Colposcopy of the cervix - why is it needed, how it is performed and deciphered. Why is a pap test prescribed, how is it carried out, decoding of the analysis
The vaginal part of the cervix - ectocervix is lined with stratified squamous non-keratinized epithelium. In women of reproductive age, it is constantly rebuilt by proliferation-maturation-desquamation and is completely replaced by a new population of cells every 4 to 5 days.
Normally, squamous epithelium is the following types cells: cells of the superficial layer, cells of the intermediate layer and cells of the basal-parabasal layer. Cellular composition depends on the presence/absence menstrual cycle and its phases. The squamous epithelium performs a protective function.
The cervical canal - endocervix - is lined with a cylindrical mucus-producing epithelium. Cyclic changes in the epithelium of the endocervix are poorly expressed. The main function of the cylindrical epithelium is secretory.
The transformation zone is the junction of the stratified squamous and columnar epithelium in women of reproductive age, which basically coincides with the area of the external os. Depending on age and hormonal balance in the body, it can also be located on the vaginal part of the cervix. In women of older reproductive and postmenopausal age, the boundary line is actually localized within the external pharynx. According to statistical data, precancer occurs from the zone of transformation.
Material for research. In the direction for the cytological examination of biological material, clinical data, diagnosis, features and place of obtaining the material, data on the menstrual cycle must be indicated.
Swabs are taken prior to bimanual examination and colposcopy. The instruments used must be sterile and dry, as water and disinfectant solutions destroy cellular elements.
During a preventive examination (cytological screening) of women, it is advisable to obtain cellular material from the surface of the vaginal part of the cervix (ectocervix) and walls cervical canal(endocervix), in the presence of pathological changes in the cervix aimingly.
Modified Eyre-type spatulas or Cervix-Brash, Papette brushes are used as a tool for taking material from the cervix during a preventive examination of women. For diagnostic purposes, the material is obtained separately with spatulas from the ectocervix, brushes such as Cytobrash from the endocervix.
Material for cytological diagnostics is obtained different ways: aspiration and scraping of the contents of the posterior fornix of the vagina, cervix or obtaining a smear-imprint. Received biological material applied in a thin layer on a glass slide and dried in air. The glass must be marked with not only the last name / code, but also the place where the cell material was taken (cervix, cervical canal). The markings on the slide and in the direction for cytological examination must correspond to each other.
Please note that in children under 16 years of age, gynecological tests are taken only in the presence of parents. Medical offices do not do cervical scrapings and swabs for pregnant women 22 weeks or more, as this procedure can cause complications. If necessary, you can contact your doctor to take the material.
Preparation conditions are determined by the attending physician. In women of reproductive age, smears should be taken no earlier than on the 5th day of the menstrual cycle and no later than 5 days before the expected start of menstruation. You should not take cell material for research within 24 hours after sexual intercourse, sanitation of the vagina, introduction of medications into the vagina.
Referral Form
Cytological smears should be taken from all women over 18 years of age, regardless of clinical data, once a year. In the presence of clinically pronounced pathological changes in the cervix, the cellular material is taken aimingly. The frequency of cytological examination is determined by a gynecologist (at least 2 times a year). (Order No. 430 "On the approval of instructive and methodological guidelines for the organization of work antenatal clinic"dated April 22, 1981 of the Ministry of Health of the USSR).
The cytological method of research occupies one of the important places in the diagnosis of diseases of the cervix. Due to its high accuracy, it is one of the leading research methods in the diagnosis of background, precancerous and cancerous processes of various localization.
Advantages of the method:
- painlessness and safety of obtaining cellular material;
- the possibility of studying the pathological focus in dynamics;
- the possibility of diagnosing a malignant neoplasm in the initial stage of development;
- small financial costs.
Disadvantages of the method:
- the impossibility of establishing signs of infiltrative growth (cell, not tissue material is examined).
The specificity of this screening method is 69%. The rate of false-negative smears ranges from 5 to 40%. Inadequate sampling from the endocervix is the most an important factor leading to false negative results.
The effectiveness of the cytological method of research in to a large extent depends on the preanalytical stage: how correctly the cell material is taken and the smears are prepared.
The interpretation of the results of the study contains information for the attending physician and is not a diagnosis. The information in this section should not be used for self-diagnosis or self-treatment. An accurate diagnosis is made by the doctor, using both the results this survey, and the necessary information from other sources: anamnesis, results of other examinations, etc.
It should be remembered that the cytological method of research, like any other laboratory method research does not always provide comprehensive information for making a diagnosis. Only a clinician has the right to make a final diagnosis (based on the study of anamnesis, observation of clinical manifestations and data from the histological method of examination).
The result of a cytological examination of the obtained biomaterial (imprint smears) can be presented by a cytologist in the form:
- descriptions of the cellular composition;
- descriptions of the cellular composition and conclusions;
- descriptions of the cellular composition and conclusions in a hypothetical form;
- descriptions of the cellular composition and recommendations.
The form of the answer depends on a number of reasons: the adequacy of the cellular material (few cells, a lot of blood elements, mucus), an incorrectly completed referral for a cytological examination: the reason for the examination (clinical diagnosis) was not indicated, the presence / absence of menstruation; it is not indicated where the material came from, the marking in the direction does not correspond to that on the glasses, etc.
Result interpretation
Possibilities of cytological diagnosis of certain diseases of the cervix and options for interpreting the results of a cytological study:
Endocervix.
Normally, with correctly obtained cellular material from the transformation zone (ZT) - the junction zone of the squamous and columnar epithelium - cells of the squamous and columnar epithelium are present in the smear without changes. Cytological conclusion: cells of squamous and cylindrical epithelium without features were found in the obtained material. The presence of a small number of metaplastic epithelial cells is an indication that the material was obtained from ST. In the absence of the above description, the swab was not taken from ST and the patient cannot be said to be at no risk of cervical cancer. Such swabs are commonly seen in postmenopausal women and patients who have undergone cervical treatment that has moved the borderline into the cervical canal. Depending on the patient's history, this may be a reason for re-sampling the material.
Clinical diagnosis in the direction of the polyp of the cervical canal, and the corresponding cytological picture allow the cytologist to conclude that the cytogram corresponds to the clinical diagnosis of the polyp of the cervical canal. If there is no clinical diagnosis, and the cellular composition is represented by large clusters of cells of the cylindrical epithelium, the cytologist gives a descriptive answer with the assumption of hyperplasia of the cells of the cylindrical epithelium or a polyp of the cervical canal.
Ectocervix. IN reproductive age Normally, the cellular composition of imprints from the vaginal part of the cervix is represented by squamous epithelial cells, predominantly of a superficial or intermediate type. The wording “in the obtained material cells of the squamous epithelium of the surface layers without features are noted” indicates that the obtained biological material consists of cells of the squamous epithelium of the surface and intermediate layers in various combinations in accordance with the phase of the cycle. At the beginning of postmenopause (normal), cells of the squamous epithelium of the intermediate layer are noted in the smear. In some women, during the whole subsequent life, an intermediate type of smear (squamous epithelial cells of the intermediate layer) is observed, sometimes with the presence of cells of the surface layer, which is apparently associated with adrenal function, an active sexual life. The presence in the preparation of cells of the squamous epithelium of the surface layer (estrogenic type of smear) in the first 5 years of menopause should be alarming in relation to neoplasms of the ovaries, uterine fibroids. Postmenopause is characterized by the presence of cells of the basal-parabasal layer (i.e., deep layers).
