Pain in the left cheekbone when opening the mouth. Causes of pain in the jaw joint
Pain in the jaw joint area may indicate the development of inflammation and dangerous diseases. Let us consider in more detail the symptoms of inflammation of the jaw joint and the most affective methods of treatment.
Inflammation of the jaw joint: the main causes of the disease
Most often, the jaw joint becomes inflamed for the following reasons:
1. Mechanical injury. It can be a fall or a blunt blow to the jaw, in which soft and bone tissues are severely injured. Also, if the jaw is injured, you may experience:
Hematoma formation;
Rupture of the inner capsule of the joint;
Crack or fracture.
As a result of trauma, inflammation occurs in the joint cavity. This leads to the accumulation of fluid and a sharp deterioration in the mobility of the jaw.
2. Getting an infection also threatens the development inflammatory process. The infection itself can enter the joint in the following ways:
Direct (with a fracture, bullet wound, knife cuts, etc.);
Contact (for diseases such as abscess, phlegmon, furuncle, purulent parotitis and otitis media);
Hematogenous (develops in acute fungal, bacterial or viral diseases).
Usually hematogenous infection occurs with such diseases:
Gonorrhea;
Syphilis;
Diphtheria;
Tuberculosis;
3. Rheumatoid arthritis quite often become the cause of inflammation of the jaw joint. With this disease, a person is strongly affected soft tissue joints. Inflammation of the jaw occurs in almost 20% of patients.
To date, there is no exact information about the causes of the development of rheumatoid arthritis. Scientists identify the provoking factors of the disease. They are hereditary predisposition and various viral infections(hepatitis, herpes, etc.).
4. Lupus erythematosus is a disease in which a person's immune system is disrupted and joints are damaged. It is also important to know that the joints themselves are not deformed in this case, therefore, after healing, the discomfort may disappear altogether.
5. Reactive arthritis accompanied by severe inflammation of the joints (including the jaw joint). It arises after earlier previous infection v genitourinary system or intestines. The very deterioration of the condition of the joints occurs due to the defeat of some microorganisms of the patient's tissues.
6. Gout accompanied by metabolic disorders, due to which the patient begins to deposit uric acid in the tissues of the body.
This disease usually develops due to malnutrition, with a lack nutrients or a sedentary person.
Because of large congestion of this substance to the blood, salt begins to collect in the joints, which leads to the development of inflammation, acute pain and burning.
Inflammation of the jaw joint: symptoms and manifestations
Acute inflammation of the jaw joint is accompanied by the following symptoms:
1. Pain. This is the most frequent symptom inflammation. The nature of the pain can be different: sharp, aching, stabbing and cutting. Intensity - Strong and repetitive (especially after chewing food).
Also, sometimes pain can be given to other parts of the face ( upper jaw, ears, etc.). This is due to the fact that different parts of the soft tissues on the face are innervated by the same nerve that passes through the jaw joint.
2. Redness and severe swelling it is most characteristic of acute arthritis (purulent form), in which pathogenic microbes collect in the joint.
3. The increase in body temperature is primarily associated with the expansion of blood vessels and the flow of warm blood to the area of the inflammatory process. This provokes the development of such a symptom.
4. A feeling of fullness and squeezing in the joint is observed due to tissue edema.
5. Hearing impairment can occur due to the spread of inflammation. It is also important to know that with infectious inflammation, the disease can spread to inner ear, causing complete deafness.
6. Rapid fatigue.
7. Fever.
8. Body aches.
9. Weakness.
10. Loss of appetite.
11. Apathy.
12. Pain when eating.
13. Frequent pain in the head.
14. Sharp rise blood pressure and exacerbation of hypertension.
Symptoms of chronic inflammation in jaw joint are:
1. It's a dull pain... In this case, its intensity will not be so pronounced, but at the same time it will deliver to the person no less unpleasant sensations, than in acute form... Also, pain can be paroxysmal and occur at any time.
2. Impaired joint mobility. This will be especially evident in the morning.
3. The appearance of a crunch in a sore joint, which may be accompanied by painful sensations.
4. Slight rise in temperature.
5. Chronic weakness.
6. Slight hearing loss (may be in one ear).
Jaw joint inflammation: diagnosis and treatment
Due to the fact that a variety of diseases can cause inflammation in the jaw joint, it is important to identify the source of the disease before starting treatment. To do this, you should go through the following diagnostic procedures:
1. General analysis blood.
2. General analysis of urine.
3. Revealing the level of uric acid.
4. Analysis for the amount of protein.
6. X-ray of the jaw joint.
It is also advisable to visit such doctors:
1. Traumatologist.
2. Neurologist.
3. Therapist.
4. Rheumatologist.
5. Dentist.
6. Otorhinolaryngologist.
Inflammation of the jaw joint: treatment methods
Traditional treatment of inflammation of the jaw joint includes the following techniques:
Immobilization;
Drug treatment;
Physiotherapy treatment.
1. Immobilization. It is indicated for dislocations, stretch marks, bruises and joint injuries, which led to the development of inflammation. The main task immobilization is the immobilization of the affected joint. For this, a soft chin bandage, sling-like or parieto-chin bandage can be applied to the patient's face.
