Equipment standards for the blood collection room. Treatment room equipment standard
Introduction
Functions nurse treatment room
Treatment room documentation
General documentation for the treatment room
Conclusion
Literature
Introduction
To provide effective and qualified assistance to a sick person, a nurse must perfectly master the necessary volume of deep knowledge, skills, practical skills, that is, be a professional in her field.
For this, nursing documentation is being developed and implemented, standards that contribute to a complete analysis of the patient's problems, ways of solving them, allowing to assess the quality of nursing care. Along with this, programs for assessing the quality of nursing care have been developed, as well as a model of the final result with the possibility of economic incentives for the work of a nurse. The functional responsibilities of the nurse in the treatment room are: Correct organization of the work of the room for the implementation of diagnostic and treatment measures, according to the profile of the department. Immediately inform the doctor about complications associated with the procedure. Provision of first aid medical care. Strict adherence to asepsis, antiseptics, infectious safety standards, OST 42-21-2-85 "Sterilization and disinfection of medical devices." Strict implementation of measures for the prevention of serum hepatitis and HIV infection. Compliance with the sanitary and epidemiological regime of the office in accordance with the current orders.
Timely replenishment of the office with medicines, instruments. Security correct storage medicines, serums, monitoring of expiration dates. Clear documentation. Compliance with safety regulations. Improve qualifications and professional skills.
1. Functions of a nurse in a treatment room
I. Implementation of diagnostic and treatment measures:
The introduction of drugs and the conduct of medical manipulations in accordance with the regulation of the types of activities of a nurse;
Blood sampling from a vein for diagnostic studies;
Assisting a doctor with:
a) carrying out manipulations with grave condition sick;
b) determining the blood group and Rh factor;
c) approbation of a new drug.
II. Office work. Logging:
Appointments;
Accounting for the work of the treatment room;
Accounting for intravenous fluids and droppers;
Accounting for intramuscular, subcutaneous injections and antibiotics;
Delivery of bixes to the central sterilization room;
Registration of general cleaning;
Accounting for patients who have had hepatitis;
Complications associated with medical procedures.
III. Relief of complications associated with medical procedures with a doctor's notice.
IV. Organization of work of junior medical personnel.
V. Participation in the preparation of a reserve of nurses in the treatment room.
2. Documentation of the treatment room
In order to comply with the sanitary and epidemiological regime, an order was put into effect, which is used in health care institutions, the order contains the following provisions:
Order of the Ministry of Health of the USSR No. 770 of 06/10/1985 on the introduction of the industry standard ost 42-21-2-85 sterilization and disinfection of medical devices. Methods, means and modes (together with the industry standard approved by the USSR Ministry of Health on 06/07/1985)
GOST 42-21-2-85 “Sterilization and disinfection of medical devices. Methods, means, modes ".
Guideline R.3.1.683-98 “Use of ultraviolet bactericidal radiation for disinfection of air and surfaces in rooms);
Order of the Ministry of Health of the USSR No. 408 of 12.06.89. "On measures to reduce the incidence of viral hepatitis in the country"
Order of the Ministry of Health and the Ministry of Health of the Russian Federation No. 170 of 08.16.94 "On measures to improve the prevention and treatment of HIV infection in Russia."
SanPiN 2.1.3.1375-03 of 06.06.2003 “Hygienic requirements for the placement of the device, equipment and operation of hospitals, genus. houses and other medical hospitals ".
Order of the FGU TsGSEN RME No. 130/84 SE of 1.06.2001 "On improving measures for the prevention of nosocomial infections in health care facilities of the republic."
SanPin 2.1.5.980-99 "Rules for the collection, storage and disposal of waste from health care facilities."
SP 3.1.958-00. "Prevention of viral hepatitis. General requirements to epidemiological surveillance of viral hepatitis ".
Order of the Ministry of Health and the Ministry of Health of the Russian Federation No. 170 of August 16, 1994 "On the introduction of
preventive vaccinations against hepatitis B ".
Order of the Ministry of Health of the Russian Federation No. 25 of January 1998 "On strengthening measures to prevent influenza and other acute respiratory infections."
