Anatomical and functional features of the hip joint. The structure of the hip joint
Parts of the thigh:
hip joint- the second largest load in the body after the knee. It consists of a head femur and acetabulum. The harmonious functioning of the parts of the joint allows us to make various movements. Damage to any component can adversely affect the ability to move and carry weight. If the hip joint is injured, it may be necessary one of three types of operations to replace it.
Femur
femur or top part legs. It is the largest bone in the body. The femur has several sections.
- 1A - Head of the femur- this is the top of the femur, which has a spherical shape. The head of the femur enters the acetabulum. The ligaments and muscles of the thigh make the joint strong and durable.
- 1B - Neck- Connects the femoral head to the pedicle
- 1C - Body of the bone- The lower long part of the bone that attaches to the knee joint. The muscles attach to two protrusions on the body of the bone, just below the head, where they connect to and move the joint.
- 1AA - Greater trochanter
- 1AA - Lesser trochanter
Taz
The pelvis or pelvic bone consists of three sections.
- Ilium
- Pubic bone
- Ischium
Before puberty Y-shaped cartilage separates these three bones.
At the age of 15-17 years, three of them grow together and form the acetabulum.
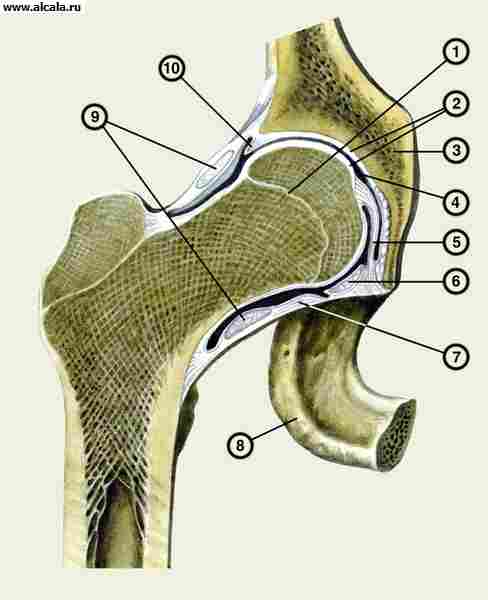
acetabulum
The acetabulum is a hemisphere, formed by bones pelvis and thigh, connecting with the head of the femur. It is fully formed at the age of 20 - 25 years.
3A - Articular capsule
The area inside the acetabulum filled with ligaments surrounding the joint.
3B - Synovium
A thin sheath inside the acetabulum that lubricates and nourishes the joint.
The synovial bursa is a small fluid-filled cavity located in the acetabulum, which is designed to prevent soft tissue from rubbing against the bone. The synovial bursa is located between the muscles, tendons and bones.
muscle groups
Gluteal muscles
This group includes three large muscles. They are attached to the back of the pelvis and enter the greater trochanter.
- Gluteus maximus muscle- the largest of the gluteal muscles and the strongest muscle in the body.
- Gluteus minimus- the smallest of the three, located in the middle.
- Gluteus medius located on outer surface pelvis.
Quadriceps femoris
Consists of four muscles that attach to the top of the lower leg.
- Vascularis lateralis muscle
- vastus medialis muscle of thigh
- Intermediate vastus femoris
- Rectus femoris
Iliopsoas muscle
The most important flexor muscle of the thigh. The group includes three muscles that emerge from the lower spine and pelvis and, passing along the surface of the joints, are attached to the lesser trochanter of the femur.
- psoas major
- Iliac muscle
- Small psoas muscle
Muscles of the back of the thigh
This group includes three muscles that attach to the lower part of the pelvis. They pass through the hip and knee joints and their main function is knee flexion and hip extension.
- Semitendinosus
- Biceps femoris
- semimembranosus muscle
Groin muscles - Adductor muscles
The groin muscle group departs from the pubis and is located on the inside of the thigh. They are fan-shaped. Thanks to the action of the inguinal muscles, the legs are reduced and bred, they also provide stability to the hip joint. There are five groin muscles.
- short adductor muscle
- adductor longus muscle
- Adductor major muscle
- thin muscle
- comb muscle
Bundles
Ligaments and muscles provide joint mobility.
- The iliofemoral ligament connects the pelvis to the femur at the front of the hip joint. The pubic-femoral ligament connects the prominence of the pubis to the femur.
- The ischiofemoral ligament connects the ischium and the femur at the bottom of the pelvis.
cartilage
The cartilages are located between the femur and the acetabulum. They are designed to protect the bones from friction and act as shock absorbers. Cartilage allows bones to move smoothly.
The acetabular lip is formed by a layer of cartilage around the outside of the acetabulum. It gives stability to the joint by increasing the depth of the acetabulum. One of the most common injuries of the hip joint is the rupture of the acetabular lip, in which case surgery is required to restore the cartilage.
Tendon of the ilio-tibial tract
The main tendon of the hip joint is called the iliotibial tract. Many muscles of the thigh and leg are attached to it. Wear on this tendon can cause hip pain.
Major nerves and blood vessels
- The sciatic nerve is located on the back of the thigh
- Femoral nerve - on the front of the thigh
- Femoral artery - originates in the pelvis and travels down the anterior pelvis.
Conclusion
Knowing the parts of the hip joint will come in handy during the hip replacement process. This will allow you to competently explain to the orthopedic surgeon or other specialist where your pain is. At first, you can carry this article with you to an appointment with a doctor or physiotherapist in order to be able to clearly explain the nature and symptoms of pain, then the doctor, in turn, will be able to make the correct diagnosis and competently plan the operation and recovery after it.
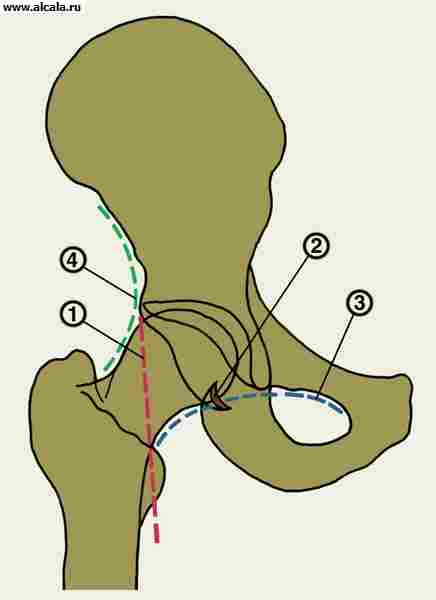
formed by the acetabulum of the pelvis and the head of the femur. A fibrocartilaginous lip runs along the edge of the acetabulum, due to which the congruence of the articular surfaces increases. T. s. strengthened by the intra-articular ligament of the head of the femur, as well as the transverse ligament of the acetabulum, covering the neck of the femur ( rice. 12 ). Outside, a powerful ilio-femoral, pubic-femoral and ischio-femoral ligaments are woven into the capsule. T. s. - a kind of spherical (so-called bowl-shaped) joint. Movements are possible in it: around the frontal axis (flexion and extension), around the sagittal axis (abduction and adduction), around the vertical axis (external and internal rotation).
