Symptoms of people with VNS pathology. Full description of the disease. What is included in botox treatment
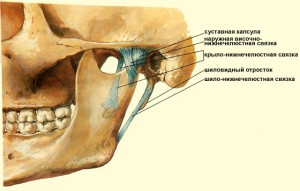
The temporomandibular joint allows a person to talk, chew food, and yawn. This joint in the skeleton is the busiest.
On average, according to a medical atlas, the TMJ is used 2 times per minute.
Temporomandibular dysfunction lower jaw joint was first discovered by B. Kosten, a famous otolaryngologist in the mid-30s of the last century. The specialist noted that this condition occurs due to high physical loads.
Kosten was able to prove that this syndrome provokes pain in patients in the area:
- heads;
- ears;
At the same time, he also proposed to eliminate the mentioned problem by correcting bite defects, as well as using an intraoral splint.
In turn, doctors point out that usually patients complain that they have a certain painful point in the area of the left or right joint. In this case, the movement of the jaw is often accompanied by a fairly clearly audible crunch or click. As a result, a person cannot eat and speak normally. In addition, sometimes patients indicate that their ears are blocked.
There are two considered joints on the human face. If they work symmetrically, then there are no problems or pains.
But if one of them is damaged at least a little, and very soon the second will start working incorrectly.
Dysfunction always develops in situations where displacement occurs lower jaw when you close or open your mouth. Therefore, they lead to it:
- change in bite;
- violation muscle tone or soft tissue injury;
- change in the position of individual components of the temporomandibular joint.
The vagueness of symptoms in most cases forces patients to visit doctors who are not involved in the treatment of this joint. Meanwhile, to determine the diagnosis, often the interaction of several specialists in related fields is required, which, according to objective reasons difficult.
Symptoms
 Most characteristic features TMJ dysfunction should be called pain. It occurs when a person eats, speaks or, for example, yawns, in the area:
Most characteristic features TMJ dysfunction should be called pain. It occurs when a person eats, speaks or, for example, yawns, in the area:
- faces;
- jaws;
- shoulders;
- in or near the ear.
She is usually blunt and quite strong.
At the same time, there is a limitation of the jaw's mobility, accompanied by its jamming.
Often, the work of the joint is accompanied by a crunch or crackle. When eating, the muscles of the face get tired very quickly. In addition, in some severe cases, one of the cheekbones noticeably swells.
Causes
Specialists now cannot bend to consensus, discussing the nature of the disease. Therefore, there are three leading theories of the appearance of TMJ dysfunction. This is about:
- myogenic;
- psychogenic;
- occlusal and articulatory.
In the latter case, the pathology develops due to:
- teeth defects;
- fast erasability of their surfaces;
- jaw injury;
- illiterately made prosthesis;
- wrong bite;
- other diseases, leading to the fact that the alveolar ridge becomes shorter.
In this situation pain syndrome usually appears about 10 or 12 days after the patient:
- pulled out one or more teeth;
- set too high a seal;
- incorrect prosthesis.
Moreover, in all cases, patients complain that the pain increases markedly with food and is accompanied by a decrease in the mobility of the jaw, which sometimes forces them to switch to soft food.
The myogenic hypothesis suggests that dysfunction is due to abnormalities in the muscles that move the jaw. This is due to both tonic spasm and mechanical overload of the muscles. Moreover, the habit of chewing on one side leads to the named problems. In addition, it develops due to:
- bruxism;
- professional factors.
As a result, there is a chronic injury to the TMJ.
The psychogenic version suggests that the disorder is provoked different kinds pathological changes in the structure of the central nervous system.
Diagnostics
 If you suspect TMJ dysfunction, you should promptly apply for medical help... Such problems are studied by such a medical discipline as neurology. However, in order to make the correct diagnosis, ideally, a consultation with a dentist is also required.
If you suspect TMJ dysfunction, you should promptly apply for medical help... Such problems are studied by such a medical discipline as neurology. However, in order to make the correct diagnosis, ideally, a consultation with a dentist is also required.
During the examination, the physician interviews the patient and examines him. It will be necessary to make impressions of the jaws in order to then make a diagnostic model.
In addition, sometimes it is required (in order to assess the condition of the joint) to undergo such examinations:
- orthopantomography;
- fluoroscopy;
MRI is needed in situations where there is suspicion of soft tissue damage. The quality of blood circulation is determined by Doppler sonography or rheoarthrography.
The main studies of the functional nature of doctors are called:
- gnathodynamometry;
- electromyography;
- phonoarthrography.