Regulatory documents governing the accounting, storage and dispensing of medicines of various groups:
Order of the Ministry of Health of the USSR dated 08/30/91. № 245 "On consumption standards ethyl alcohol for healthcare, education and social welfare institutions ”.
Order of the Ministry of Health of the USSR dated 2.06.87 No. 747 “Instructions for the registration of medicines, dressings. medical instruments "
Order of the Ministry of Health of the USSR No. 720 dated July 31, 1978 “On improving medical care patients with purulent - surgical diseases and strengthening measures to combat nosocomial infections "
Order of the USSR Ministry of Health of 30.0891 No. 245 "On standards for the consumption of ethyl alcohol for health care, education and social security institutions"
Order of the Ministry of Health of the USSR dated 2.06 198. No. 747 "Instruction for the registration of medicines, dressings, medical instruments"
Appendix No. 2 № Approximate consumption rates of ethyl alcohol in the departments of health care facilities "
All medicines are divided into three groups: "A", "B" and "General list". According to the method of application, medicines are divided into: parenteral, internal and external.
Group "A" includes narcotic and poisonous drugs that are kept by the head nurse in a metal safe under lock and key and shot to the floor. On the back of the safe is a white letter "A" on a black background and the word "VENENA" in black letters on a white background. On the left side wall there is an inscription "narcotic drugs", on the right wall of the safe - "poisonous". On the inner wall of the safe door is a list of narcotic and poisonous agents, their highest daily and single doses.
All potent drugs belong to group "B" and are stored in lockers with markings: on the back wall there is a red letter "B" on a white background and the word "HEROICA" in black on a white background. List "B" includes 14 groups of medicines, determined by the mechanism of action:
1. Antibiotics
2. Sulfonamides
3. Some digitalis drugs
4. Analgesics
5. Antispasmodics
6. Hypotensive
7. Sedatives
8. Sleeping pills
9. Hormonal
10. Diuretics
11. Anticonvulsants
12. Antiarrhythmic
13. Stimulating CNS
14. Excitatory respiratory center.
In the cabinets they are arranged according to the mechanism of action, according to the application. Internal drugs are separate from parenteral drugs.
On the objectively quantitative couple, there are psychotropic drugs from list No. 3 - 16 items.
Medicines of the "general list" are stored in cabinets with the inscription inside: on a white background in black letters "general list". Parenteral drugs are stored separately from internal and external drugs are located according to the mechanism of action.
3. General documentation for the treatment room
The treatment room should contain:
1. Professional job description.
2. Orders, instruction letters of the Ministry of Health of the Russian Federation, institutions of the State Sanitary and Epidemiological Supervision, local administration, regulating the activities of the nurse in the treatment room.
3. List of documentation for the treatment room:
Quartz cabinet notebook.
General cleaning notebook
Notebook for accounting for azopyram and phenolphthalein samples.
Sterilization control log for instruments and soft inventory.
Treatment room appointment log.
Intravenous blood sampling notebook for biochemical analysis, HbSAg, blood group Rh factor.
Intravenous blood sampling record book on RW.
Notebook for recording intravenous blood sampling for HIV infection.
Fridge temperature control notebook.
Register of prof. Vaccinations.
Hepatitis vaccination register.
4. List of equipment, equipment for the treatment room.
5. List of the sequence of the workflow.
6. List of medicines required for emergency assistance.
7. List of medicines, a list of measures to be taken in case of anaphylactic shock.
8. List of medicines, expiration dates.
9. Instructions for the storage of drugs.
10. Higher single doses of narcotic drugs.
11. Table of antidotes for drug poisoning.
12. Higher single and daily doses of potent and poisonous medicines.
13. Incompatibility of medicines.
14. List of medicines stored in the refrigerator, the sequence of their placement.
15. A complex of anti-epidemic measures for the prevention of HIV / AIDS, hepatitis in the treatment room.
16. Precautions when working with disinfectants and detergents.
17. First aid for poisoning with disinfectants.
18. Methods of sterilization.
Standards:
Treatment room equipment standard;
Standard for equipping a treatment room with solid inventory
Antibiotic dilution standard;
Intramuscular injection standard;
Subcutaneous injection standard;
Intravenous injection standard;
Blood sampling standard for biochemical research;
General cleaning standard;
Current cleaning standard;
Sterile table cover standard;
Bix stacking standard;
The standard for the preparation of 10% of the original clarified solution of bleach.