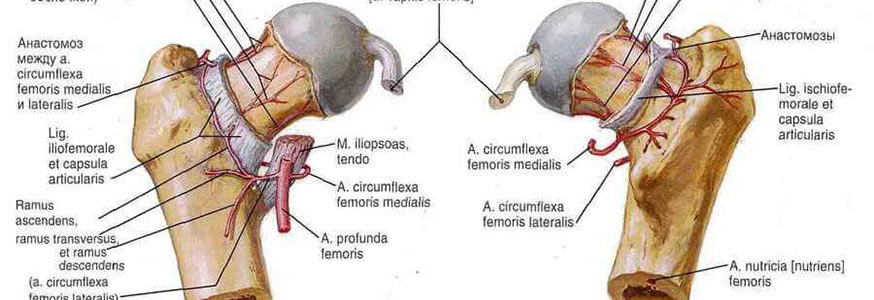
Blood supply of T. with. It is carried out through the arteries that envelop the femur, branches of the obturator and (inconsistently) branches of the superior perforating, gluteal and internal pudendal arteries. The outflow of blood occurs through the veins surrounding the femur, into the femoral vein and through the obturator veins into the iliac vein. Lymph drainage is carried out to the lymph nodes located around the external and internal iliac vessels. T. s. innervated by the femoral, obturator, sciatic, superior and inferior gluteal and pudendal nerves.
Research methods
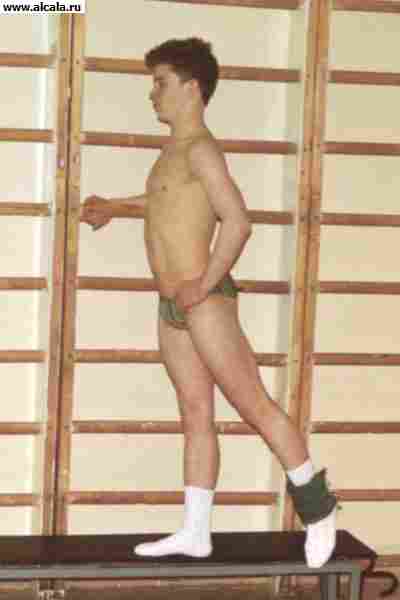
In an upright position, the patient's posture and gait, the severity of lumbar lordosis, the position of the limbs in relation to the pelvis and their length are checked. For example, with bilateral congenital hip dislocation, compensatory hyperlordosis may be observed. The presence of the Trendelenburg symptom is determined, which is noted in violation of the support of the lower limb and weakness of the gluteal muscles - in the standing position on the sore leg and bent at the hip and knee joints, the other pelvis leans into healthy side and lower is the gluteal fold.
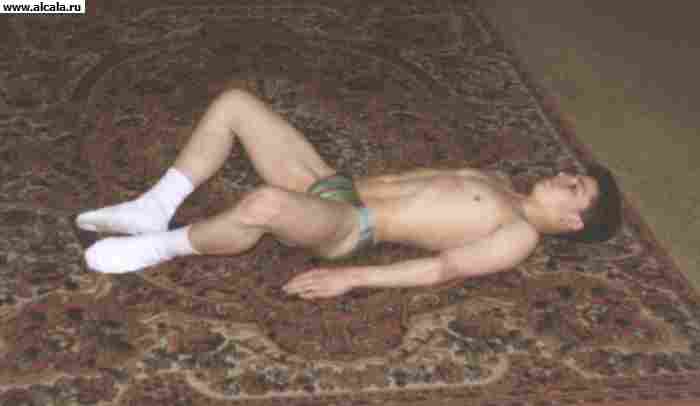
In the position of the patient on the back, the true position of the limb on the side of the lesion is established (in this case, it is necessary to eliminate hyperlordosis by bending the opposite limb in the hip and knee joints).
Check the volume of active and passive movements in the hip joints. Palpation determine the position of large skewers. Normally, they are located symmetrically at the level of the Roser-Nelaton line, which connects the superior anterior iliac spine and the ischial tuberosity. When the greater trochanter is displaced upward, the symmetry of the location of Shemaker's lines (drawn from the greater trochanter through the superior anterior iliac spine on each side to the intersection with the midline of the abdomen) and the isosceles triangle of Bryant are also violated. The construction of the latter is carried out as follows: on the line, which is a continuation of the axis of the thigh and passing along its outer surface through the greater trochanter, a perpendicular descends from the superior anterior iliac spine; the second line connects the superior anterior iliac spine and the apex of the greater trochanter. Normally, the distance from the top of the greater trochanter to the point of intersection of the perpendicular with the line, which is a continuation of the axis of the thigh, is equal to the length of the lowered perpendicular. In newborns, in addition to measuring length lower extremities and determining the range of motion in the hip joints, it is necessary to check the depth and symmetry of the inguinal, femoral and gluteal folds.
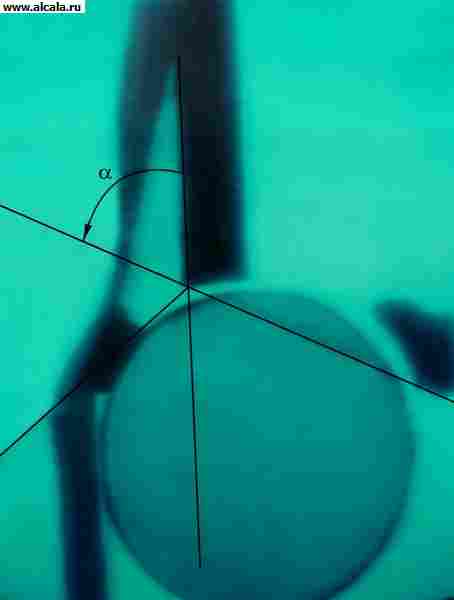
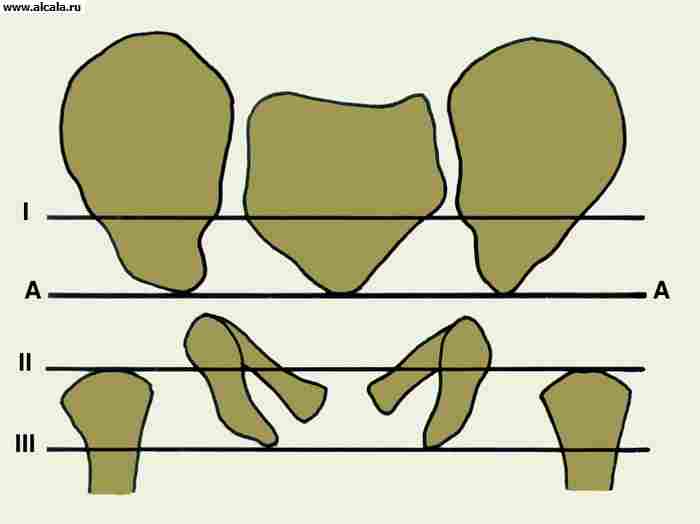
A significant role in the diagnosis of T.'s lesions. plays x-ray. Due to the fact that in the formation of T. s. involved bones that have irregular shape, the radiological projection image depends on the position of the patient (Fig. 3). The correctness of the laying is checked by the uniformity of the contours of the obturator foramen, the symmetry of the position of the sacral foramina, the uniformity of the radiographic gap of the sacroiliac joints and the size of the wings of the ilium. It is also necessary to take into account age features associated with structural transformations of the bones that form the hip joint.
The head of the femur in newborns is cartilaginous. The ossification nucleus appears in the first half of the year (by 4-6 months), increasing approximately 10 times by the age of 5-6. The growth of the femoral neck continues until the age of 18-20. In the first year of life, the cervical-diaphyseal angle averages 140°. The acetabulum is formed by the ilium, pubic and ischium bones and the Y-shaped cartilage connecting them. Complete synostosis of the bones in the region of the acetabulum occurs by the age of 14-17.