Erosion (ectopia) of the cervix. The concept of cervical erosion (true erosion) involves a defect in the cervical mucosa caused by various diseases(syphilis, traumatic injuries, consequences of radiation therapy, cervical cancer, etc.). The term cervical ectopia (pseudo-erosion) means the displacement of a high cylindrical epithelium on the vaginal part of the cervix. Subject to the presence in the direction of the clinical diagnosis of "erosion / ectopia of the cervix" and the correct sampling of biomaterial from the ectocervix (cellular material is represented by cells of the squamous epithelium of all layers in various combinations, clusters of cells of the cylindrical epithelium, elements of inflammation), the cytological conclusion has following form answer: the cytogram corresponds (does not contradict) the clinical diagnosis - erosion of the cervix.
Cytological conclusion: The cytogram corresponds (does not contradict) the clinical diagnosis of cervical ectopia suggests the presence in the obtained material of squamous epithelial cells of the surface layers, clusters of cylindrical epithelium cells.
Conclusion: a cytogram of endocervicosis takes place if the clinical diagnosis of erosion / ectopia of the cervix is not indicated in the direction for a cytological examination, and cells of the squamous epithelium and clusters of cells of the cylindrical epithelium are morphologically noted.
It is not always possible to make a cytological diagnosis between superficial endocervicosis (ectopia of the cervix) and proliferating endocervicosis. A descriptive cytological response occurs when:
- in the material obtained from the ectocervix, cells of the squamous epithelium and single clusters or single cells of the cylindrical epithelium were found;
- cellular material obtained from ecto- and endocervix and presented in one mixed smear;
- smears are not smeared.
With healing endocervicosis, a large number of cells of metaplastic epithelium are found in smears (metaplasia is the replacement of one type of epithelium with another). Metaplastic epithelium is a target for human papillomavirus exposure - an area for the development of precancerous conditions. The presence in smears from the cervix of a small number of cells of metaplastic epithelium is an indicator of a normal physiological process.
Histogenetic mechanisms of replacement of columnar epithelium by squamous:
- progression of squamous transformation - direct ingrowth of native epithelium under the cylindrical. As the squamous cells develop and mature, the endocervical cells move upward, degenerate, and eventually slough off. A similar process is observed during re-epithelialization of true cervical erosion healing;
- squamous metaplasia - proliferation of undifferentiated reserve cells of the endocervical epithelium and their partial transformation into a fully mature squamous epithelium. The first stage of the process is the appearance of reserve cells, then comes reserve cell hyperplasia, followed by differentiation into immature squamous epithelium, and at the final stage mature squamous epithelium is observed.
Leukoplakia of the cervix. With the cytological method for diagnosing simple leukoplakia (a benign lesion of the cervix, an underlying disease), hyperkeratosis is detected, i.e., in the material obtained from the ectocervix, layers (clusters) of squamous epithelium scales were found (there is no nucleus in the cytoplasm of the cell), separately lying squamous epithelium scales, dyskerocytes . If there is a clinical diagnosis of "leukoplakia of the cervix" - in the cytological report it is noted that the picture does not contradict the clinical diagnosis - leukoplakia of the cervix. In the absence of a clinical diagnosis of cervical leukoplakia, depending on the available material, the cytologist gives a descriptive answer, possibly with a recommendation to exclude cervical leukoplakia. Single squamous epithelium diagnostic value Dont Have. Leukoplakia with atypia - a cytological method of research is not always possible to identify, which is explained by the presence of squamous epithelium scales on the surface of the stratified squamous epithelium, which prevent the receipt of cellular elements. It is necessary to conduct a morphological study of the biopsy of the cervix.
Dysplasia of the cervix. Dysplastic changes occur in the stratified squamous epithelium of both exocervix and endocervix. As a rule, changes begin at the junction of the squamous and columnar epithelium. Dysplasia can simultaneously develop in several areas of the cervix and cervical canal, often changes are expressed to varying degrees. Spectrum dysplasia (CIN) is not a single disease. There are two biological essences of the process: a productive human papillomavirus infection and a cancer precursor.
Dysplasia-I (mild dysplasia, CINI) is one of the least reproducible cytological diagnoses. Dysplasia-I is often difficult to differentiate from reactive epithelium. Conduct differential diagnosis between dysplasia III (severe dysplasia, CIN-III) and intraepithelial cancer by cytological research is not always possible.
Cytological conclusion: Dysplasia - I (weak, CIN-1); Dysplasia -II (moderate, CIN-II); Dysplasia -III (severe, pronounced, CIN-III).
If there are cells with signs of malignancy in the obtained material, the cytologist gives a conclusion on the cytogram of the malignant neoplasm and, if possible, specifies the form of cancer.
Inflammatory processes of the cervix. Inflammation - a cellular reaction (in the focus) - is represented by a degeneratively altered epithelium, proliferative changes of a reparative, protective nature, and inflammatory atypia. In an acute nonspecific inflammatory process, a pronounced leukocyte infiltration (many neutrophilic leukocytes), incomplete phagocytosis is noted in the smear. The composition of the cell population of the epithelium may change. Cytological conclusion: cytogram of ecto-/endocervicitis. In subacute and chronic inflammation, eosinophils, lymphocytes, macrophages / cells of the type foreign bodies(multinuclear macrophages) - cytological conclusion: cytogram of chronic ecto-/endocervicitis. Acute inflammatory processes are more often observed in age group 20 - 24 years old, chronic processes and their consequences occur in women 25 - 34 years old.
Infectious lesions of the cervix. Cytological features of smears for infectious lesions of the cervix depend on the pathogen and the duration of the inflammatory process.
Mycoplasmas, ureaplasmas and corynobacteria as the cause of inflammation is observed in a group of young women (up to 20 years). In the age group over 30 years, anaerobic microorganisms occupy the first place among the causative agents of inflammatory processes in the genitals. Mixed infection increases the pathogenicity of each of the pathogens. In such cases, inflammation causes a pronounced tissue reaction, accompanied by damage to the epithelium, destruction and dysplasia. This leads to the development of not only colpitis, endocervicitis, but can play a significant role in the formation of cervical ectopia. Incomplete phagocytosis is noted (phagocytic activity of leukocytes is suppressed). The cytological conclusion indicates the type of flora with a recommendation to exclude certain kind infections.
Bacterial vaginosis(BV) - (clinical diagnosis). In cytological preparations, BV is represented by key cells. If the key cells are not found, and the flora is cocco-bacillary, it is recommended to exclude the presence of gardnerella (ureaplasma) in the cytological response; in the presence of bacilli mobiluncus, a recurrence is possible pathological process after the treatment.
Genital herpes- Herpes simplex virus has a high tropism for epithelial and nerve cells. Relapses are mainly due to the persistence of infection in the nerve ganglion. Cytological examination of the obtained material may show changes in squamous epithelial cells specific for their defeat by this type of viral infection: multinucleated cells of the "mulberry" type. Form of cytological response: signs of a viral infection were found in the material obtained. It is recommended to exclude the herpes simplex virus.
Papillomavirus infection of the genitals. The human papillomavirus is able to persist for a long time in the basal layer of the squamous epithelium, which causes a high frequency of recurrence of the process. The frequency of coincidence of cytological and histological diagnoses in condyloma was 42%: CIN-I - 56%, CIN III 74%. False-negative cytological responses are explained by the consequence of incorrect material sampling - 90%, incorrect interpretation - 10%.
