee joint in an extended position due to the tension of the broad fascia of the thigh. The postero-inferior bundles bring the thigh and simultaneously rotate it outward.
The gluteus medius extends from the ilium and fascia lata downwards, passes into the tendon, which attaches to the apex and outer surface of the greater trochanter. The gluteus maximus muscle is located under the middle, it begins on the outer surface of the ilium and attaches to the antero-outer surface of the greater trochanter. These muscles abduct the thigh, their anterior bundles provide internal rotation, the posterior ones - external.
The fascia lata tensioner starts from the anterior superior iliac spine and the adjacent part of the ridge, passes at the border of the upper and middle third of the thigh into the iliotibial tract, which attaches with its distal part to the lateral condyle of the tibia. This muscle flexes the hip, stabilizes the knee joint in an extended position. In addition, it is a feeding stem when using the iliac wing section for plastic replacement in the hip joint area (with aseptic necrosis of the femoral head, dysplasia, etc.).
The quadratus thigh muscle and the external obturator muscle provide external rotation of the thigh.
The thigh muscles are classified into three groups:
- anterior (flexors),
- back (extensors) and
- medial (adductors).
The anterior group is represented by the sartorius and quadriceps muscles. The muscles of the posterior group include
- two-headed,
- semitendinosus and
- semi-membranous. 
The medial muscle group is
- thin,
- comb and
- leading (long, short and large).
Movement in the hip joint is possible in all directions and in a very significant amount. An extremely favorable circumstance, from the point of view of preventing traumatic dislocations, is that a person uses this large range of movements very rarely (except for persons whose professions are associated with the need to produce a significant range of movements - ballerinas, gymnasts, etc.)
Thus, the anatomical and physiological features of the hip joint protect the joint from traumatic dislocations:
1) there is a complete correspondence of the articular surfaces;
2) a bag with its reinforcing ligaments is a very strong formation;
3) powerful muscles protect the joint from violence;
4) a large range of motion in the joint with significantly lower functional requirements limits the possibility of the formation of unusual extreme positions in the joint, which can lead to dislocations. 
The neck and head of the femur consist of spongy tissue, covered at the periphery with a thin plate of compact bone substance (Fig. 5). On the lower-inner surface of the neck, this layer is much thicker and is called the Adams arch, which can be used as a support for the fixator when fastening the neck and head of the femur in case of fracture, it is very strong and prevents the fixator from moving downward under the influence of "shear force".
Inside the femoral neck (Fig. 6) there is another solid piece of bone tissue called the Merkel spur. The bony beams of the femoral neck have the form of a vault. The spongy tissue consists of a system of thin beams arranged in the form of arches, through which body weight is transferred to the walls of the bone tube. These crossbeams are located according to the lines of compression and tension trajectories, like a bracket, and are directed arcuately towards the middle of the bone, intersect with its axis at an angle of 45 °, and between themselves at an angle of 90 ° (Fig. 7). This structure gives the neck significant strength and allows it to withstand heavy loads.

The blood supply to the neck and head of the femur is carried out through numerous terminal small vessels extending from the medial and lateral arteries that surround the femur (Fig. 8). The femoral head is supplied with blood through the artery of the ligament of the femoral head, which is unstable and its role decreases significantly with age. The branches of this artery end at the beginning of the head in the form of a loop or penetrate into the peripheral layer of the head and in the form of weak processes.

The sources of blood supply to the neck and head of the femur are (according to A.N.Shabanov, I.Yu. Kai, 1966, Fig. 9.1):
- A - from the artery of the ligament of the femoral head, it is limited and sometimes absent;
- B - numerous large vessels penetrate into the neck from the places of attachment of the capsule;
- B - short small vessels pass from the synovial membrane to the head;
- D - numerous and well-developed vessels come from the intraosseous arteries;
- D - from the places of muscle attachment in the intertrochanteric region.