treatment room nurse document
Conclusion
The quality of medical care is determined, first of all, by the health care organization system as a whole and by each of its branches separately. The functioning of the health care system is determined by laws and regulations.
In the treatment room of the healthcare facility, all the appointments of the attending physicians are carried out. In the office, everything should be provided for carrying out various medical procedures: performing injections - subcutaneous, intramuscular, intravenous; taking blood from a vein for laboratory research; providing emergency assistance in emergency situations.
The procedural nurse is responsible for: the correct organization of the work of the procedural room around the clock; For the timely fulfillment of the doctor's prescriptions for the procedures; For the implementation of the sanitary and epidemiological regime at their workplace, the rules of asepsis and antiseptics; For providing the office during the day with the required number of instruments, drugs, solutions, sterile material for performing procedures; For compliance with the conditions and rules for storing medicines, inventory, tools, cabinet equipment; For the high-quality documentation of the office and making notes on the procedures performed. For the correct organization of the work of the nurse's office.
Literature
Agkatseva S.A. Practical skills training in the system of secondary medical education. Algorithms of manipulations in the activities of a nurse. Phoenix, 2006 - 168s.
Fundamentals of nursing: Textbook Weber V.R., Chuvakov G.I., Lapotnikov V.A., et al. - M .: Medicine, 2001- 496s.
A Nurse's Guide to a Treatment Room. Chernova O.V. - Rostov n / a: Phoenix, 2006 - 15p.
Handbook for nurses treatment room Grinenko A.Ya. WORD ,. 2005 - 20s.
Similar works:
- Abstract >>
Applicable legislation. Documentation procedural and vaccination cabinet 1. Quartzing notebook cabinet... 2. Notebook of general ... syndrome. Scope of work performed in procedural cabinet... V procedural cabinet I do subcutaneous, intramuscular and ...
- Abstract >>
When carrying out manipulations in this cabinet... High quality lead documentation procedural cabinet... Make marks daily in the completed ...
Filling the drip system
I. Preparation for the procedure
1. Wash the hands.
2. Check the tightness of the packing bag and the expiration date of the system.
3. Use non-sterile tweezers to open the central part of the metal cap of the vial with drug and treat the rubber stopper of the bottle with a cotton swab (napkin) dipped in alcohol.
4. Open the packaging bag and remove the system (all actions are performed on the desktop).
II. Procedure execution
5. Remove the cap from the airway needle (short needle with a short tube, closed with a filter) and insert the needle against the stop into the bottle cap; fix the free end of the air duct on the bottle (you can do this with a pharmacy rubber band). Note. In some systems, the airway opening is located directly above the drip chamber. In this case, you only need to open the plug that covers this hole.
6. Close the screw clamp, remove the cap from the needle at the short end of the system, and insert this needle all the way into the vial stopper.
7. Turn the bottle over and fix it on a tripod.
8. Turn the dropper in horizontal position(if it is not rigidly connected to the vial needle), open the clamp; slowly fill the dropper to half the volume.
9. Close the clamp and return the dropper to its original position: the filter must be completely submerged in the infusion liquid.
10. Open the clamp and slowly fill the long tube of the system until the air is completely expelled and drops appear from the injection needle; it is possible to fill the system without putting on the injection needle, in which case drops should appear from the connecting cannula.
11. Check for air bubbles in the long system tube (system full). III. End of procedure
12. Place the injection needle, closed with a cap, in a sterile tray or in a packaging bag, cotton balls(napkins) with a skin antiseptic, sterile napkin.