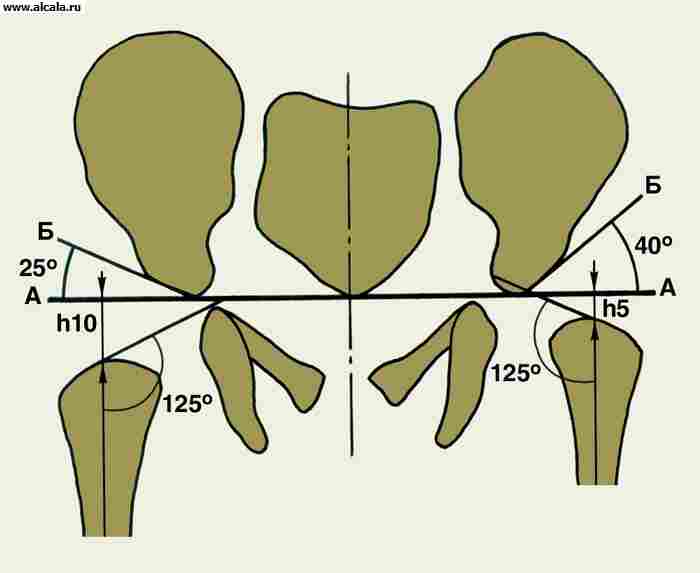
To determine the ratio of the elements of T. s. different reference points are used rice. 3, 4, 5 ). So, the inner wall (bottom) of the acetabulum and the wall that limits the cavity of the small pelvis in this area form a “tear figure”. The femoral heads are normally located at the same distance from the “tear figure”. Also symmetrically projected onto the lower inner quadrant of the femoral head is a “crescent figure” formed by a groove between the posterior part of the semilunar surface and the body of the ilium. A vertical line (Ombredand's line), lowered from the outer point of the upper edge of the acetabulum, passes outside the femoral head or through its outer segment. The arcuate line (Shenton's line) smoothly passes from the lower contour of the femoral neck to the upper edge of the obturator foramen. The angle formed by the horizontal line (Hilgenreiner line) drawn through the symmetrical sections of the Y-shaped cartilage on both sides and the line passing through the outer and inner points of the acetabular arch does not exceed 22-26° (Fig. 5). An increase in the angle indicates a sloping (underdevelopment) of the roof of the acetabulum. The displacement of the femoral head in relation to the listed landmarks indicates the presence of its subluxation or dislocation. Adults may normally have additional bone formations T. s. (Fig. 6).
Pathology
Malformations include T.'s dysplasia of page, inborn varus and valgus deformities of a neck of a femur.
Dysplasia The hip joint is manifested by underdevelopment of the acetabulum and proximal femur. Among other orthopedic diseases in newborns, it occupies one of the first places (from 5 to 16 per 1000 newborns). The frequency of cases of the birth of children with dysplasia T. s. increases with unfavorable heredity, advanced age of parents, infectious disease of the mother, endocrinopathy, toxicosis of pregnant women, breech presentation fetus. Increasing attention is paid to the teratogenic effect of ionizing radiation. Dysplasia occurs in utero and is primary, and displacement of the femoral head (subluxation or dislocation) occurs secondarily, usually in the postnatal period. With age, the number of subluxations and dislocations increases.
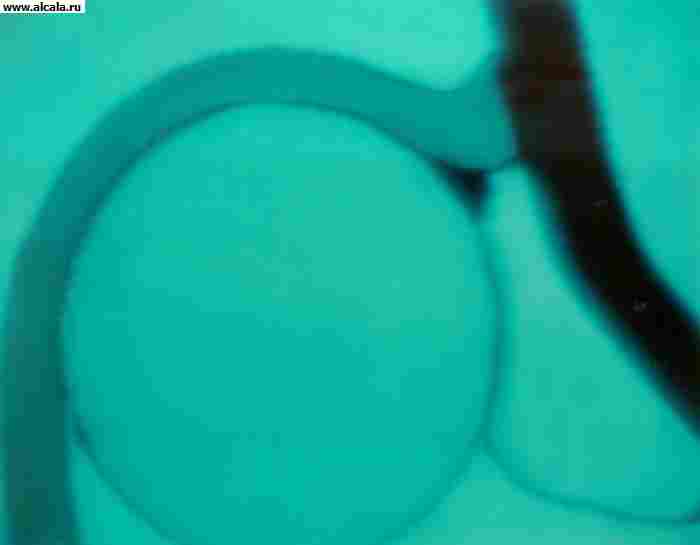
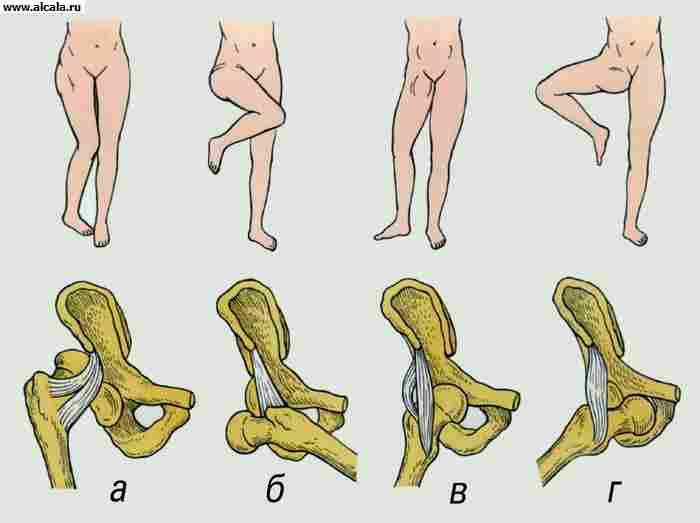
Distinguish three degrees of a dysplasia of T. of page: a preluxation, a subluxation and dislocation. The most frequent clinical signs hip dysplasia, which can be detected in the first months of a child’s life, are a symptom of slipping, or a “click” symptom, limitation of passive hip abduction on the side of the lesion, asymmetry skin folds on the hips of the child, shortening of the entire lower limb, placing the lower limb in the position of external rotation.
In children older than 1 year, with unilateral dislocation, instability or lameness is noted when walking, and with bilateral dislocation, a waddling, so-called duck gait. classic sign formed dislocation is positive symptom Trendelenburg. In addition, with pressure on the calcaneus, an increase in the mobility of the greater trochanter in the longitudinal direction and its displacement upwards is determined. Normally, the head of the femur is palpated at the level of the pulsation of the femoral artery; if the hip is dislocated, the head is not palpable at this place.
In diagnosis of a dysplasia of T. page. a significant role belongs to x-ray examination. Early radiological signs of this pathology are considered to be an increase in the slope of the roof of the acetabulum, displacement of the proximal end of the femur outward and upward relative to the acetabulum, late appearance and hypoplasia of the ossification nucleus of the femoral head.
In children older than 1 year, there are 5 degrees of dysplasia T. S.: the head of the femur is located laterally, but at the level of the cavity (I degree); head is higher horizontal line Y-shaped cartilages at the top of the acetabulum (II degree); the head is above the peak of the acetabulum, the formation of a non-cavity is possible ( III degree); the entire head is covered with the shadow of the iliac wing (grade IV); extremely high location the femoral head at the top of the iliac wing (grade V).