In addition, underdiagnosis in cervical smears may be due to the presence of koilocytes in the deeper layers of the squamous epithelium or the presence of a large overlap of elements of inflammation and flora. Cytological conclusion: the obtained material showed signs of a viral infection. It is recommended to rule out the human papillomavirus. Indirect changes characteristic of a viral infection: an increase in the size of the nucleus, nonspecific multinucleation. The form of the cytological response: in the received material, indirect signs viral infection. It is recommended to exclude the herpes simplex virus, human papillomavirus.
Trichomoniasis. An inflammatory reaction develops in the presence of a large number of protozoa. For the quality of research, it is important proper preparation patient. Termination of the use of trichomonocidal drugs for 5-7 days before taking the material. In the cytological preparation, there are signs of an acute/chronic inflammatory process, mixed flora, Trichomonas. Cytological conclusion: trichomonas colpitis.
Chlamydial infection. Chlamydia are tropic to columnar epithelium. Often found in women with cervical ectopia. In pregnant women and menopausal women, signs of infection may be observed in the squamous epithelium. They can also be found in macrophages. Cytologically, the presence of intracellular specific inclusions is determined, which are more often detected with a fresh or untreated infection. Cytological forms of response: cells with cytoplasmic inclusions morphologically similar to chlamydial infection were found. It is recommended to exclude the presence of chlamydial infection.
Squamous intraepithelial lesions(PIP) of the cervix are associated with significant qualitative and quantitative changes in the vaginal microflora. Deficiency of lactobacilli is observed in all patients with PIP, there is an increase in representatives of opportunistic flora. In the cytological conclusion, changes in the flora are indicated, if possible, a representative of the opportunistic flora is characterized. The presence of nonspecific vaginosis is noted.
Fortunately, my goal is not to write a new textbook on colposcopy. After Bauer and Rogovskaya, this niche is closed for 20 years. We will consider the goal of the manual "for dummies" not to learn how to do colposcopy, but to figure out what colposcopic terms mean, and approximately understand "what is good and what is bad" 
The most difficult thing is to figure out what the norm is.
I remind you that the visible part of the cervix is covered with stratified squamous epithelium, the cervical canal is lined with a single-row cylindrical epithelium that secretes mucus. Between them is the transition zone, or the transformation zone - the most delicious zone, because cancer begins there.
So we have to find stratified squamous epithelium, columnar epithelium and transformation zone.
Rule number 1 - you can't see shit without vinegar
How it works and how Hans Ginselman came up with this idea is still unclear. If someone needs details - ask in the comments, but before the vinegar treatment, the "incomprehensible red spot" remains a red spot, just increased in size. Acetic acid removes superficial mucus and makes all tissues more prominent, voluminous, pathological areas begin to turn white rapidly, cylindrical epithelium appears and becomes similar to red caviar or grapes.
The zone between the cylindrical and stratified squamous epithelium is called the transformation zone, or transition zone, and the epithelium in this zone is called metaplastic. Such an epithelium is thin, pale, contains "holes" and "dots". "Holes" - open ducts of the cervical glands that produce mucus. "Points" - ducts of the glands, covered with a cover of squamous epithelium. If, after the lid has closed, the gland continued to produce mucus, a "pimple" is formed - a retention cyst, or Naboth's cyst, or Ovula Nabothii. In the photo, such "pimples" are marked with numbers - Naboth's cysts. This is a variant of the norm, in most cases, no activity is needed. 
The cylindrical epithelium can be located on the neck quite confidently, then we are talking about ectopic columnar epithelium
I repeat for the 100500th time - the ectopia is precisely the cylindrical epithelium, not the cervix. You can say "ectopia ON the cervix", the cervix itself has not been ectopic anywhere, it does not stick out of the vagina. But this is already grumbling and senile tediousness.
Survey simple colposcopy - an incomprehensible red spot 
the photo sucks (by the way, it is rather difficult to make a normal one) - what was red became light and grainy, clear edges appeared 
It's perfect healthy woman. We see a cylindrical epithelium, loosely located on the neck, a thin border of the transition with a well-defined open gland and a pale stratified squamous epithelium. It is necessary to turn pale, because after treatment with vinegar, numerous subepithelial vessels are reduced. ![]()
To clear our conscience, we carry out a Schiller test - we process the neck aqueous solution iodine.
Abnormal colposcopic areas never stain Brown color because atypical cells do not store glycogen. They don't need supplies - they just want to eat and multiply. 
- Oh God! What is this? Huge anomalous area?
No, it's just a cylindrical epithelium. It also does not stain with iodine at all and this is completely normal.
I can't help but remember the magic story.
When I moved to Khimki, for some time I had a strong feeling that I had lost my mind. So amazing things happened in the local residential complex that I seriously thought about my mental health. It is known that only the flu gets sick together, they go crazy alone.
For a while I sat on "paid services". That sounds good, but it's actually complete nonsense. On paid services only those who do not come compulsory medical insurance policy. By the way, they don’t have any money either, so for 300 rubles at the cash desk it was necessary to heal from all diseases, preferably without tests, ultrasound and other “divorce”
In the "paid" office there was a decent video colposcopic system. One day, quite unexpectedly, I took part in a consultation.
Two doctors put the patient on the chair, exposed the neck in the mirrors, treated it with iodine and began to look for the iodine-negative zone. Moreover, inside the unstained area, they saw some less unstained area and tried to draw some conclusions. My opinion was also asked, purely out of courtesy. I had to answer that without vinegar treatment, I don’t understand anything on the neck at all. They looked at me with pity. I looked at the monitor, the picture was approximately the same as in the previous photo. It was difficult to remain silent, so I said that the cylindrical epithelium is not stained with iodine in principle, so it is pointless to look for an anomalous zone here. The look of my colleagues ceased to be meaningful. I probably said something too complicated or indecent.
From 2008 to 2010, I had endless conflicts with the local manager
- What are you doing? Why do you need an extended colposcopy? Keep it simple! You don't need plain vinegar
To explain to a person who is a kmn and a "cauterizer" that a simple survey colposcopy is a prelude for a colposcopic examination, that without a sample with a solution acetic acid nothing is visible at all - neither the norm, nor the pathology, I did not succeed. He put up with my "whim", because I worked as an oncogynecologist, but nothing more
Returning to colposcopic terminology, we must clearly understand that there are normal colposcopic pictures. In such cases, the conclusion "you have erosion" should turn into "you are healthy"

In the classification of Rio de Janeiro, variants of transformation zones are separately prescribed. This is done in order to more accurately determine which colposcopy is satisfactory and which
The transformation zone starts from the cylindrical epithelium and ends at the level of the most distant gland (open or closed)
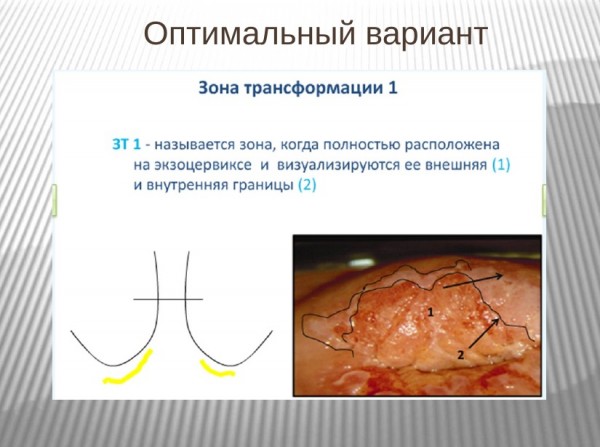
Thus, ectopic columnar epithelium almost always suggests a type 1 transformation zone - the most calm and prosperous option. ![]()
Transformation zone type 2 is almost always an unsatisfactory colposcopy. The displacement of the columnar epithelium into the cervical canal does not allow us to confidently assess the entire transformation zone. It is quite possible that the most "ugly" section hid in the canal. Please note that the "points" and "holes" are clearly visible in the photograph - closed and open ducts of the glands 
The transformation zone is not visible at all, colposcopy is categorically unsatisfactory. I will obsessively repeat: "unsatisfactory" is uninformative, not bad. Such patients need to carry out regular and high-quality cytological control, paying maximum attention to the sampling of material from the cervical canal - cancer will begin exactly there, when we see changes, it will be unforgivably late.
all colpophotographs by A.S.Bushkova
A gynecological Pap smear is a simple, painless test used to diagnose endometrial and cervical cancer. It is based on the work of George Papanicolaou, who discovered that malignant tumor cells slough off into vaginal secretions.