It is extremely important to exclude the following pathologies in the diagnosis:
- dislocation or subluxation of the jaw;
- arthritis;
- fracture of the articular process;
- synovitis;
- hemoarthrosis.
How to treat
First of all, it is necessary to reduce the stress on the joints. For this, the patient is transferred to soft food and it is recommended to talk less. For treatment, depending on what causes led to dysfunction, are attracted different specialists... It can be:
- orthodontist;
- terpaevt;
- dentist;
- vertebrologist;
- neurologist;
- psychologist;
- osteopath;
- chiropractor.
Pain is relieved with medication. In some cases, they are also prescribed:
- glucocorticosteroids (injections);
- antidepressants;
- various blockades;
- sedatives, etc.
Shown and myogymnastics. The main thing here is not to overload sore joints.
From physiotherapeutic agents, the following are suitable:
- laser treatment;
- electrophoresis;
- inductothermy;
- ultrasound.
The massage will help relax the chewing muscles. Psychotherapy also achieves a similar effect.
If the problem is due to dental factors, then the patient will need:
- restore the correct bite with braces;
- fix too protruding filling or prosthesis;
- polish teeth to restore their occlusion, etc.
If none of the above fixes the problem, then consider the possibility surgical intervention.
Treatment with folk remedies
It makes sense to use such options only in situations where the severity of dysfunction symptoms is not very pronounced. Ointments or compresses are most effective.
This composition is quite suitable for external use:
- 5 grams of turpentine and 10 vinegar are added to one yolk;
- everything is thoroughly mixed until smooth;
- cool slightly.
Ointment rubbed into sore spot until completely absorbed.
Here's another recipe:
- black radish is chopped on a frequent grater;
- juice is squeezed out;
- mixed with 150 milliliters of honey and a spoonful of table salt.
This drug is applied to the joint and wrapped in a scarf.
It should be noted that folk remedies full treatment cannot be replaced. Therefore, it is extremely important:
- follow all the doctor's orders;
- avoid eating solid foods;
- perform assigned exercises.
Unpleasant sensations in the temporomandibular joint most often occur with arthritis. It can span two sides or be one-sided. Arthritis is characterized by discomfort when chewing food and opening the mouth.
The chronic form can cause significant harm not only to the physical, but also to the emotional well-being of a person.
It is for this reason that treatment should be started immediately after the definition of the disease. This ailment can occur at any age, but older people are more likely to suffer. Also, quite often pain is observed in children. This is due to the constant growth in the growing body.
Causes
Pain and discomfort in the temporomandibular joint may appear on different reasons... It is extremely important to correctly determine the cause, because the effectiveness of future treatment will depend on this. Each of them has its own characteristics. The main reasons for the development of the disease:
- Infection and viruses;
- received injuries of a mechanical nature;
- all kinds of inflammatory ailments.
The infection can cause joint pain. The harmful microorganisms begin to form a positive environment for the formation of inflammation. It can enter the mouth by contact, direct contact, and blood. The most common is the straight path. So infection occurs when the joint capsule is injured and damaged. All kinds of microorganisms enter the oral cavity, which provoke the appearance of the disease.
The contact route is characterized by the multiplication and spread of bacteria from infected tissues. The main causes of contact infection: boil, purulent mumps, phlegmon, abscess, otitis media, osteomyelitis and all kinds of infectious diseases oral cavity... Measles, sepsis, diphtheria, tonsillitis, gonorrhea and syphilis can cause bloodborne infection.
Symptoms
To determine arthritis of the temporomandibular joint, you need to know the main symptoms, among which:
- Pain... With the formation of inflammatory processes, the pain is always very sharp, cutting or stabbing. It tends to intensify during movement. It is very difficult for a person to open his mouth even for a few minutes. It is worth noting that temporomandibular arthritis can have transient pain. This is because different parts of the face are connected by the trigeminal nerve.
- Fever. Heat the human body is observed when advanced stages diseases. Also, arthritis of the temporomandibular joint can be accompanied by muscle aches, increased fatigue, headaches and general weakness.
- Redness and inflammation... In the hearth accumulates large amount microbes, as a result, the joint may swell.
- Hearing impairment... When inflammation occurs, a decrease in the external auditory canal is observed. As a result, hearing can be impaired on the side of the joint injury.
Treatment

The first step is to note that the pain will not go away on its own, it is extremely important to provide the right treatment. In any form of this whitening, it is necessary to ensure the immobility of the jaw. For this, a special bandage is applied, which reliably fixes the jaw. If we are talking about an injury, then the bandage is worn for 7-9 days, but in the case of an infectious type, it is enough to fix the jaw for 1-3 days.