In the intact thigh, these vessels anastomose freely. Violation of the blood supply to the proximal femur fragment depends on the location of the fracture (Fig.9.2):
- fracture along line 1 - blood supply due to group A.
- fracture along line 2 - blood supply due to groups A + B.
- fracture along line 3 - blood supply due to groups A + B + B + D.
- fracture along line 4 - blood supply is practically not disturbed. 
One of the main reasons for delayed consolidation, the formation of a pseudarthrosis and necrosis of the femoral head is a violation of the blood supply to the proximal fragment due to rupture of the vessels feeding it. With high fractures of the neck, the head of the femur sharply decreases or completely loses its blood supply. Poor immobilization or insufficient adaptation of the fragments leads to head necrosis and cervical resorption (Fig. 10).
The hip joint has a rich innervation, which is carried out by the nerves of the periosteum, periarticular neurovascular formations, as well as branches of large nerve trunks: the femoral, sciatic, obturator, superior gluteal, lower gluteal and genital nerves. The posterior-lower part of the articular capsule is innervated by branches of the sciatic nerve, as well as the superior gluteal and genital, the anterior part is innervated by the articular branch of the obturator nerve.
The round ligament and the fat pad are innervated by the posterior branch of the obturator nerve; in addition, the branches of the femoral and superior gluteal nerves may participate in the innervation of these structures.

Kinematics of the hip joint. In accordance with the shape of the hip joint and the state of the surrounding tissues, the maximum total amplitude
- flexion-extension movements is 140 °,
- adduction-abduction - 75 ° and
- rotation - 90 °.
When walking, the used range of motion in the hip joint is significantly less than the potential one: flexion and extension movements do not exceed 50-60 ° with a minimum of adduction-abduction and rotation. In everyday life, maximum joint movement is associated with the wearing of shoes or socks and generally implies approximately 160-170 ° total total mobility, which includes flexion, abduction, and external rotation.
Distribution of pressure in the hip joint. The biomechanics of the hip joint is complex and changes depending on the position of the person while standing and walking.
Distinguish two-bearing phase stride when the load is evenly distributed between the two joints, and single support phase when the body weight rests on one leg.
In this phase, the steps, in turn, emit
- support on the heel,
- support on the whole foot and
- push with the front of the foot (toes).
In the standing position, the entire articular surface of the acetabulum is loaded and approximately 70-80% of the femoral head is in contact with the articular cavity. Only the lower surface of the femoral head and the area around foveae capituli femoris remain unloaded, which corresponds to the location of the round ligament of the thigh and the fat pad in the area fossae acetabuli. When walking, while moving in the joint, the roof of the acetabulum (roof) does not experience prolonged stress, and only the front and rear parts of the head maintain contact with it. Using the hip joint endoprosthesis for measurement, it was determined that the contact pressure in the postero-superior part of the acetabulum when the patient got up from the chair was more than 18 MPa. This transition from partial contact during movement of the joint to full contact with support on the leg is responsible for the change in the load zone on the femoral head during walking. In the presence of discongruence during walking, a contact area with high pressure can be created: however, this does not happen due to the fact that as a result of deformation of two layers of articular cartilage and the underlying subchoidal bone tissue, both the contact area and the congruence of the articular surfaces increase, thus ensuring the transition from discongruence in the phase of movement in the joint to congruence with support on the leg. This transition allows the joint to distribute greater load forces more efficiently.
However, this transition from discongruence to congruence creates high joint pressure when walking, more than 21 MPa. This high pressure is well tolerated by a healthy hip joint, however, in the presence of joint dysplasia, regular overloads of the same area of bone tissue lead to the development of degenerative-dystrophic changes. In addition, a practically significant question arises whether this pressure is not a factor that ensures the transfer of the products of abrasion of polyethylene (debris) into the tissues surrounding the pedicle and acetabulum after arthroplasty.