Research principle
Every year, 500 thousand women fall ill with cervical cancer in the world. Over the past 30 years, the incidence has decreased by more than 2 times. This is largely due to wide application screening cytology.
Basis for early detection of cervical cancer in large groups population over the past 60 years - Pap smear.
What is a Pap test (also known as Pap smear)?
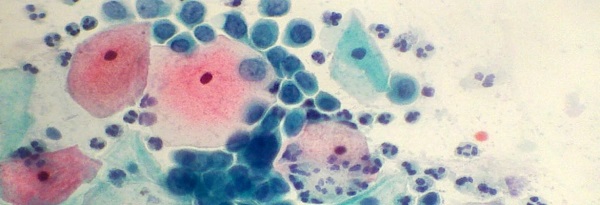
This is an exfoliative cytological procedure with staining of the obtained material. In other words, a Pap smear is a scraping of the tissues of the surface layer of the cervix and examination of the resulting cells under a microscope after treatment with special dyes. The method is also used to detect cancer Bladder, stomach and lungs. Any body secretions (urine, feces, sputum, prostate secretion), as well as biopsy material, are suitable for it.
However, most often the Pap smear is used to diagnose the initial stages. The material is taken from the transition zone of the cervix, where the columnar epithelium of the cervical canal borders on the squamous stratified epithelium lying on the vaginal part of the cervix. The resulting sample is placed on a glass slide, stained, and examined under a microscope to detect abnormal or malignant cells.
What does it show?
It detects precancerous and malignant changes (cancer) of the cervix. After a few minutes, the analysis can reveal or her neck at a stage when the tumor is not accompanied by external changes and damage to surrounding tissues. At this time, the malignant neoplasm is successfully cured. Therefore, a Pap test is recommended for all women over the age of 21 on a regular basis.
The liquid-based cytology Pap test aids in the detection of . At the same time, an additional study is carried out to identify the DNA of the virus. This pathogen is a major risk factor for cervical cancer. When using the method of liquid cytology, the material is placed not on a glass slide, but in a test tube with a liquid preservative.
A smear for the human papillomavirus is prescribed in case of doubt in the results of a cytological examination. Both traditional analysis and liquid cytology have equal diagnostic efficiency. Both of these methods can be used in practice.
HPV testing is not performed in women under the age of 30 due to the high prevalence of this infection in this age group. In addition, often the infection is transient, that is, it can disappear.
Although the interpretation of the results largely depends on the qualifications and experience of the doctor, there are objective ways to improve the accuracy of the diagnosis. Thus, special computer programs. Some clinics retest some swabs for quality control.
Much depends on the correct preparation of the woman for the study.
Test preparation
The analysis is carried out during scheduled inspection at the gynecologist. The doctor should be informed about the contraceptives and other hormonal drugs taken.
Special preparation for the Pap test:
- refrain from vaginal intercourse for 48 hours before the study;
- at the same time, do not use vaginal tampons, do not douche, do not use drugs or contraceptives inserted into the vagina;
- it is desirable to pre-cure, if any.
Pap test, in other words Pap smear
On what day of the cycle should I take the test?
There are no special restrictions. The only condition is the absence of menstrual or other uterine bleeding. However, the analysis can be taken even during menstruation, but its accuracy is reduced.
If a woman has bleeding or cervicitis (inflammation of the cervix), this is not a contraindication for the study. These symptoms may be caused by precancer or malignancy, which can be detected during screening.
Indications
For timely diagnosis malignant tumors requires a simple method that has no contraindications. Pap test of the cervix is a screening test that allows you to regularly examine most women.
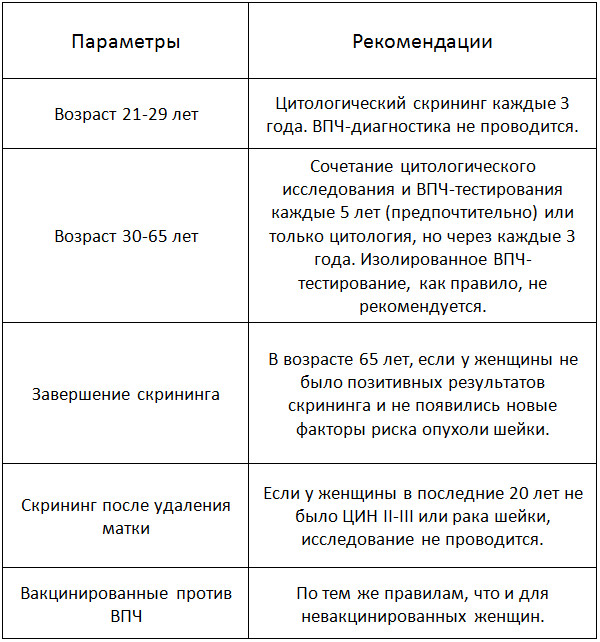
Table. When is the best time to do a Pap test?
Some women have a higher than average risk of developing cancer. They may need more frequent testing.
At-risk groups:
- women infected with HPV or HIV;
- survivors and venereal diseases;
- immunocompromised patients;
- early onset of sexual life;
- multiple sexual partners;
- had;
- smoking or drug use.
A Pap test during pregnancy is mandatory to exclude infections and precancerous diseases. No danger to future mother And he's not carrying a baby.
How is it carried out?
For the analysis are used:
- gynecological chair and lamp;
- metal or plastic vaginal dilator;
- examination gloves;
- cervical spatula and a special brush;
- test tube or glass slide.
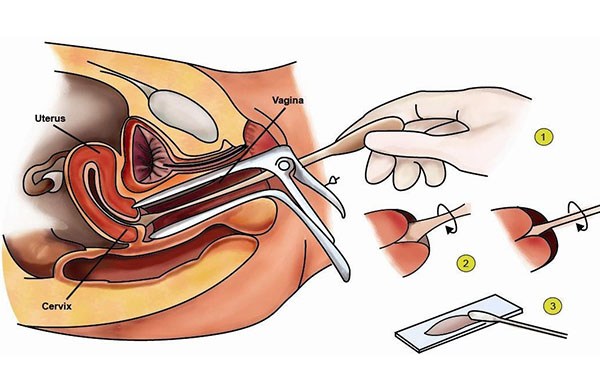
How is a Pap smear performed?
The patient is located on the gynecological chair. Her coccyx should be on the edge of the chair to ensure a good view when the dilator is inserted.