During treatment, it is better to refuse solid food, it is better to eat exclusively liquid food... If you are substitutes for at least some symptoms of arthritis of the temporomandibular joint and feel pain, then you should definitely consult a doctor for detailed advice. He will help to correctly determine the cause and prescribe treatment.
For any form of inflammation and deviation of the temporomandibular joint, anabolic drugs are prescribed. For traumatic types, medications are also prescribed that stimulate blood circulation in damaged tissues. If your ailment is of infectious origin, then you simply cannot do without strengthening the immune system. For this, doctors prescribe all kinds of vitamin complexes.
Each separate case has its own specifics, but in most cases after 3 days effective treatment positive changes are observed. After the relief of the main symptoms of the disease, they are prescribed additional procedures, these include: magnetotherapy, mud therapy, electrophoresis, hot paraffin applications, laser therapy, massage and all kinds of exercises that are necessary for muscle recovery.
If you have, then you can eliminate some of the symptoms at home. Bee venom ointments can be effective. But remember that it is forbidden to make them for people with allergic reactions... It is also recommended to make compresses from coltsfoot, chamomile, oak bark and thyme.
This procedure is best done at least 2 times a day. Before going to bed, it is recommended to apply iodine grid on the jaw. This product widely used in medicine. Its properties allow you to get rid of many negative factors... Will help relieve joint pain warm rinses from chamomile.
If the appearance of arthritis is associated with the presence of dental diseases, then after the elimination of the main symptoms, the oral cavity must be sanitized. This measure is mandatory. Otherwise, in just a couple of months, arthritis and joint pain will return again. With a rheumatoid variety, doctors prescribe a general strengthening course. These are all kinds of trace elements, dietary supplements and vitamins.
In practice, there are often cases of purulent and rather complex arthritis of the temporomandibular joint. In this case, you cannot do without a full-fledged surgical intervention. So the articular cavity is opened and a special drainage is installed. People suffering from purulent arthritis should undergo inpatient treatment, which can last from 2 to 4 weeks, it all depends on the complexity of the situation.
As mentioned earlier, only after determining the type and characteristics of the disease, treatment can be prescribed. Various methods are used to find out the cause. The most common are general analysis blood test and evaluation of clinical data.
In any case, every health problem leaves its mark on the body. Doctors advise you to improve your nutrition and put more emphasis on all kinds of fruits and vegetables. So the immune system will recover much faster and be less susceptible to disease.
DO YOU STILL SEE IT HARD TO GET RID OF JOINT PAIN?Judging by the fact that you are now reading these lines, victory in the fight against joint pain is not yet on your side ...
Constant or intermittent pain, crunching and palpable pain during movement, discomfort, irritability ... All these symptoms are familiar to you firsthand.
But perhaps it is more correct to treat not the effect, but the cause? Is it possible to get rid of joint pain without serious consequences for the body? We recommend reading the article by DOCTOR OF MEDICAL SCIENCES, PROFESSOR BUBNOVSKY SERGEY MIKHAILOVICH about modern methods getting rid of joint pain ...
The presence of spontaneous pain, fluid accumulation or effusion in the joint cavity. The difficulty in diagnosing diseases of the temporomandibular joint is associated with determining the source of pain - whether the pain in the joint area is caused by a disease of the muscles, joint or systemic disease... In most cases, arthralgic pain originating from the temporomandibular joint is referred to as pain located anterior to auricle... This pain sometimes radiates to adjacent (eg, temporal) areas. On palpation and movement, pain in the joint is noted.
Arthralgia can be caused by several joint diseases.
Displacement of the disc with reduction is characterized by the appearance of clicks in the temporomandibular joint when opening and closing the mouth. A click when opening the mouth occurs when the articular head moves along the posterior surface of the disc and the normal relationship between the head of the temporomandibular joint and the concave lower surface of the disc is restored. The clicking sound when closing the mouth reflects the reverse process. The articular head slides backwards over the posterior surface of the disc and stops behind the disc. It is assumed that such a change in function is associated with unevenness of the articular surface, the formation of adhesions between the articular surface and the disc, changes in the properties of the synovial fluid, impaired interaction between the disc and the condylar process due to muscle dysfunction, increased muscle activity in the joint area or disc deformation. As disc dysfunction progresses, it begins to interfere with the normal movement of the condylar process and can cause intermittent blockage of the temporomandibular joint. Sometimes the patient opens his mouth too wide due to weakness of the ligamentous apparatus and hypermobility in the joint, which is associated with the risk of block or subluxation in the joint.