Distribution of forces acting on the hip joint. A general idea of the distribution of forces acting in the hip joint can be obtained by statistical analysis of the vectors of forces acting on the joint in one plane during support on the leg. Two other methods for calculating the forces acting on the hip joint involve direct measurement by implanted devices or mathematical modeling of the load on the joint by one of the known methods. Studies on the distribution of loads in the hip joint are important for a better understanding of the function of the normal and affected joint, the development of the optimal treatment method, in terms of determining the best implant, performing a corrective osteotomy and drawing up a rehabilitation program, as well as for understanding the pathogenesis of the pathological process in the hip joint.

Using plane static analysis, the load distribution in the hip joint can be represented by considering a simple leverage system. In a standing position with support on both legs, the center of gravity of the body passes through the discs Th10 and Th11. The perpendicular, lowered from this point to the horizontal line connecting the centers of rotation of the femoral heads, divides it into two equal arms (Fig. 11). If the body weight (60 kg) is reduced by subtracting the weight of the legs to 40 kg, then a mass equal to 20 kg acts on each head of the femur.

In the single-support position, the center of gravity is shifted down to the level L3-L4 and, when walking, changes its position in accordance with the phase of the step. In this case, two main forces act on the femoral head (Fig. 12):
- force TO- body weight minus the weight of the supporting leg, acts vertically through the lever b and
- force M, which is determined by the efforts of the muscles that support the pelvis and the whole body in balance and acts on the center of rotation of the head through the lever a, lowers the pelvis down and laterally.
Leverage ratio a and b is 1: 3. Knowing the size of the levers a and b, you can calculate the magnitude of the resulting force R, which acts on the head of the femur and is the sum of the body weight and the muscle strength balancing it. With a single-bearing step phase, the sum of the acting forces relative to the center of rotation of the head is equal to zero, i.e. M x a = K x b.
Muscle strength M consists of the action of the pelviotrochanteric muscle group and the dorsal crural. Pelviotrohunter group includes mm. gluteus médius et minimus, m. piriformis, m. iliopsoas, their resulting force is in the region of the greater trochanter and is directed at an angle of 29.3 ° downward and outward.
The dorsal crural group consists of m. tensor fasciae latae, m. rectus femoris, m. sartorius, its resultant force is located in the region of the lesser trochanter at an angle of 5.5 °, directed posteriorly and medially. The total resultant force M runs from top to bottom, from the inside to the outside and forms an angle of 21 ° with the vertical line.
In turn, the strength M can be imagined as consisting of two components: strength Pm is directed vertically downward, and the force Qm- horizontally in the lateral direction. Thus, the following forces act on the center of rotation of the femoral head: Pm and TO in the vertical and caudal direction and Qm and horizontal and lateral direction (Fig. 13).

Parallel forces K and Pm add up, resulting in the resulting force R, which is directed at an angle of 15.4 ° to the vertical line (Who is it directed at this angle, the average person? - H.B.)
... This force is opposed by an equal and opposite force R1, which presses the head into the acetabulum. In turn, the obliquely directed force R1 can be represented by two forces: the force of retraction of the head into the acetabulum ( Qm) and the force of compression of the head ( R). Each of these forces is opposed by equivalent, but oppositely directed forces that make up the resulting force R... It is important to see the differences between the resulting forces R and R1.
Force R is directed to the center of the head and does not depend on the position and inclination of the acetabulum. The opposing force R1 Is the counterpressure force of the femoral head and acetabulum, and it acts directly through the acetabular vault: compressive force Q directed parallel to the surface of the cartilage, and the force R- perpendicular to this surface. Their size and direction depend on the inclination of the acetabulum. It is only when the vault of the acetabulum is horizontal that all four forces are balanced. If the vault of the acetabulum has a craniolateral inclination (with dysplasia of the acetabulum), then the force Q strength decreases and prevails Qm directed to the displacement of the femoral head from the acetabulum.