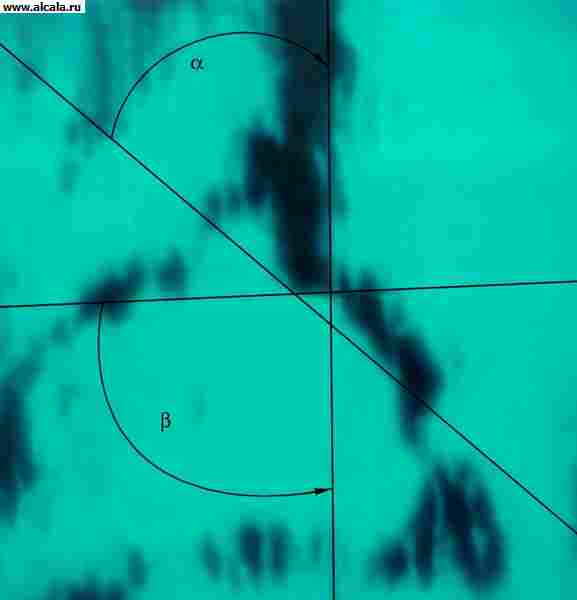
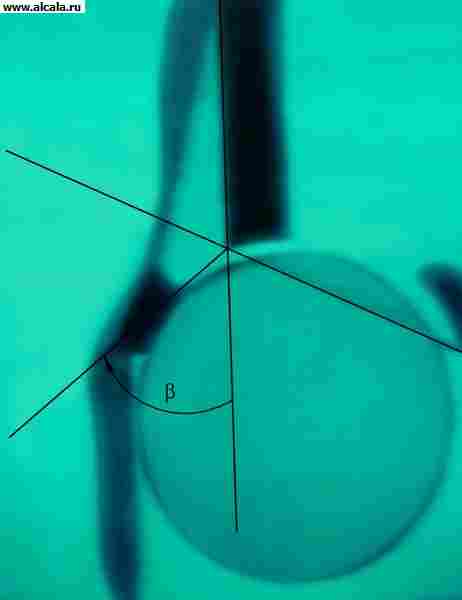
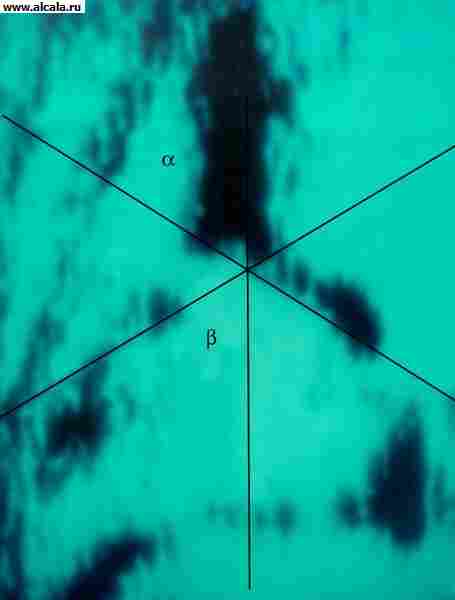
In newborns and children under 1 year old, to determine developmental disorders T. s. also use ultrasound procedure(ultrasonography). Key Benefits this method are its harmlessness to the patient, visualization of the soft tissue structures that form the joint at this age. With the help of ultrasonography, dynamic monitoring of the development of the joint during the growth of the child and its treatment is carried out. On the ultrasonogram, the degree of formation of the bone and cartilaginous parts of the roof of the acetabulum, the location of the limbus (the cartilaginous part of the acetabulum), as well as the appearance of ossification nuclei in the femoral head are determined. For quantification data of ultrasonographic examination, 3 auxiliary lines are carried out: the main line is parallel to the wing of the ilium; a line from the lower bony edge of the cavity to the upper; line from the upper bony edge of the roof of the acetabulum to the middle of the limbus. The angle formed by the main line and the bone roof line characterizes the degree of development of the bone roof. The angle formed by the main line and the line of the cartilaginous roof characterizes the degree of development of the cartilaginous part of the roof of the acetabulum. Depending on the ultrasonographic picture of T. s. and the ratio of the values of the indicated angles, all joints are divided into 4 types, in each of which subtypes are distinguished. A normally formed joint corresponds to type 1, subtypes A and B ( rice. 7, 8 ). Type 2 A (Fig. 9) is detected in children under the age of 3 months with a physiological delay in ossification of the roof of the acetabulum. Type 2 V ( rice. 9, g ) is determined in children over the age of 3 months, the development of the joint in these children requires the supervision of an orthopedist. Type 2 C corresponds to pre-luxation of the hip, such children need treatment that provides conditions for proper development joint. Type 3 A (Fig. 10) corresponds to subluxation of the hip, in this case, the normal structure of the cartilaginous part of the roof of the acetabulum is determined by ultrasonography. In type 3 B (Fig. 11), there are signs of a change in this structure, which is a poor prognostic sign. Type 4 - dislocation, the femoral head is outside the acetabulum (Fig. 12).
Treatment of a dysplasia of T. page. start from the moment you discover pathological changes. Newborns from the very first days, to eliminate the contracture of the adductor muscles, undergo therapeutic exercises, which consist in the abduction of the legs bent at the knee and hip joints. Swaddling legs should be free. To keep them in the divorced position, various pads, a pillow and a Freika envelope are used. For the same purpose, abduction (abduction) sliding functional splints CITO and others are used, which retain the possibility of movements in the joints of the lower extremities (except for hip adduction), which contributes to the formation of the roof of the acetabulum. The most favorable age for starting functional treatment of children is from 2-3 weeks to 5-6 months. The abduction splint is removed on average after 4-7 months. The duration of treatment is determined by the timing of the formation of the roof of the acetabulum. At early start treatment, patients with dysplasia or subluxation get on their feet and begin to walk at the same time as healthy children. Satisfactory results can also be achieved with the use of an abduction splint in the second year of a child's life.
With a dislocation of the hip with a high standing head and a sharp contracture of the adductor muscles (i.e. most often with late diagnosis) treatment should begin immediately with vertical traction using an abduction splint. Gradually increase the load and increase the degree of dilution of the limbs. Stretching should begin with a small load (300-500 g) on each leg, increasing it by 100-200 g daily. The maximum load is determined by the position of the buttocks (when lifting them above the bed). The term of application of traction is from 3 to 12 weeks. With an early start in the treatment of congenital hip dislocation, patients get on their feet while still in an abduction splint at the age of 8-11 months. Walking starts either with the splint on or after it is removed, usually at 12-15 months of age. However conservative methods of treatment of a dysplasia of T. page. not always effective, for example in the case of interposition of the joint capsule. Surgical interventions for most dislocations are performed in children older than 2 years. Surgical treatment it is also indicated for irreducible dislocations already at the age of 1-2 years, as well as for complications that are noted after dislocations previously reduced using conservative methods.
All surgical interventions for congenital hip dislocation are divided into intra-articular and extra-articular. Intra-articular operations include anterior capsulotomy according to Ludloff, open reduction without deepening of the cavity, open reduction with deepening of the cavity, open reduction with corrective osteotomy of the femur, Scaglietti surgery, etc. Extra-articular are reconstructive operations on the base of the ilium, reconstructive operations on the upper end of the femur (varus and detorsion-varus osteotomies), palliative operations.
With a well-formed acetabulum and a developed femoral head, a simple open reduction is possible. The operation is effective at the age of 2-4 years with unexpressed antetorsion of the femoral neck. In case of underdevelopment of T. s. the open reduction of the dislocation is combined with the deepening of the cavity or the formation of its upper edge.