A dilator is placed in the vagina. It is recommended to warm it up first. warm water for the comfort of a woman. In some clinics, if necessary, a small amount of a special lubricant is used to facilitate the insertion of the dilator.
The surface of the cervix should be completely open and well examined by a doctor. It is necessary to visualize the squamous epithelium, the transition zone and the external pharynx. The transition zone is the area where the squamous epithelium is transformed into glandular. HPV affects this area. Therefore, the selection of cells is carried out in this zone. In addition, material is taken from the surface of the neck and from the area of the external pharynx.
If necessary, the neck is cleaned of secretions with a soft swab. Taking the material is taken with a spatula or a special brush, turning them around its axis.
Depending on the equipment used, the resulting material is either placed in a special solution, which is in a test tube, or on a glass slide, which is then applied with a fixative and placed in an alcohol solution.
The study is completed within a few minutes. It is painless. After the analysis, within 5 days it is better to refuse sexual intercourse, the use of tampons and douching.
Can I take a bath after a Pap test?
Complications and restrictions
Adverse effects after a Pap smear are very rare. A woman should be warned of the possibility of weak spotting. This is fine. Another complication is the addition of an infection. However, its probability is very low, since the procedure does not damage the blood vessels and sterile instruments are used.
Although the Pap smear is one of the best screening methods, it has its limitations. The sensitivity of a single Pap test in detecting cervical dysplasia averages 58%. This means that the existing disease will be found only in half of the women who actually have it. Approximately 30% of women with newly diagnosed cervical cancer had negative result analysis.
Higher sensitivity has HPV testing. In the group of women over 30 years old, it allows diagnosing dysplasia in 95% of cases. However, in younger women, such an analysis becomes less informative.
results

If the interpretation of the results of the Pap test showed the presence of abnormal cells, the patient is assigned a colposcopy. This study helps to detect precancerous and malignant changes using a biopsy - taking a piece of tissue for microscopic analysis. If a precancerous disease is detected and treated in time, this will save the patient from cancer.
How many days is the analysis done?
The result is ready in 1-3 days, when using automatic analyzing systems, the time to obtain the result is reduced. In some public clinics, the waiting time for the result increases to 1-2 weeks.
There are 5 classes of smears:
- Normal, no abnormal cells.
- Cellular change associated with inflammatory disease of the vagina or cervix.
- Single cells with altered cytoplasm or nucleus.
- individual malignant cells.
- Atypical cells in large numbers.
The Bethesda classification system is also used. In accordance with it, a low and a high degree of change are distinguished. Low includes koilocytosis and CIN grade I. High includes CIN II, III and carcinoma in situ. This corresponds to grades 3-5 smears.
As a result of the analysis, you can see the following designations:
- NILM - the norm, corresponds to class 1 smear.
- ASCUS - atypical cells of uncertain significance. They can be caused by dysplasia, HPV infection, chlamydia, mucosal atrophy during menopause. HPV testing and a repeat Pap test in a year are required.
- ASC-H is an atypical squamous epithelium that occurs in CIN grade II-III or early cancer. The tumor occurs in 1% of women with this result. An extended colposcopy is scheduled.
- LSIL - a small number of altered cells, indicates mild dysplasia or HPV infection. HPV testing is necessary, and if a virus is detected, a colposcopy. A repeat Pap smear is performed after one year.
- HSIL - pronounced changes corresponding to CIN II-III degree or cancer in situ. Without treatment within 5 years, cancer will occur in 7% of these patients. A colposcopy with biopsy or diagnostic excision is prescribed.
- AGC - altered glandular cells that occur with dysplasia and cancer of the cervix and body of the uterus. An HPV study, colposcopy, curettage of the cervical canal are prescribed. If a woman is over 35 and has irregular uterine bleeding, a separate diagnostic curettage is carried out.
- AIS is carcinoma in situ, an early stage of a malignant tumor. Shown colposcopy, diagnostic excision, separate diagnostic curettage.
- High-grade SIL - squamous cell carcinoma.
- Adenocarcinoma is a tumor that develops from the glandular epithelium of the cervical canal.
Benign glandular changes are considered a normal variant in women with a normal menstrual cycle. If there is irregular bleeding, or the patient is in menopause, diagnostic curettage of the endometrium is indicated to rule out uterine cancer.
With any variant of the Pap test, a consultation with a gynecologist is necessary.
Preparation:
Preparation conditions are determined by the attending physician.
In women of reproductive age, smears should be taken no earlier than on the 5th day of the menstrual cycle and no later than 5 days before the expected start of menstruation. You should not take cell material for research within 24 hours after sexual intercourse, sanitation of the vagina, introduction of medications into the vagina.
Indications:
Cytological smears should be taken from all women over 18 years of age, regardless of clinical data, once a year. In the presence of clinically pronounced pathological changes in the cervix, the cellular material is taken aimingly. The frequency of cytological examination is determined by a gynecologist (at least 2 times a year).
The cytological method of research occupies one of the important places in the diagnosis of diseases of the cervix. Due to its high accuracy, it is one of the leading research methods in the diagnosis of background, precancerous and cancerous processes of various localization.
Advantages of the method:
- painlessness and safety of obtaining cellular material;
- the possibility of studying the pathological focus in dynamics;
- the possibility of diagnosing a malignant neoplasm in the initial stage of development;
- small financial costs.
Disadvantages of the method:
- the impossibility of establishing signs of infiltrative growth (cell, not tissue material is examined).
The specificity of this screening method is 69%. The rate of false-negative smears ranges from 5 to 40%. Inadequate sampling from the endocervix is the most important factor in causing false negative results.
The effectiveness of the cytological research method largely depends on the preanalytical stage: how correctly the cellular material is taken and the smears are prepared.
It should be remembered that the cytological method of research, like any other laboratory research method, does not always provide comprehensive information for making a diagnosis. Only a clinician has the right to make a final diagnosis (based on the study of anamnesis, observation of clinical manifestations and data from the histological method of examination).
The result is presented as:
- descriptions of cellular composition and conclusions
Result interpretation
Possibilities of cytological diagnosis of certain diseases of the cervix and options for interpreting the results of a cytological study:
Endocervix. Normally, with correctly obtained cellular material from the transformation zone (ZT) - the junction zone of the squamous and columnar epithelium - cells of the squamous and columnar epithelium are present in the smear without changes. Cytological conclusion: cells of squamous and cylindrical epithelium without features were found in the obtained material. The presence of a small number of metaplastic epithelial cells is an indication that the material was obtained from ST. In the absence of the above description, the swab was not taken from ST and the patient cannot be said to be at no risk of cervical cancer. Such swabs are commonly seen in postmenopausal women and patients who have undergone cervical treatment that has moved the borderline into the cervical canal. Depending on the patient's history, this may be a reason for re-sampling the material.
Ectocervix. In reproductive age, the normal cellular composition of imprints from the vaginal part of the cervix is represented by squamous epithelial cells, predominantly of a superficial or intermediate type. The wording “in the obtained material cells of the squamous epithelium of the surface layers without features are noted” indicates that the obtained biological material consists of cells of the squamous epithelium of the surface and intermediate layers in various combinations in accordance with the phase of the cycle. At the beginning of postmenopause (normal), cells of the squamous epithelium of the intermediate layer are noted in the smear. In some women, during the whole subsequent life, an intermediate type of smear (squamous epithelial cells of the intermediate layer) is observed, sometimes with the presence of cells of the surface layer, which is apparently associated with adrenal function, an active sexual life. The presence in the preparation of cells of the squamous epithelium of the surface layer (estrogenic type of smear) in the first 5 years of menopause should be alarming in relation to neoplasms of the ovaries, uterine fibroids. Postmenopause is characterized by the presence of cells of the basal-parabasal layer (i.e., deep layers).