Depending on the severity of the patient's condition, he should wear such a bandage from several hours to several weeks.
2. Drug treatment. It is aimed at relieving pain, swelling and improving blood circulation. Most often, the following groups of drugs are prescribed to the patient:
Anti-inflammatory drugs (Nimesil);
Non-narcotic analgesics (Paracetamol);
At severe pain narcotic pain medications (Tramadol, Morphine) may be prescribed;
Cytostatics for inflammation (Cyclophosphamide, Azathioprine).
It's important to seem that these drugs can be taken both orally in the form of tablets and injected.
3. Physiotherapy usually done after drug treatment as a restorative procedure. The duration of such treatment is determined by the attending physician, depending on the severity of the disease and the patient's condition.
Traditional physiotherapy treatment includes the following set of procedures:
1. UHF therapy. It aims to impact electric field on the affected tissue. In this case, the energy that is emitted by this field will be absorbed by diseased cells, which will lead to an improvement in blood circulation and normalization of the endocrine systems.
Also, UHF therapy has the following therapeutic effects:
Relieves pain;
Nourishes tissues;
Relieves inflammation;
Improves metabolism in the patient's tissues.
To achieve maximum therapeutic effect this procedure should be done twice a day for fifteen minutes. The general course of treatment should not be longer than two weeks. You can repeat it after two months.
2. Electrophoresis- This is one of the types of physiotherapy procedures, which involves treatment with electric current and various medications. When the current hits the diseased area, it has the following therapeutic effect:
Pain relieves;
Relieves inflammation in the joint;
Relaxes;
Improves blood circulation.
Most often, for diseases of the joints, doctors use electrophoresis with novocaine. It effectively relieves pain.
In this case, the solution with this drug is applied to electrophoresis, after which it is applied to the patient's body. After filing electric current the medicine will affect the affected area.
The duration of this procedure is 20 minutes. The course of treatment should include at least 14 sessions.
Diagnosis of TMJ lesions is complicated by the fact that this pathology has a lot of symptoms. But some of them can be called classic - those that affect the TMJ joints themselves, ears, head, face and teeth. Since the joints nerve endings no, when their function in this area is impaired, the person does not experience pain. It occurs in the ears, in the neck, head, or at trigger points, which are seals in the muscles (masticatory, temporal, sublingual, temporal, cervical) - pain is felt when pressed on them. At the same time, one can feel noise in ears, crunching in the joints when opening the mouth.
The most common symptom is clicking in the joint of the lower jaw, and not always accompanied by pain. The sound made by the jaw can be heard by others. If the jaw clicks, then the disc is misaligned and the muscles supporting the lower jaw while chewing food are unnaturally tense. This tension results in pain in the muscles, face, head and neck.
Blocking, or locking, of the TMJ is a condition in which the joint moves unevenly due to the abnormalities that have occurred in it. A person notices that the lower jaw opens unevenly, as if catching something. And to open your mouth wide, you first need to move lower jaw then in one direction, then in the other direction, sometimes it has to be done until a click is heard at the point of its "unlocking".
Due to the proximity of the TMJ to auricles, his defeat often causes pain in the ear, his congestion, up to hearing loss. Tinnitus can cause both joint disorders and pain management with drugs (aspirin, ibuprofen).
Prophylaxis
Prevention is a timely and high-quality treatment and prosthetics of teeth, correction of occlusion, timely seeking help from a doctor after an injury.
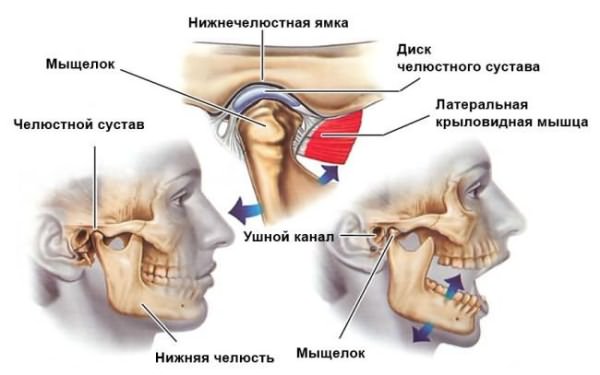
Temporal mandibular joint(TMJ) is a paired formation located behind the earlobe. It connects temporal bone skull with the lower jaw and provides its movement in three directions. Any deviations in its work or adjacent structures cause pain, discomfort and impaired articulation.
The jaw joint refers to combined type: movement from the left and right side are carried out synchronously. It consists of:
The joints move in three planes:
- frontal - up and down;
- sagittal - forward and backward;
- vertical - in the lateral direction.
The blood is supplied by the branches of the external carotid artery, and its outflow is provided by the venous network of the jaw. The outflow of lymph is carried out into the cervical lymph nodes. Because of this, their increase is one of the symptoms of TMJ inflammation.
Important! The innervation of the TMJ is provided by the ternary nerve. Therefore, the reason why the jaw hurts may be hidden in the pathologies of other parts of the face.