With residual subluxations of the hip, T.'s instability with. in children aged 3 to 5 years, in 2/3 of cases it is due to a violation of the development of the proximal femur, and only in 1/3 - underdevelopment of the anterior superior edge of the acetabulum. By the age of 7-8, already in 50% of cases, and by the age of 10-12 in almost 100% of cases, surgery is indicated not only on the femoral, but also on the pelvic component of the joint.
With moderate underdevelopment of the acetabulum in children under 7-8 years of age, complete osteotomies in the area of the base of the ilium are effective. The Chiari operation involves, after osteotomy, the displacement of the femoral head together with the acetabulum inwards, the Salter operation - turning the cavity outward (in last years it is preferred). With a shallow depression, double pelvic osteotomy according to Pozdnikin (also at the age of up to 7 years) and pericapsular acetabuloplasty according to Pemberton, Korzh and others (up to 8-12 years) are used. In adolescents and adults with subluxations of the femoral head, satisfactory results were noted with corrective osteotomy of the femur to center the head and pelvic osteotomy according to Andrianov (plasty of the roof of the cavity).
With a high standing head, formed neoarthrosis, its operative reduction from the age of 8-10 years is not very promising. It is more expedient to perform corrective subtrochanteric double osteotomy with lengthening according to Shants-Ilizarov-Kaplunov, which allows creating an additional point of support, maintaining mobility in neoarthrosis and eliminating functional shortening of the limb.
Physiotherapy exercises are used at all stages of both conservative and surgical treatment of congenital hip dislocation. The general objectives of the use of exercise therapy are the activation of the main body systems and the prevention of complications associated with hypokinesia; improvement of circulatory conditions in the joint and lower extremities: restoration of static and dynamic dysfunctions of the musculoskeletal system (restoration of mobility in the hip joint and strengthening of periarticular muscle groups). The child's parents must be informed of the need to special exercises repeatedly during the day throughout the course of treatment.
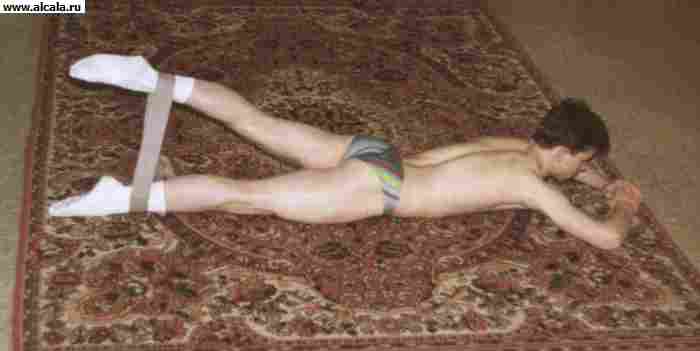
During the period of fixation of the child's limbs with various orthoses or splints, special physical exercises are aimed at strengthening the abductor muscles of the thigh. Children under 3 years of age are recommended passive and active-passive movements in T. s. for withdrawal. In the first months of life, reflex exercises are used. At an older age, exercises are performed independently with a gradually increasing load, for example, free breeding of the legs bent at the knee joints is carried out with additional external resistance to movement due to the hands of the methodologist or mother, stretching the rubber bandage that binds the hips at the level of the knee joints. Special exercises are done several times a day in combination with a light relaxing massage (superficial stroking, shaking) of the adductor muscles of the thigh. In addition to the special exercises described above, they perform respiratory and general developmental exercises for the upper limb belt.
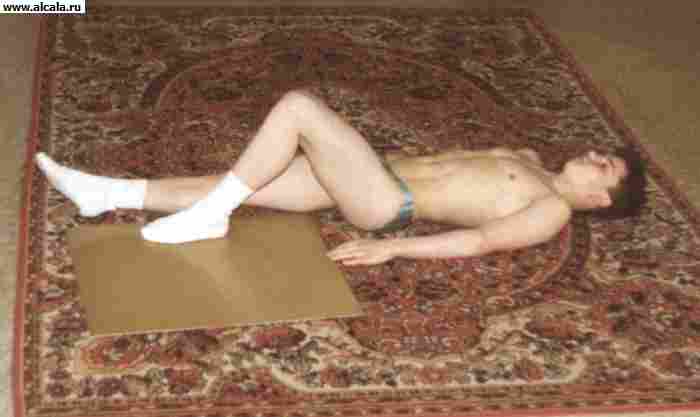
After completion of treatment in orthoses or abduction splints, it is necessary to conduct a course of manual massage (12-15 procedures) of the gluteal muscles and legs. Recommended cycling with wide-set pedals, exercise in warm water, swimming, systematic exercise. Physiotherapy aimed at restoring joint function and increasing its stability. Free exercises are used for flexion, extension, abduction, internal rotation in T. s. in the prone position: At the same time, exercises are prescribed to strengthen the abductor muscles of the thigh. Do not force your child to walk. He will get up and walk on his own when his neuromuscular apparatus is ready for vertical loading.
main goal rehabilitation treatment after intra-articular operations on T. s. is to create conditions for the restructuring of the structural elements of the joint and its functions. The special tasks of the exercise therapy used are the restoration of joint mobility, the training of the periarticular muscles, the gradual preparation for the implementation of the supporting and locomotor functions.
At operational methods treatment of congenital dislocation of the hip postoperative period(immobilization) apply general developmental breathing exercises, isometric muscle tension under a plaster cast, free and free movements with weighting in non-immobilized joints.
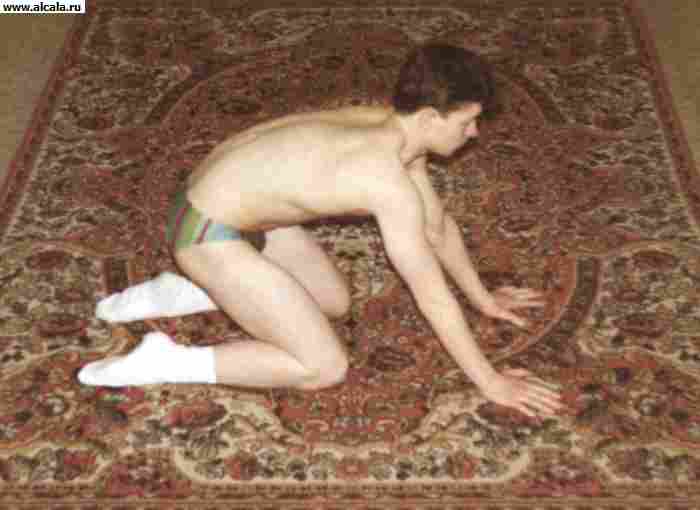
After the termination of immobilization or the use of stable osteosynthesis for osteotomy of the femur or pelvis, physical exercises are aimed at fastest recovery joint functions. To do this, light (active with self-help) movements in the hip joint, physical exercises in a hydrocolonotherapy bath in combination with manual and underwater massage are performed. As mobility in the joint is restored, exercises are added to strengthen the periarticular muscle groups and electrical stimulation of the gluteal muscles. It must be remembered that as a result of femoral osteotomy, the points of attachment of the abductor muscles of the thigh and external rotators may move, which leads to their functional insufficiency. That's why great attention give special physical exercises aimed at training the hip abductors with gradually increasing resistance. Therapeutic gymnastics is carried out in the supine position, on the side, on the stomach, as well as in the knee-hand position (on all fours). The axial load on the leg is gradually increased with good mobility, the function of the gluteal muscles, and the restoration of the bone structure of the femoral head.