With decreasing strength Q there is a compensatory increase in the force of compression of the head R... It is this imbalance of forces that leads to a gradual subluxation of the femoral head with the formation of an osteophyte along the lower inner surface of the head. Strength increases with craniomedial acetabular inclination (consequences of acetabular floor fracture or rheumatoid arthritis) Q directed to displacement of the head inward, and the force R decreases (Fig. 14, 15).
An important point in assessing the biomechanical prerequisites for the development of many pathological processes is the analysis of the formula for the equality of the moment of forces. With a decrease in the distance between the greater trochanter and the center of rotation of the femoral head (this is observed when plow valga, shortening of the femoral neck due to injury or previous Legg-Calne-Perthes disease, etc.) shoulder a decreases, which leads to a proportional increase in muscle strength M and total strength R and R1 affecting the hip joint (according to the formula R = K x b / a).
With an increase in the distance between the greater trochanter and the center of rotation of the femoral head ( plow valga) the lever arm of the resultant muscle force increases and, accordingly, the value of the resultant muscle force decreases M.
The presence of flexion-adduction contracture of the joint with external installation of the leg, which is most common in coxarthrosis, causes a significant increase in the load on the hip joint. In this case, there is a skew of the pelvis, which leads to a more significant shift of the center of gravity towards the unsupported lower limb when leaning on the sore leg. As a result, the shoulders of the patient's gravity lever increase, and hence the moment of force K x b... Accordingly, great muscle strength is needed to balance the joint. M which ultimately increases the overall stress on the joint.
The above principles and calculations of the load on the hip joint apply to cases of implantation of an artificial joint (endoprosthesis). Interesting data were obtained with triaxial telemetry after total hip arthroplasty. In the position of support on two legs, the intended load on the joint was equal to the body weight. Single-support leg load corresponded to 2.1 body weight, load peaks were observed during walking and were measured from 2.6 to 2.8 body weight. Telemetric measurements revealed the emergence of large forces aimed at twisting during rotational movements in the region of the head and neck of the endoprosthesis during rotational movements.
We are glad to present you the first social network of supporters of a healthy lifestyle in the Russian-language Internet and a full-fledged platform for the exchange of experience and knowledge in everything related to the words "health" and "medicine".
Our task is to create an atmosphere of positive, kindness and health on the site, which will cheer you up, heal and prevent, because information and thoughts are transformed into material events! ;-)
We strive to create a highly moral portal in which a variety of people will be pleasant to be. This is facilitated by the fact that we control the actions of all users. At the same time, we want the site to be fairly objective, open and democratic. Here everyone has the right to express their personal opinion, to their own assessment and comment on any information. In addition, anyone can have an article, news or any other material in most sections of the site.
The project "To health!" positioned as a portal about health, not medicine. In our opinion, medicine is the science of how to recover from a particular disease, and health is the result of a lifestyle in which you will not get sick. The more health you have, the less likely you are to get sick. Our body is conceived in such a way that with the right lifestyle we should not get sick at all. Therefore, let's improve our health instead of studying diseases. There are many sites about medicine, but in our opinion, they are intended more for medical professionals than for ordinary people. We strive to talk with you about health. We do not want to write a lot about diseases and methods of their treatment - enough has already been written about this. Instead, we'll focus your attention on how to avoid getting sick.
We are interested in a healthy lifestyle and want to live happily ever after. We believe you, too, are not indifferent to the topic of healthy longevity. Therefore, if you want to have an environment of healthy people and those who strive for this, this site will help you solve this problem. Our plans include the creation of an active community of people leading a healthy lifestyle, and in this regard, we are pleased to offer you the following opportunities:
- create your page with personal photos, blog, forum, calendar and other sections
Do what you like, and we will try to provide you with everything you need for this. We strive to make this site the most comfortable for you. There is still a lot of new and interesting ahead.
Register yourself and invite your colleagues, friends and close people to the site for constant contact with them and exchange of experience. Be always in touch, discussing all the news and interesting in the field of health.
Stay with us!