13. Prepare two strips of narrow (1 cm) adhesive plaster, 4-5 cm long.
Intravenous drip
I. Preparation for the procedure
1. Ask the patient about the drug's awareness and consent to the injection.
2. Help the patient get into a comfortable position.
3. Apply a tourniquet to the middle third of the patient's shoulder.
4. Wear gloves.
II. Procedure execution
5. Treat the elbow bend area in succession with two cotton balls (napkins) with a skin antiseptic; the patient squeezes and unclenches the hand at the same time.
6. Fix the vein by pulling the skin of the elbow.
7. Remove the cap from the needle and puncture the vein, as usual (the patient's hand is clenched into a fist), covering the needle cannula with a sterile ball.
8. When blood appears from the cannula of the needle, remove the tourniquet.
9. Open the clamp, attach the system to the cannula of the needle.
10. Adjust the drip rate with the screw clamp according to the doctor's prescription.
11. Secure the needle with adhesive tape and cover it with a sterile napkin.
12. Remove gloves, wash hands.
13. Monitor the patient's condition and well-being throughout the entire drip procedure.
III. End of procedure
14. Wear gloves.
15. Close the screw terminal.
16. Remove the needle from the vein, pressing the injection site with a ball (napkin) with alcohol for 5-7 minutes (do not leave cotton wool on the patient!); you can fix the ball with a bandage.
17. Make sure the bleeding has stopped.
18. Remove gloves, wash hands.
If it is necessary to sequentially enter medicinal solutions from several vials, proceed as follows: when the first vial remains a small amount of solution, quickly remove the air duct from it and insert it into the stopper of the second bottle, previously fixed on a tripod. The needle for the bottle is also quickly rearranged on the short part of the system. If it is necessary to carry out frequent and prolonged intravenous drip infusions, the vein catheterization method is used. Catheterization of the subclavian vein is performed by a physician, while catheterization of peripheral veins (elbow, hand) is performed by a specialized nurse.

Treatment room documentation.
1.PROCEDURAL NURSE INSTRUCTIONS
2. HOURLY SCHEDULE
3.GENERAL CLEANING LOG
4. MEDICAL APPOINTMENT LOG
5. BLOOD COLLECTION LOG FOR BIOCHEMICAL RESEARCH
6 RW BLOOD COLLECTION LOG
7.LOG FOR TAKING BLOOD FOR HIV
8.LOG OF BLOOD AND BLOOD SUBSTITUTES
9.LOG OF ACCOUNTING OF MEDICINAL PREPARATIONS SUBJECT TO SUBJECT - QUANTITATIVE ACCOUNTING
10.LOG OF ACCOUNTING POISONOUS MEDICINES
11.LOG OF ACCOUNTING OF ALCOHOL
12.LOG OF ACCOUNTING NARCOTIC DRUGS
Introduction ……………………………………………………………………… ..3
Functions of a nurse in a treatment room ………………… 4
Procedure room documentation ………………………………… ..5
General documentation for the treatment room ……………………… 8
Conclusion ………………………………………………………………… 10
Literature …………………………………………………………………… .11
Introduction
To provide effective and qualified assistance to a sick person, a nurse must perfectly master the necessary volume of deep knowledge, skills, practical skills, that is, be a professional in her field.
For this, nursing documentation is developed and implemented, standards that promote full analysis problems of the patient, ways to solve them, allowing to assess the quality of nursing care. Along with this, programs for assessing the quality of nursing care have been developed, as well as a model of the final result with the possibility of economic incentives for the work of a nurse. The functional responsibilities of a nurse in a treatment room are: Correct organization the work of the office for the implementation of medical and diagnostic measures, according to the profile of the department. Immediately inform the doctor about complications associated with the procedure. Provision of first aid medical care. Strict adherence to asepsis, antiseptics, standards of infectious safety, OST 42-21-2-85 "Sterilization and disinfection of products medical purpose". Strict implementation of measures for the prevention of serum hepatitis and HIV infection. Compliance with the sanitary and epidemiological regime of the office in accordance with the current orders.