Varus deformity of the femoral neck(coha vara) is manifested by a functional decrease in the cervical-diaphyseal angle. It is based on pathological restructuring along the femoral neck or directly in the area of the growth zone. Lameness, relative shortening of the lower limb, its external rotation and adduction are clinically noted. Trendelenburg's sign is positive. The greater trochanter is displaced above the Roser-Nelatin line, the symmetry of the Shemaker line and the isosceles triangle of Bryant are broken. Movements in T. with. limited, especially internal rotation and abduction.
In the early childhood attempts are being made to stop the progression of pathological restructuring in the femoral neck by long-term unloading of the joint in combination with therapeutic exercises, physiotherapy and spa treatment. Conservative treatment is effective only when early diagnosis. In older children and adults, corrective osteotomies of the proximal femur or operations aimed at restoring its support are performed.
congenital hallux valgus (plow valga) is characterized by an increase in the cervical-diaphyseal angle, is much less common. Clinically detected more low position greater trochanter, some lengthening of the limb. If the function is impaired, an intertrochanteric varus osteotomy is indicated.
Damage hip joint - bruises, traumatic hip dislocations, fractures of the head and neck of the femur, acetabulum. Bruises are manifested by local pain, limited mobility in the joint. Bleeding into soft tissues, intermuscular hematomas are possible. Treatment is conservative.
Traumatic hip dislocations usually occur as a result of indirect trauma. Depending on the position of the femoral head in relation to the acetabulum, posterior, anterior and central dislocations are distinguished (Fig. 13). In addition to pain and limitation of joint function, the forced position of the limb is noteworthy (see Dislocations). With posterior dislocations, the limb is in a position of flexion, adduction and internal rotation, with anterior dislocations, it is straightened (or slightly bent), abducted and rotated outwards. Often the femoral head can be palpated. With a central dislocation with protrusion of the head, the retraction of the greater trochanter is noted.
On radiographs, the femoral head appears outside the acetabulum. Posterior dislocations are characterized by an increase in the length of the radiological image of the femoral neck (as a result of its internal rotation), for anterior dislocations - an increase in the size of the lesser trochanter, a projective decrease in the length of the neck and an increase in the cervical-diaphyseal angle (signs of external rotation of the femur). With central dislocations, cracks in the bottom of the cavity and its comminuted fractures with protrusion of the head are distinguished.
Treatment of victims is carried out in a hospital. Before transportation, immobilization is carried out without changing the fixed position of the limb. With fresh dislocations of the hip, reduction is often performed according to the Kocher method. Subsequent unloading of the joint is carried out using skeletal traction with a load of 3-4 kg. Walking with the help of crutches is allowed after 5-6 weeks, loading the limb - not earlier than after 3-4 months. With cracks in the bottom of the acetabulum, unloading skeletal traction along the axis of the thigh is used. In fractures with protrusion of the head, traction along the axis of the femoral neck is used to extract it.
During the patient's stay in skeletal traction after traumatic hip dislocation, physical exercises are aimed at preventing hypostatic complications, improving blood circulation in the limb. Against the background of general developmental exercises, free movements are used in all joints of intact limbs and the ankle joint of the injured leg, short-term isometric tension of the thigh muscles, gluteal muscles on the side of the lesion.
After removing the traction, walking is allowed with the help of crutches with a partial load on the leg. Restoration of joint mobility is carried out in parallel with an increase in its stability by strengthening the ligamentous-muscular apparatus. To increase mobility in the joint in the initial prone position, free movements (flexion, extension, abduction, rotation) are performed in the hip joint without taking the foot off the bed or couch (Fig. 14). To strengthen the muscles, long-term isometric tension of the gluteal muscles and thigh muscles, static retention of the raised, abducted, extended leg, etc. are used (Fig. 15). It is not allowed to perform movements of a swing nature and to stretch the ligamentous apparatus of the joint, as well as training muscles with an axial load on the leg.
With fracture-dislocations T. s. therapeutic exercises are aimed at preventing the development of post-traumatic coxarthrosis. A longer unloading of the joint with crutches is recommended (up to 6 months after the injury). In the future, with long walking and the presence pain syndrome walking is recommended with additional support on a cane.
After the termination of immobilization, physical exercises in the water are shown using exercises at the side of the pool and elements of swimming, underwater and manual massage gluteal and thigh muscles, thermotherapy, ultrasound. Therapeutic gymnastics is carried out in the supine position, on the side, on the stomach with the use of free movements in the hip joint. To strengthen the muscles of the thigh, the starting position is used, standing on a healthy leg on a dais. The raised leg is held forward (to the side, back) for 3-5 s in alternation with free swing movements of the relaxed leg. In the future, when carrying out these exercises on the ankle joint, a cuff with a load of 250-500 g is strengthened. In outpatient conditions, it is necessary to repeat courses of treatment 1-2 times a year.
Diseases. Inflammatory changes in T. with. predominantly infectious origin (see Coxitis), may occur with a predominance of exudative or proliferative processes. Perhaps the primary lesion of the synovial membrane, followed by involvement in the process of the femoral head and acetabulum, or secondary (primary bone forms of coxitis).
The earliest clinical manifestations are pain in the joint area, limited mobility with the formation of myogenic contracture, and an increase in local temperature. With purulent and tuberculous coxitis, further destruction of bone structures occurs, often with hip dislocation, shortening of the limb and strengthening of its vicious position. The consequence of purulent coxitis is often bone ankylosis in the vicious position of the limb. Fibrous ankylosis is more characteristic of tuberculous coxitis. When the joint capsule is destroyed, an abscess or phlegmon of the paraarticular tissues is formed. Possible transition to chronic form with fistula formation.
One of the first radiological signs is osteoporosis. The presence of foci of destruction in the bone elements of the joint indicates an active inflammatory process. Subsequently, destruction of the articular surfaces is observed. Importance has a bacteriological study of exudate. The joint is punctured in front in the projection of the femoral head or outside above the greater trochanter.
IN acute period antibiotic therapy is indicated in combination with immobilization of the joint. TO surgical intervention resort more often with acute and purulent coxitis (arthrotomy with drainage of the joint). With extensive destruction, resection of the affected sections is carried out, usually the head and neck of the femur (i.e., draining resection). in the vicious position of the limb, extra-articular interventions are used (corrective osteotomies (Osteotomy)).
Dystrophic processes in the joint develop more often against the background of dysplasia, the consequences of injuries, inflammatory processes and metabolic disorders (see Coxarthrosis).
Chondromatosis T. s. rare; manifested by intermittent blockage and sharp pain. Surgical treatment - removal of intra-articular bodies (see Chondromatosis (Chondromatosis of bones and joints)).
The causes of aseptic necrosis (see Aseptic bone necrosis) of the femoral head are different. It is manifested by pain, lameness, limited movement (see Perthes disease). With the ineffectiveness of conservative treatment (unloading the joint, physiotherapeutic procedures), they resort to surgical intervention (corrective osteotomy, arthroplasty, arthrodesis).
Tumors can come from the joint capsule (see Synovioma), cartilage and bone tissue. In the proximal femur, osteoblastoclastoma, osteoma, chondroblastoma, chondroma, chondrosarcoma, and osteogenic sarcoma are observed (see Joints, tumors). Surgical treatment: resection with osteoplastic replacement of the defect or arthroplasty of the proximal femur, disarticulation of the femur.
Operations
For drainage and revision resort to arthrotomy. Osteosynthesis or Endoprosthetics are performed for medial fractures of the femoral neck. In order to improve statics, corrective osteotomies of the proximal femur are performed. Arthroplasty is used to restore joint mobility. To this end, there are various options endoprosthesis. To restore the support of the thigh, arthrodesis is performed (see Joints). With dysplasia T. s. in addition to corrective osteotomies of the proximal femur, reconstructive operations on the pelvic component are indicated in order to increase the degree of coverage of the femoral head.