Erosion (ectopia) of the cervix.
The concept of cervical erosion (true erosion) involves a defect in the cervical mucosa caused by various diseases (syphilis, traumatic injuries, the effects of radiation therapy, cervical cancer, etc.). The term cervical ectopia (pseudo-erosion) means the displacement of a high cylindrical epithelium on the vaginal part of the cervix. Provided that there is a clinical diagnosis of "erosion/ectopia of the cervix" in the direction and the correct sampling of biomaterial from the ectocervix, the cellular material is represented by squamous epithelial cells of all layers in various combinations, clusters of cylindrical epithelium cells, elements of inflammation /
With healing endocervicosis, a large number of cells of metaplastic epithelium are found in smears (metaplasia is the replacement of one type of epithelium with another). Metaplastic epithelium is a target for human papillomavirus exposure - an area for the development of precancerous conditions. The presence in smears from the cervix of a small number of cells of metaplastic epithelium is an indicator of a normal physiological process.
Leukoplakia of the cervix. With the cytological method for diagnosing simple leukoplakia (a benign lesion of the cervix, an underlying disease), hyperkeratosis is detected, i.e., in the material obtained from the ectocervix, layers (clusters) of squamous epithelium scales were found (there is no nucleus in the cytoplasm of the cell), separately lying squamous epithelium scales, dyskerocytes . In the absence of a clinical diagnosis of cervical leukoplakia, depending on the available material, the cytologist gives a descriptive answer, possibly with a recommendation to exclude cervical leukoplakia. Single scales of squamous epithelium have no diagnostic value. Leukoplakia with atypia by the cytological method of research is not always possible to identify, which is explained by the presence of squamous epithelium scales on the surface of the stratified squamous epithelium, which prevent the receipt of cellular elements. It is necessary to conduct a morphological study of the biopsy of the cervix.
Dysplasia of the cervix.
Dysplastic changes occur in the stratified squamous epithelium of both exocervix and endocervix. As a rule, changes begin at the junction of the squamous and columnar epithelium. Dysplasia can simultaneously develop in several areas of the cervix and cervical canal, often changes are expressed to varying degrees.
Dysplasia-I (mild dysplasia, CINI) is one of the least reproducible cytological diagnoses. Dysplasia-I is often difficult to differentiate from reactive epithelium. It is not always possible to make a differential diagnosis between dysplasia III (severe dysplasia, CIN-III) and intraepithelial cancer by cytological examination.
If there are cells with signs of malignancy in the obtained material, the cytologist gives a conclusion on the cytogram of the malignant neoplasm and, if possible, specifies the form of cancer.
Inflammatory processes of the cervix . Inflammation - a cellular reaction (in the focus) - is represented by a degeneratively altered epithelium, proliferative changes of a reparative, protective nature, and inflammatory atypia. In an acute nonspecific inflammatory process, a pronounced leukocyte infiltration (many neutrophilic leukocytes), incomplete phagocytosis is noted in the smear. The composition of the cell population of the epithelium may change. In subacute and chronic inflammation, eosinophils, lymphocytes, macrophages / cells such as foreign bodies (multinuclear macrophages) join. Acute inflammatory processes are more often observed in the age group of 20-24 years, chronic processes and their consequences occur in women aged 25-34.
Infectious lesions of the cervix . Cytological features of smears for infectious lesions of the cervix depend on the pathogen and the duration of the inflammatory process.
Mycoplasmas, ureaplasmas and corynobacteria as the cause of inflammation is observed in a group of young women (up to 20 years). In the age group over 30 years, anaerobic microorganisms occupy the first place among the causative agents of inflammatory processes in the genitals. Mixed infection increases the pathogenicity of each of the pathogens. In such cases, inflammation causes a pronounced tissue reaction, accompanied by damage to the epithelium, destruction and dysplasia. This leads to the development of not only colpitis, endocervicitis, but can play a significant role in the formation of cervical ectopia. Incomplete phagocytosis is noted (phagocytic activity of leukocytes is suppressed). The cytological conclusion indicates the type of flora with a recommendation to exclude a certain type of infection.
Bacterial vaginosis (BV) - (clinical diagnosis). In cytological preparations, BV is represented by key cells. If the key cells are not found, and the flora is cocco-bacillary, it is recommended to exclude the presence of gardnerella (ureaplasma) in the cytological response; in the presence of mobiluncus bacilli, a recurrence of the pathological process after the treatment is possible.
Genital herpes- Herpes simplex virus has a high tropism for epithelial and nerve cells. Relapses are mainly due to the persistence of infection in the nerve ganglion. Cytological examination of the obtained material may show changes in squamous epithelial cells specific for their defeat by this type of viral infection: multinucleated cells of the "mulberry" type. Form of cytological response: signs of a viral infection were found in the material obtained. It is recommended to exclude the herpes simplex virus.
Papillomavirus infection of the genitals. The human papillomavirus is able to persist for a long time in the basal layer of the squamous epithelium, which causes a high frequency of recurrence of the process. The frequency of coincidence of cytological and histological diagnoses in condyloma was 42%: CIN-I - 56%, CIN III 74%. False-negative cytological responses are explained by the consequence of incorrect material sampling - 90%, incorrect interpretation - 10%.
In addition, underdiagnosis in cervical smears may be due to the presence of koilocytes in the deeper layers of the squamous epithelium or the presence of a large overlap of elements of inflammation and flora. Cytological conclusion: the obtained material showed signs of a viral infection. It is recommended to rule out the human papillomavirus. Indirect changes characteristic of a viral infection: an increase in the size of the nucleus, nonspecific multinucleation. The form of the cytological response: the obtained material shows indirect signs of a viral infection. It is recommended to exclude the herpes simplex virus, human papillomavirus.
Trichomoniasis. An inflammatory reaction develops in the presence of a large number of protozoa. Proper preparation of the patient is essential for the quality of the study. Termination of the use of trichomonocidal drugs for 5-7 days before taking the material. The cytological preparation contains signs of an acute / chronic inflammatory process, mixed flora, Trichomonas
Chlamydial infection. Chlamydia are tropic to columnar epithelium. Often found in women with cervical ectopia. In pregnant women and menopausal women, signs of infection may be observed in the squamous epithelium. They can also be found in macrophages. Cytologically, the presence of intracellular specific inclusions is determined, which are more often detected with a fresh or untreated infection. Cytological forms of response: cells with cytoplasmic inclusions morphologically similar to chlamydial infection were found. It is recommended to exclude the presence of chlamydial infection.
Papanicolaou test- analysis to detect precancerous and. This study has many synonyms - Pap test, Pap smear, cytological smear. The Papanicolaou test was named after the author, physician and founder of medical cytology - Georgios Papanicolaou.
Pap test is done during gynecological examination all women over 21. Using a spatula and endobrush, the doctor takes cell samples from the surface of the cervix and cervical canal. The resulting material is applied to a glass slide, fixed with alcohol and sent to the laboratory. Laboratory assistants stain the smear according to the method developed by Papanicolaou, study the structure of cells, drawing Special attention on the typicality, size, degree of maturation, size and structure of the nuclei, their relationship with the cytoplasm.