Displacement of the disc without reduction is characterized by a pronounced restriction of opening of the mouth when the process of normal sliding of the condyle along the disc is disrupted due to disc adhesion, deformation or dystrophy. In this situation, the opening of the mouth is usually limited to 20-30 mm in combination with the deviation of the lower jaw to the affected side when opening the mouth. Joint noise is minimally expressed due to the fact that the movement in the joint is sharply limited. The masticatory muscles and joint often become painful to palpation due to joint dysfunction. With persistent disc displacement, soft tissues reconstruct the disc and ligamentous apparatus in the joint. After persistent blockage, routine daily chewing functions promote adaptive changes in tissues adjacent to the posterior surface of the disc and collateral ligaments, resulting in pain relief and normal mouth opening. Further adaptation of the joint includes reconstruction of the surface of the condylar process, glenoid fossa and articular eminence, with corresponding radiological changes. Disc perforation can cause degenerative changes and severe crepitus when opening and closing the mouth. Successful re-modeling helps to restore normal mouth opening with minimal pain, although articular noise often persists. However, in some cases degenerative changes in bone tissue progress, leading to the development of erosive changes, a decrease in vertical size, malocclusion, increased pain in the joint and muscles and severe dysfunction of the lower jaw.
Disc injury and arthralgia of the temporomandibular joint are at least partly related to abnormal biomechanical stress on the condylar process.
which leads to a change in the size, shape and function of the tissues of the joint. Friction resulting from joint dysfunction and abnormal disc position can exacerbate both jaw displacement and changes in the shape and function of the disc. In other cases, triggers can be jaw injuries, accidental biting of a hard object, or improper chewing. Sometimes, the development of arthralgia in the temporomandibular joint and disc displacement can be caused by "whiplash".
Temporomandibular joint disc displacement is common in the general population, but in most cases, joint function is preserved and does not require treatment. If the patient applies for medical help about the appearance of noises in the temporomandibular joint in the absence of other symptoms, in these cases, long-term observation, patient education and the patient's mastery of self-help methods are sufficient. Pain, intermittent blockage, and difficulty moving the jaw require close monitoring, possibly with therapy.
Subluxation or dislocation of the temporomandibular joint with or without disc displacement is characterized by joint hypermobility due to weakness of the ligamentous apparatus. Subluxation of the temporomandibular joint can be triggered by dental manipulations with wide, prolonged opening of the mouth, especially in patients with systemic hypermobility of the joints. The condylar process is displaced anteriorly with respect to the disc and the articular eminence and cannot return to the closed position due to the fact that normal sliding in the posterior direction is blocked. In most cases, the condylar process can be displaced laterally or medially by the physician or patient to help remove the block and allow the mouth to close properly. If the blockage of the joint cannot be eliminated by these influences, additional manipulations (lower jaw downward and forward) may be required to return the lower jaw to its original position.
Temporomandibular joint osteoarthritis is characterized by degenerative beating of the articular surfaces, which can cause crepitus, joint dysfunction, and radiographic changes. In osteoarthritis, degenerative changes are accompanied by the appearance of spontaneous pain, tenderness in the joint area on palpation, and the development of inflammation. Osteoarthritis can develop at any stage of disc displacement, as well as as a result of trauma, infection and other damaging factors that cause disruption of the integrity of the joint, or in rheumatic or other conditions that can cause polyarthritis. Such diseases include systemic osteoarthritis, rheumatoid arthritis, psoriasis, systemic lupus erythematosus, scleroderma, Sjogren's syndrome and gout. Consultation with a rheumatologist is indicated if there is pain, swelling, redness, stiffness, or crepitus in the temporomandibular joint (as well as in other joints).
Other diseases of the temporomandibular joint include ankylosis, traumatic joint injury and fractures, neoplasms and malformations. Ankylosis or complete absence movements in the joint can be associated with the formation of bone or fibrous fusion between the articular head and the glenoid fossa. Extracapsular pathological processes such as coronoid injury or muscle contracture can also cause significant limitation of mandibular movement. The most common traumatic injuries include contusion (contusion) with hemorrhage into the joint cavity, the neck of the condylar process, the articular head, or the external auditory canal. TMJ injuries are usually associated with pain and limited range of motion in the joint. Malformations, primary benign and malignant tumors, myxoma, fibrous dysplasia, metastases, or local invasion of the joint malignant tumors from neighboring regions are also found, but belong to rare reasons lesions of the temporomandibular joint.