See also Thigh.
Bibliography: Human Anatomy, ed. M.R. Sapina, vol. 1, p. 144, M., 1986; Vilensky V.Ya. Diagnosis and functional treatment of congenital hip dislocation, M., 1971, bibliogr.; Volkov M.V., Ter-Egiazarov G.M. and Yukina G.P. Congenital hip dislocation, M., 1972; Kaplan A.V. Damage to bones and joints, p. 355, 359, Moscow, 1979; Conservative treatment of children with diseases of the musculoskeletal system., ed. E.S. Tikhonenkov, p. 73, L., 1977; Korzh A.A. and others. Dysplastic coxarthrosis, M., 1986; Marks V.O. Orthopedic diagnostics, p. 355, Minsk, 1978; Mirzoeva I.I., Goncharova M.N. and Tikhonenkov E.S. Surgical treatment of congenital hip dislocation in children, L., 1976; Orthopedic and trauma care for children, ed. V.L. Andrianova, p. 39, 44, L., 1982; Pathology of the hip joint, ed. V.L. Andrianova, p. 4, L., 1983; Shkolnikov L.G., Selivanov V.P. and Tsodyks V.M. Damage to the pelvis and pelvic organs, M., 1966.













![]()









formed by the acetabulum and the head of the femur. Both articular surfaces are covered with cartilage. The acetabulum is part of the pelvis, located at the confluence of the ilium, ischium and pubis. The articular bag goes along the edge of the articular cavity, passes to the femur and is attached above its skewers, so most of the femoral neck is located in the cavity of the hip joint. The articular bag is very strong, reinforcing ligaments are woven into it. T. s. refers to multiaxial joints - flexion and extension, adduction and abduction, rotation of the thigh outward and inward are possible. It is supplied with blood from regional vessels.
First aid is provided for injuries of the hip joint of various severity. So, with bruises in the area of T. s. pain is noted, swelling and hemorrhage are usually poorly expressed, movements in the joint are not limited. In this case, it is enough to apply cold and unload the joint until the pain subsides. For small superficial wounds in the joint area, a sterile pressure bandage is applied. Intra-articular fractures and dislocations of the hip joint are severe injuries. Unlike a bruise in case of fractures of the bones that form T. s., the leg is in a forced position, for example, it is turned outward, the victim cannot raise the injured leg, and the pain intensifies when trying to move. With some fractures of the neck of the femur (for example, impacted), swelling in the area of T. s. expressed slightly, sometimes the victims can even move independently. With fractures of the trochanteric region, swelling and hemorrhage are more extensive and extend to the upper third of the thigh. Due to the fact that the final diagnosis can only be made after a special examination, and external manifestations extensive bruising of the area T. s. and fractures are very similar, the volume of first aid should be the same as for a fracture. It is very important to immobilize the hip joint well before transporting the victim to the hospital. It is better to use the Dieterichs tire for this (see. rice. 4 to the article Hip), and in its absence - improvised tires of a sufficiently large length.
Dislocations in the hip joint are relatively rare. As a rule, they occur with severe mechanical trauma, for example. as a result of a traffic accident or a fall from a height. The head of the femur, moving, breaks the articular bag with the ligaments that strengthen it and is located in the periarticular tissues. The leg is in a forced position ( rice. ), movements in T. s. impossible, immediately after the injury appears strong pain. When giving first aid, you should not try to "correct" the position of the leg. The victim urgently needs to be taken to the hospital for examination and reduction of the dislocation. The immobilization of the damaged joint is carried out in the position in which it is after dislocation. At the same time, unnecessary movements should be avoided, because. they increase pain and may cause additional injury, eg. sciatic nerve injury.
At open damages of area T. page. a sterile dressing is applied to the wound. A pressure bandage is applied to small wounds, with more extensive damage to soft tissues, the joint is immobilized as in a fracture.
Splinting- see thigh.
bandages, used in first aid in connection with damage to the area of T. s., more often bandage, rarely use a mesh bandage. For small wounds, you can apply an adhesive bandage. Depending on which area is closed, a one-sided (right, left) or two-sided spiky bandage of the pelvis can be used, as well as an anterior, covering the inguinal region, an external (lateral), covering the region of the greater trochanter, and a posterior, covering the buttocks region. When applying the right-sided anterior (inguinal) spica bandage of the pelvis, the first round of the bandage is made around the body at the level of the navel, leading the bandage from left to right, the next round is carried out obliquely from back to front along the side, and then along the front surface of the right thigh to its back semicircle and turn obliquely up and inside, crossing the previous round of the bandage in the inguinal region. Next, the bandage is led over the pelvic bones on the left side, and from there it is directed to the posterior semicircle of the body and again to the groin area, repeating the previous rounds of the bandage and overlapping them by 2/3 of the diameter. Finish the bandage with circular tours of the bandage around the torso. Subsequent rounds of the bandage can be ascending (each next round is higher than the previous one) or descending. When a similar bandage is applied to the area of the left groin, the bandage also goes from left to right, but after the first fixing tours around the body, it goes obliquely from behind to the front surface of not the right, but the left thigh, bypasses its back surface and then goes obliquely up the thigh, crossing with the previous round, goes around the body from behind and again goes to the front surface of the left thigh, repeating the previous rounds and covering each of them by 2/3 of its width. The bandage is also finished with circular tours of the bandage around the torso. For greater strength, each eight-shaped bandage (spike) tour can be fixed with one circular tour.
If necessary, close with a bandage bandage T. s. on all sides, a slightly different version of the spike-shaped bandage is used - the spike-shaped bandage of the thigh, which is started in a circular motion not on the body, but approximately on the middle third of the thigh. According to the method of application, it is similar to a spike-shaped shoulder bandage, i.e., having fixed the bandage on the thigh, the bandage is led along the outer surface of the T. s. to the lower back, make a fixing circular tour around the body and continue bandaging in the same way as when applying a spike-shaped bandage of the pelvis, gradually overlapping the previous tours.
In emergency cases or in the absence of other dressings, you can use scarf bandages on the T. area. To do this, use two scarves. One middle is placed over the damaged area of tissue, its ends are wrapped around the thigh and tied, and the third end (top) is brought under the belt formed from another scarf, folded back and fastened with a pin. In the absence of a second scarf, you can use a belt.
Anatomy
The hip joint is a spheroidal joint formed by the round head of the femur and the cup-shaped acetabulum. The acetabulum is formed by the fusion of three bones: the ilium, ischium, and pubis. Along the edge, the acetabulum is surrounded by a fibrocartilaginous fold that deepens it - a lip, which reduces the diameter of the exit from the cavity, forming a cartilaginous rim covering the femoral head. Bottom part the lip is open and forms an acetabular notch, which is occluded by the transverse ligament, turning the notch into an opening through which blood vessels pass into the joint.
The articular capsule is strong, dense, attached proximally to the edge of the cavity, to the lip and transverse ligament. Distally, the capsule surrounds the femoral neck and attaches anteriorly to the intertrochanteric line, and posteriorly to the femoral neck.
The hip joint is fixed by a number of ligaments (Fig. 24).