Research value. Papanicolaou test can detect dysplasia and cervical cancer on initial stages until the disease responds well to treatment. Thanks to the massive Pap test over the past 40 years, it has been possible to reduce the incidence of cervical cancer by 60-70%, and the death rate from this type of cancer has decreased by 4 times.
Cervix
Cervix- the lower part of the uterus, which opens at one end into the uterine cavity, and at the other into the vagina. It is a tube 3-4 cm long, consisting of smooth muscles and connective tissue fibers.Secreted in the cervix two parts:
- exocervix or vaginal part - the lower segment of the cervix, which is in contact with the vagina;
- endocervix or cervical canal, which is also called cervical canal- this is a through hole that passes through the body.
- internal os opens into the uterine cavity;
- external pharynx opens into the vagina.
- Epithelium- cells located on the surface of the mucosa;
- basement membrane- a thin plate of connective tissue, which is the basis of the mucous membrane.
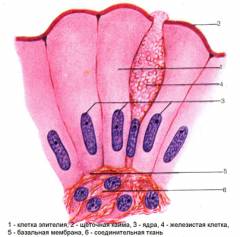
- Basal- 1 layer of small undifferentiated(immature) cells lying on the basement membrane;
- Parabasal- 2-3 rows of cells in which the first signs of maturation appear;
- Intermediate- 6-12 rows of moderately differentiated cells;
- Surface- 3-18 rads of cells lying on the surface. They are not prone to keratinization and are constantly sloughing off, being replaced by new ones rising from the basal layer.
Indications for a pap test
A smear for cytology must be taken by all women over 21 years old, regardless of the intensity of sexual activity and the number of partners.- First smear at the age of 21 or 3 years after the onset of sexual activity.
- 1 time per year during a routine gynecological examination for all women from 21 to 64 years of age.
- 1 time in 2-3 years handed over by women under 65 years of age, in whom 3 consecutive births in a smear did not reveal changes in the structure of epithelial cells of the cervix. After age 65, the test can be done less frequently.
- 1 time in 6 months- women of the following categories:
- women with;
- patients with cancer in the family;
- women with, or other diseases of the cervix;
- signs of human infection are found;
- to control the treatment of the cervix.
Pap test methodology
When is the best time to do a Pap test?
 To obtain the material, scraping of the epithelium is carried out from the surface of the vaginal part of the cervix and from the cervical canal. best time the period between the 10th and 20th day of the menstrual cycle is considered. It is not advisable to take the material later than 5 days before the expected menstruation and during menstrual bleeding. During this period, mucosal physiological changes, which can be mistaken for signs of the disease.
To obtain the material, scraping of the epithelium is carried out from the surface of the vaginal part of the cervix and from the cervical canal. best time the period between the 10th and 20th day of the menstrual cycle is considered. It is not advisable to take the material later than 5 days before the expected menstruation and during menstrual bleeding. During this period, mucosal physiological changes, which can be mistaken for signs of the disease. To take the material, the gynecologist uses disposable instruments:
- Eira spatula - for taking a smear from the vaginal part. Its narrow end is inserted into the external pharynx, and the short and wide end is scraped from the vaginal part;
- curettes - Volkmann's spoons - for taking scrapings from suspicious areas;
- endobranch brush - for scraping the epithelium inside the cervical canal.
How is a Pap test performed?
 The material for test dads is taken before an extended and bimanual examination - palpation (palpation) of the uterus and its appendages. This avoids contamination of the material with talc.
The material for test dads is taken before an extended and bimanual examination - palpation (palpation) of the uterus and its appendages. This avoids contamination of the material with talc. - The woman is placed in an examination chair. The doctor examines the cervix using gynecological mirrors.
- Cleansing the cervix from mucus. carried out if a large amount of secretion prevents scraping.
- Material samples are taken from several sites:
- In the area of the external pharynx, where precancerous and cancer cells;
- On visible foci of pathological changes, if any;
- WITH inner surface cervical canal. This procedure is carried out after the removal of the mucous plug.
- The resulting material from each area is applied in an even layer on separate glass slides, touching all surfaces of the brush. Smears are fixed with fixative solutions containing alcohol. This is necessary to avoid their drying out and deformation.
- Glasses are marked (signed), a direction is attached to them containing brief information about the patient.
- In the laboratory, the samples are stained to better see the structural features of the cells. Conduct microscopy of samples. It evaluates:
- cell type;
- size;
- the presence of inclusions in the cells;
- their degree of maturity;
- the number and structural features of cell nuclei;
- the state of the cytoplasm;
- ratio of cytoplasm to nucleus.
- The result of the pap test is usually sent to the attending physician in 1-2 weeks. In private laboratories, the waiting time for a Pap test result is 1-3 days.
Methodology for conducting a pap test based on liquid cytology:
- The brush makes 5 rotational movements clockwise in the region of the external pharynx. Thus, it is possible to make a scraping from the entire transformation zone. With another brush, material is collected from the walls of the cervical canal.
- The brush tips are removed and placed in separate vials with preservative liquid.
- The tube is shaken, as a result of which the cells pass into the liquid.
- In the laboratory, the liquid is centrifuged. Preparations are prepared from the resulting cell sediment, stained and examined under a microscope.
How to prepare for the pap test?
The Pap test requires some preparation. 1-2 days before visiting the gynecologist must refrain from:- sexual contacts;
- douching;
- vaginal preparations - creams, suppositories, spermicidal gels;
- washing inside the vagina and vaginal shower;
- hot bath.
Pap test is not performed:
- during menstruation;
- during inflammatory diseases cervix.
What are the results of the pap test?
 Several systems are used to evaluate the result of the Pap test:
Several systems are used to evaluate the result of the Pap test: - System developed by Papanicolaou in 1954, which classifies changes into 5 classes:
- Class I - normal cytological picture, unchanged cells;
- Class II - minor cell changes associated with inflammatory process in the vagina and cervix;
- Class III - suspicion of malignancy, single cells with an anomaly in the structure of the nucleus and cytoplasm;
- Class IV - single cells with obvious malignant changes;
- V class - malignant tumor, a large number of cancer cells.
- The system proposed National Institute US Cancer Research in 1988. It was revised in 2001 and is now widely used in all countries.
- NILM- absence of signs of malignancy and epithelial damage;
- ASCUS- atypical squamous epithelial cells of an indeterminate nature. May indicate inflammation, but neoplasia (a precancerous condition that can transform into a malignant tumor) is not ruled out;
- ASC-H- atypical squamous epithelial cells. It is impossible to exclude the defeat of the squamous epithelium of a high degree of severity - HSIL;
- LSIL- damage to the squamous epithelium of a low degree of severity. Indicate weak dysplasia or damage by human papillomavirus;
- HSIL- damage to the squamous epithelium of a high degree of severity. May indicate moderate or high grade dysplasia, rarely carcinoma in situ;
- AGC- atypical glandular cells, atypical cells of the glandular epithelium of the cervical canal;
- AGUS- abnormal glandular cells of uncertain significance;
- Carcinomain situ- the beginning of the formation of a cancerous tumor, the cells do not go beyond the basement membrane;
- High Grade SIL- a large number of malignant cells, which indicates cancer based on squamous epithelium;
- Adenocarcinoma- cancer based on columnar epithelium.