Timely replenishment of the office with medicines, instruments. Ensuring the correct storage of medicines, serums, monitoring the expiration dates. Clear documentation. Compliance with safety regulations. Improve qualifications and professional skills.
1. Functions of a nurse in a treatment room
I. Implementation of diagnostic and treatment measures:
The introduction of drugs and the conduct of medical manipulations in accordance with the regulation of the types of activities of a nurse;
Blood sampling from a vein for diagnostic studies;
Assisting a doctor with:
A) carrying out manipulations in a serious condition of the patient;
B) determining the blood group and Rh factor;
C) approbation of a new medicinal product.
II. Office work. Logging:
Appointments;
Accounting for the work of the treatment room;
Accounting for intravenous fluids and droppers;
Accounting for intramuscular, subcutaneous injections and antibiotics;
Delivery of bixes to the central sterilization room;
Registration of general cleaning;
Accounting for patients who have had hepatitis;
Complications associated with medical procedures.
1. Journal of registration of transactions related to turnover drugs and psychotropic substances.
2. Journal of appointments in / m and n / c.
3. Journal of appointments in / in and in / in drip infusions.
4. Register of blood sampling for biochemical research.
5. Register of blood sampling for HIV and VH, RV.
6. Register of the introduction of antibiotics.
7. Register of blood transfusions and blood substitutes.
8. Journal of registration of general cleaning.
9. Log book of the operation of the bactericidal lamp hours.
10. Journal of registration of disinfectants.
11. The logbook of the temperature in the refrigerator.
12. Journal of registration of work dry heat.
13. Register of control of samples after disinfection and pre-sterilization cleaning.
14. Journal of accounting of alcohol.
15. Register of disposable syringes, systems
16. Register of medicines taken from patients.
17. Shift change log.
BOOK OF ACCOUNTING THE TURNOVER OF NARCOTIC DRUGS IN DEPARTMENTS AND OFFICES (Order No. 330-97, No. 205-03)
Name, unit of measure ______________________________________
___________________________________________________________________________
ANALYSIS SHEET№ 3-52
Department: surgery number 176
Name of the medicinal product: Promedol solution 1% - 1.0
Semenov A. V. Case history No. 1500
Pharmacy requirement
ANTIBIOTIC JOURNAL
BLOOD COUNTING LOG FOR HIV
LOG OF ACCOUNTING MEDICINES TAKEN FROM PATIENTS
REFRIGERATOR TEMPERATURE LOG
BLOOD TAKING LOG FOR BIOCHEMICAL RESEARCH
PROCEDURAL LOG (DIAGRAM) DESTINATION LOG
Section 10: Probe Manipulation.
TYPES OF GASTRIC AND DUODENAL PROBES
Types of gastric tubes.
1. Single and multiple use.
2. Rubber, elastic.
3. By appointment: for feeding through the mouth d 0.5-0.8 cm; intranasal d0.3-0.5 cm; for probing the stomach d 0.5 cm; for gastric lavage d0.8-1.0-1.5 cm.
4. Adults 1-1.5 m long, children (infant) for feeding newborns and infants(standard in sterile packaging).
Types of duodenal probes *
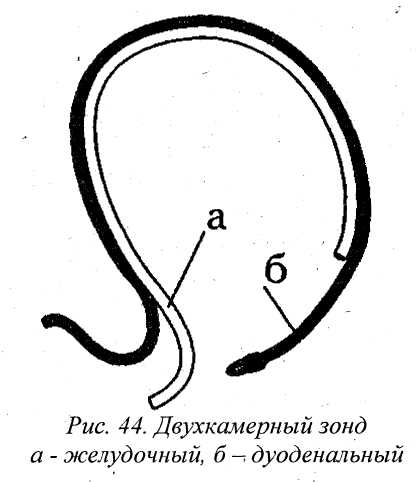
1. Rubber with a metal olive at the end d 0.5 cm, 1-1.5 m long.
2. Two-channel (for simultaneous gastric and duodenal intubation).
Target: therapeutic and diagnostic for the study of gastric secretion, to assess the secretory activity of the stomach.
Execution conditions: stationary, outpatient and polyclinic.