Causes of pain
Pain in the jaw joint may appear due to:
- Mechanical injuries: bruises, fractures, dislocations. They are accompanied by hemorrhage into the joint cavity, rupture of the capsule, ligaments, and cracks in the superficial bones.
- Infection. It occurs due to the penetration of pathogenic microorganisms into the cavity. Infection is possible when:
3. Systemic inflammatory diseases:
- arthritis - inflammatory pathology caused by viruses and infections, it can affect any joint: jaw, knee, elbows, shoulder, ankle;
- arthrosis - the jaw joint is destructively damaged;
- systemic lupus erythematosus - antibodies begin to attack the intracellular structures of the body, while there is no structural deformation;
- gout - accompanied by impaired excretion or increased production of uric acid, which accumulates in the tissues.
4. Neoplasms:
- benign: adamantinoma, osteoma, osteoblastoclastoma;
- malignant: sarcoma, cancer.
Important! TMJ can also hurt due to malocclusion, advanced carious lesions, trigeminal neuralgia, facial artery arteritis, improperly installed orthodontic (braces) and orthopedic structures (bridges, prostheses).
Symptoms
Pain in the temporomandibular joint is local or radiating. Local signs of dysfunction include:

Also, TMJ dysfunction is accompanied by radiating pain in the head, facial muscles, ears, neck and upper back. Often, diseases of the jaw structures lead to impaired auditory and visual functions, dizziness, disorientation in space.
Important! Due to irradiating pain, disruptions in the work of the TMJ are often confused with pathologies of other organs: migraine, periodontal disease, teeth, violation of the mechanism of equalization of intra-ear pressure.
How to relieve pain?
Cure diseases on your own temporomandibular joint impossible. For correct therapy, careful diagnosis and identification of the exact cause of the inflammation is required. However, a number of measures will help reduce pain syndrome before visiting a doctor:
- Applying cold. Ice wrapped in a towel or dampened cold water The scarf is applied to the affected area. The procedure time should not exceed 15 minutes, the subsequent session is carried out at least one hour later.
- Warm compresses. The jaw joint is warmed with a bag of salt, paraffin, and a damp heated towel.
- Taking analgesics. They will help to temporarily remove sharp pain... Recommended "Ketanov", "Nurofen", "Nise".
- Reduce chewing stress. It is necessary to eat non-solid foods: cereals, soups, grated fruits, vegetables, dairy products... It is also best to sleep on your side or on your back to avoid squeezing your jaw while resting.

A warm compress relieves pain.
Important! If not known true reason, because of what the jaw joint hurts, are excluded from the list of what can be done warm compresses- they accelerate the spread of infection.
Diagnostics
Initial diagnosis TMJ dysfunction is carried out by a general dentist. Depending on the cause of the lesion, he can refer to a specialist in another direction:
- surgeon;
- traumatologist;
- neurologist;
- orthopedist;
- gnathologist;
- rheumatologist;
- otolaryngologist.
During the examination, the patient is initially interviewed, visual examination and palpation. To clarify the cause of dysfunction, you need to do:
Treatment
Treatment for TMJ dysfunction depends on the type of pathology and the cause of its occurrence. There are several methods of therapy:
- Immobilization. It is used for traumatic injuries after appropriate measures: reduction of dislocation, comparison of bone fragments. Immobilization of the jaw is also necessary if there is a possibility that the jaw joint may move or if a fracture is suspected.
- Drug therapy. Aimed at eliminating pain and suppressing the growth of pathogenic microorganisms. Appointed:
- analgesics: paracetamol, Nurofen;
- non-steroidal and steroidal anti-inflammatory drugs: Diclofenac, Nimesil, Affida Fort, Prednisolone;
- antibiotics: "Amoxicillin", "Tetracycline";
- antifungal agents: Nystatin, Fluconazole;
- cytostatics: "Methotrexate", "Sulfasalazine".
3. Physiotherapy. Apply after removal acute symptoms... Most often they are prescribed:

4. Surgical intervention. Used when other treatments fail positive result or with extensive damage (fractures with displacement and multiple fragments). Also, indications for the operation are infectious processes, for example, purulent arthritis. The technique consists in opening the cavity, cleansing it of pus and areas of necrosis.
Important! As complementary therapy appoint remedial gymnastics increasing the mobility of the jaw.
Possible complications
Lack of correct therapy for TMJ diseases can lead to structural changes in the joint itself, adjacent tissues and the further spread of infection. Possible complications include:
- Loss of mobility - ankylosis. It occurs due to the fusion of the articular surfaces. The reasons are tissue overgrowth during infectious processes and after fractures.
- Destruction of structural parts. It occurs against the background of damage by staphylococci and streptococci. Leads to complete or partial limitation of mobility.
- Meningitis. The lining of the brain becomes inflamed if the infection begins to spread along the ascending pathway.
- Phlegmon. A purulent process in adipose tissue develops against the background of inflammation with a decrease in the body's immune forces.
- Sepsis. The penetration of the infection into the bloodstream and its further spread.
The jaw joint is affected by injury, infection and development systemic diseases... Due to the peculiarities immune system and natural wear and tear, this pathology is often observed in the elderly. Its treatment is carried out only by a specialist after thorough examination and establishing the cause of the inflammation.