Pap test result options
I. Normal result. If the terms are indicated in the conclusion: NILM(negative for intraepithelial lesion or malignancy), negative result, class I - this means that the woman is healthy and no altered cells have been detected. There are no serious violations in the cervix:,. Signs indicating and are allowed.The material may include:
- unchanged squamous epithelial cells;
- cells of cylindrical and metaplastic epithelium;
- leukocytes in a small amount;
- bacteria in small quantities.
1.ASC-US- atypical squamous cells of uncertain significance. Their appearance can be caused by:
- dysplasia;
- human papillomavirus (HPV) infection;
- and other sexually transmitted infections;
- mucosal atrophy during menopause.
- undergo an analysis for the detection of papillomavirus (an analysis for HPV);
- retake the pap test after 1 year.
Causes:
- dysplasia;
- papillomavirus infection.
- test for HPV
- colposcopy, if HPV is detected,
- conduct PAP in a year.
Causes:
- precancerous changes - dysplasia of 2-3 degrees;
- rarely, the initial form of cancer.
- mandatory extended colposcopy.
Causes:
- high-grade dysplasia;
- rarely, cervical cancer.
- if the examination reveals first-degree dysplasia, then a pap test and colposcopy are performed every 6 months for 2 years;
- women over 25 years of age immediately undergo a diagnostic excision - removal of a section of the mucous membrane of the cervix.
Causes:
- dysplasia of 1-3 degrees;
- cervical cancer;
- endometrial cancer.
- colposcopy;
- collection of material by scraping the mucous membrane of the cervical canal;
- analysis for HPV;
- women over 35 years of age with irregular spotting - collection of material by scraping the endometrium.
Causes:
- high-grade dysplasia;
- cervical cancer
- colposcopy;
- diagnostic curettage of the cervical canal;
- scraping the endometrium for diagnostic testing;
- diagnostic excision - removal of a section of the mucosa.
Causes:
- endometrial hyperplasia - precancerous changes in the endometrium;
- endometrial cancer;
- in the absence of symptoms (irregular menstruation, bloody issues from the vagina, not related to menstrual bleeding) in women who have not reached menopause, benign glandular changes are considered a variant of the norm.
- diagnostic curettage of the endometrium in women who have reached menopause or who have symptoms of endometrial hyperplasia;
- there is no need for further evaluation in premenopausal women who are asymptomatic.
What to do with a “bad” pap test result?
Depending on the age of the woman and the nature of the changes, the doctor may choose one of the options.
- Repeat pap test in 3 months. If it turns out to be negative (without pathological changes), then repeated Pap tests after 6 months, 1 year, 2 years. At a positive result- Perform a colposcopy.
- Perform a colposcopy. If an extended colposcopy does not reveal any changes, then repeat the Pap test after 6 or 12 months. If colposcopy has revealed foci of changes, then they are carried out. At dubious result colposcopy is carried out with anti-inflammatory or estrogenic hormonal treatment followed by another colposcopy.
- Get tested for human papillomavirus (HPV). If oncogenic types of the virus are detected, colposcopy is performed. In the absence of such, a repeated Pap test after 6 months.
Incorrect pap test result
 The sensitivity of the pap test ranges from 70-95%. The cause of errors may be incorrect collection and fixation of the material, insufficient qualifications of the laboratory assistant, or processes occurring in the uterus.
The sensitivity of the pap test ranges from 70-95%. The cause of errors may be incorrect collection and fixation of the material, insufficient qualifications of the laboratory assistant, or processes occurring in the uterus. - False positive Pap test result- analysis indicates that there is dysplasia, although the woman is healthy. The cause may be transferred inflammatory and infectious diseases genital organs, erosion in the stage of healing (regeneration), hormonal disorders. These processes give rise to cells that may have unusual shape. To exclude errors, a colposcopy or a repeated pap test is performed.
- False negative result pap test- there is a disease, and the test results are within the normal range. This is possible if the doctor did the scraping incorrectly and epithelial cells from the foci of the disease did not get into the smear, or atypical cells were not found in the laboratory. This option is possible, but do not be afraid. If visible changes appear on the cervix, the doctor will prescribe a colposcopy and a biopsy. Even if the foci of dysplasia go unnoticed, it will take 2-20 years before they turn into a malignant tumor, and the pathology will be detected during the next PAP test.
The Pap test is a diagnostic procedure designed to detect precancerous and cancerous diseases of the cervix. Also during the study, signs of inflammation, or atrophy of the cervix, may be detected.
- Infections.for bacterial and viral infections indicate:
- squamous cells of uncertain significance ASC US;
- the presence of bacteria in the material;
- changes in the structure of cells caused by the presence of a virus.
- Inflammatory atypia - the appearance of cells with minor deviations (thin membranes, enlarged nuclei), which is caused by inflammation;
- Squamous metaplasia - replacement of the cylindrical epithelium with stratified squamous;
- Hyperkeratosis - keratinization of stratified squamous epithelium;
- Parakeratosis - increased keratinization or complete absence the process of keratinization;
- Reserve cell hyperplasia - an increase in the volume of reserve cells.
- papillomavirus infection. The appearance of most atypical cells is associated with the human papillomavirus. Its presence in the body is indicated by:
- Atypical squamous cells of uncertain significance ASC US;
- Low-grade squamous intraepithelial lesions LSIL - disorders in squamous cells;
- Atypical squamous cells that do not rule out HSIL - ASC-H;
- Neoplasia or dysplasia of the cervix abbreviated CIN (cervical intraepithelial neoplasia) is pathological changes cervical mucosa that occurs when infected with the human papillomavirus. The virus damages the genetic material in the cell nuclei, which causes the appearance of abnormal cells and increases the risk of developing malignant cells. Mild dysplasias are able to regress (cure) on their own, but about 20% eventually progress to a more severe stage.
- Carcinoma in situ(in situ) - cervical cancer on early stage development. Cancer is a collection of epithelial cells. It does not penetrate into the basement membrane and underlying tissues, does not form metastases. It responds well to treatment. About the development of the oncological process they say:
- High grade squamous intraepithelial lesions HSIL;
- Cells characteristic of cervical cancer - carcinoma in situ .
- Adenocarcinoma - cervical cancer, which originates from the cylindrical epithelium - cells of the cervical canal. Adenocarcinoma is indicated by:
- Atypical glandular cells AGC;
- Adenocarcinoma cells in situ AIS.
- Squamous cell carcinoma - a type of cervical cancer that is formed on the basis of squamous epithelial cells. The analysis reveals:
- Carcinoma in situ - AIS;
- Atypical squamous cells that do not rule out HSIL - ASC-H;
- High grade squamous intraepithelial lesions - HSIL;
- Atypical glandular cells - AGC.
- Cervical cancer or endometrial cancer- a malignant tumor of the inner lining of the uterus. Cancer is indicated by:
- Atypical glandular cells AGC;
- Atypical squamous cells that do not rule out HSIL - ASC-H;
- High grade squamous intraepithelial lesions - HSIL;
- Cells characteristic of cervical cancer - AIS.
- Benign glandular changes- endometriosis. About this disease they say:
- Benign endometrial cells;
- Endometrial stromal cells;
- Histiocytes are connective tissue cells.
What to do after pap test
During the procedure for taking material for a Pap test, the doctor scrapes off the top layer of the mucosa, after which a small abrasion forms on the cervix. For 3-5 days, scanty bloody or dark brown discharge. This condition does not require treatment and the use of any medication.To prevent infection of lesions on the cervix, it is recommended to refrain from:
- sexual contacts;
- douching and vaginal douche;
- use of tampons.