Contraindications:
1. Stomach and intestinal bleeding.
2. Peptic ulcer stomach, chronic cholecystitis and pancreatitis in the acute stage.
3. Diseases of the heart with severe circulatory failure (angina pectoris, myocardial infarction).
4. Hypertonic disease 3rd stage.
5. Damage to the esophagus.
6. 2nd half of pregnancy.
7. Diabetes mellitus.
Material resources:
Sterile gastric tube 1.5 m long 5 with a diameter of 3-5 mm, silk thread;
Syringe Janet;
Shipping container;
Container with disinfectant solution;
A napkin with a disinfectant solution;
Needle puller or needle disposer;
A rack with 9 test tubes, a towel;
A solution of histamine or pentagastrin for subcutaneous administration or an enteric irritant (30 g stale white bread, 300 ml warm boiled water);
Sterile syringe, cotton balls, alcohol 70 ° (for the introduction of histamine).
Personnel safety: Washing hands before and after manipulation. Use of masks and gloves, face shield, apron.
Patient preparation.
one. . Say hello, introduce yourself, clarify the patient's full name.
2. Explain to the patient the meaning of the procedure and the rules of behavior, find out the allergic anamnesis.
3. Obtain oral consent from the patient.
4. The night before - light dinner no later than 19 00 (scrambled eggs, porridge, cottage cheese).
5. In the morning on an empty stomach (do not drink water), probing is performed. Weigh the patient.
6. Conduct psychoprophylactic training (the night before).
Contraindications for the administration of histamine *
1. Allergies.
2. Hypertension.
3. Gastrointestinal bleeding.
4. Severe atherosclerosis.
In such cases, use a "test breakfast" - enteral.
At the heart of the poor tolerance of probe procedures in. in most cases there is a negative psychological preparation the patient for the probing process:
Reducing negative attitudes;
Fear of exploration can supplant, a more powerful attitude - stimulus - the goal of the procedure.
Technics.
1. Sit the patient on a chair with a back (remove if there are removable dentures). Measure the distance from the incisors to the navel, plus the width of the patient's palm - mark the first mark "entrance to the stomach", the second mark through 7-10 cm "the bottom of the stomach" or the patient's height in centimeters minus 100.
2. Put on gloves, mask and apron
3. Ask the patient to tilt his head back slightly, open his mouth, put the end of the probe on the root of the patient's tongue and say "a", take a deep breath through the nose and slowly gnaw the probe.
4. Slightly advance the probe following the swallowing movements (control the patient's breathing). Tilt the patient's head with the chin to the sternum for several sips.
5. As soon as the probe reaches the mark number 1 "entrance to the stomach", check where the probe is located. To do this, draw a small amount of air into a syringe, enter through a tube into the stomach. If the probe is in the stomach, the patient feels an "air jolt" in the epigastrium.
6. Advance the probe another 7-10 cm into the stomach.
7. Pump out the entire contents of the stomach into a test tube "lean portion" (with Janet's syringe). Clamp the probe.
8. In 15 minutes after a fasting portion, take 4 portions within an hour (after 15 minutes), take with a syringe "basal secretion" - 50-100 ml (norm). After each extraction of gastric contents, close the tube with a clamp.
9. Introduce subcutaneous histamine to the patient at the rate of 0.1 g ha 10 kg of patient weight or subcutaneous pentagastrin according to the scheme.
10. 15 minutes after the administration of histamine, take 4 more portions within an hour (every 15 minutes) - "stimulated secretion" - 50-110 ml (normal). Close the probe in between.
11. Remove the probe through a napkin soaked in disinfectant solution (according to the mode of viral infections).
12.Put the probe into a container with disinfectant for treatment.
13.Take the patient to the ward, make sure that the patient feels comfortable.
14.Transport the tubes to the laboratory (tubes in a rack, closed with stoppers) with a direction, in a container.
15. Process the probe according to the instructions.
16. Remove gloves, mask, apron into a container for processing. Wash your hands.
17. Make a note on the assignment sheet about the study.