Rice. 24. Hip joint (front view): ligament apparatus
The iliofemoral ligament, crossing the anterior surface of the capsule, stretches from the anterior inferior iliac spine to the anterior surface of the base of the femoral neck and the intertrochanteric line. When the trunk is straightened, the ligament prevents the pelvis from turning backward around the femoral head, strongly pressing the femoral head into the cavity.
The pubic-femoral and ischio-femoral ligaments cover the hip joint along the medial-inferior and posterior surfaces, respectively, limiting abduction, rotation, and adduction of the hip. The pubic-femoral ligament extends from the pubic bone down to the lesser trochanter, and is woven into the articular capsule. The sciatic-femoral ligament begins behind the joint from the cartilaginous rim of the acetabulum in the area of the ischium, goes laterally and upward, merging with the circular fibers of the capsule at the inner surface of the greater trochanter.
The round ligament of the thigh is an intracapsular ligament that runs from the head of the femur to the bottom of the glenoid cavity. It is a channel through which blood vessels pass into the head of the femur.
The synovial membrane lines the deep surface of the articular capsule and surrounds the round ligament in the form of a vagina.
In the area of the hip joint there are a number of synovial bags: iliac-comb, trochanteric, ischio-gluteal (Fig. 25).
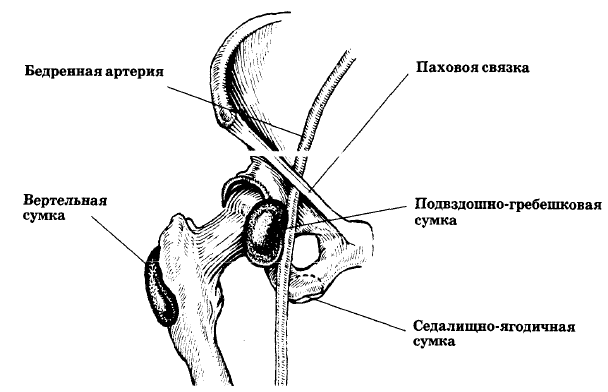
Rice. 25. Hip joint (front view): location of mucous bags
The iliac-scallop bursa lies between the posterior surface of the iliopsoas muscle and the anterior surface of the joint in the interval between the iliac-femoral and pubic-femoral ligaments.
Normally, it communicates with the joint cavity in 15% of cases.
The trochanteric bursa is located between the gluteus maximus muscle and the posterolateral surface of the greater trochanter. The bag separates the deep surface of the gluteus maximus muscle from the ischial tuberosity and from the vastus lateralis muscle of the thigh.
The ischio-buttock bag lies on the ischial tuberosity.
- Bone landmarks
The iliac crest terminates anteriorly in the anterior superior spine and posteriorly in the posterior superior spine. The ischial tubercle lies under the gluteal muscle and is easily palpated with the hip bent. The greater trochanter is located below the iliac crest at a distance equal to the width of the palm, halfway between the ischial tuberosity and the anterior superior spine.
Features of diagnostics
The hip joint is the joint most deeply located under the soft tissues, so exudative changes, swelling and pain on palpation can be detected in extremely rare cases. Sometimes informative deep palpation over the middle of the inguinal ligament and somewhat distal to it. Basically, when diagnosing lesions of the hip joint, one has to focus on complaints, pain and limitation of mobility during passive movements, and x-ray data. Typical are complaints of pain when walking, often at rest, in the gluteal and inguinal regions, as well as in the proximal lower limb along the femur. Mobility in the hip joint is examined in the position of the patient lying on a hard couch. Extension in the joint is performed in the position of the patient on the side, all other types of movements - on the back. The angle of flexion, which is normally equal to 115°, is determined by pulling the limb bent at the knee joint to the stomach as much as possible. In this case, it is necessary to ensure that the pelvis does not take part in flexion. Hip extension (20°) is checked by pulling the straightened leg backwards, immobile pelvis and spine. The amplitude of abduction and adduction (45° and 40°, respectively) is also determined with the limb extended, with one hand grasping the ankle and moving the leg in the appropriate direction, and with the other, fixing the pelvis by pressing on the crest of the opposite iliac bone. It is also advisable to perform abduction with the hip and knee joints bent at 90 ". One of the most early signs lesions of the hip joint are the limitation and pain of rotational movements that are performed by a limb bent at 90 ° in the hip and knee joints. A variant of this study is rotation with moderate pressure on the knee joint towards the hip joint. At healthy individuals the angle of internal and external rotation is 45°. It should also be remembered that there is a need for a comparative measurement of the true length of the limbs (from the anterior superior iliac spine to the medial malleolus). If it is the same on both sides, and only the visible length of the legs differs (from the navel to the medial malleolus), then this may be due to a pelvic tilt, which in some cases is due to other reasons (for example, changes in the spine).
In rheumatoid arthritis, the hip joint is usually painless or slightly painful until all of the load-bearing cartilage has been destroyed. IN this case pain is primarily associated with mechanical damage, which characterizes the late stage of the process. In violation of the congruence of the articular surfaces, the friction of the femoral head against the acetabulum during walking often produces a loud, characteristic creak that can be heard from a distance. A similar situation is observed with the involvement of the hip joint in psoriatic arthritis, ankylosing spondylitis, Reiter's syndrome and other types of arthritis.
At the same time, in some cases, pain and limitation of movements in the joint are ahead of pronounced violations of the anatomical relationship between the femoral head and the acetabulum. These manifestations may be due to aseptic necrosis of the femoral head, osteophytes in osteoarthritis, and in ankylosing spondylitis - ossification of the capsule. The above causes can be diagnosed clinically and confirmed by X-ray examination.
However, in the area of the hip joint there are places where pain can occur that is not associated with the joint itself. This is the region of the greater trochanter, where the source of pain may be damage to the bags of greater trochanters or enthesopathy, ischial tuberosity, the area of innervation of the lateral cutaneous nerve of the thigh.
- Greater trochanter area
It is often impossible to differentiate pain that occurs in the greater trochanter sac from pain that occurs at the attachment of muscles and tendons to the greater trochanter (enthesopathy). This is the area of attachment of a powerful fibrous layer, the gluteal fascia, to the top of the greater trochanter. The insertion of the gluteus medius is also closely related to the fascia in this area. Lateral and below is the place of attachment of the gluteus maximus muscle and the bag lying under it. Wherever the source of pain is localized, the method used to relieve it is the same.
Pain in the region of the greater trochanter is observed with various types polyarthritis (usually rheumatoid, ankylosing spondylitis), as well as in the "snapping hip" syndrome, which occurs after a complex (combined) movement in the hip joint. The patient discovers that with simultaneous adduction and flexion of the hip, a clicking sound occurs in the joint area, due to the passage of the iliofemoral ligament over the top of the greater trochanter. This can irritate the underlying structures and subsequently be a constant source of pain when walking, which the patient tries to alleviate by further clicking.
The ischial tuberosity is palpated deeply from the medial side of the buttocks. It bears the entire weight of the body in a sitting position. Although the ischial tuberosity is well wrapped in subcutaneous fatty tissue, protected by a mucous bag and muscles attached here, it sometimes becomes painful. This may be due to inflammation of the ischio-gluteal bursa or enthesopathy in ankylosing spondylitis and other seronegative arthritis. In some cases, the obvious cause of the pain cannot be found,
- Neuralgia of the lateral femoral cutaneous nerve (Roth-Bernhardt disease))
Roth-Bernhardt disease is a neuropathy resulting from entrapment of the lateral femoral cutaneous nerve at its passage through the deep fascia approximately 10 cm below and medial to the anterior superior iliac spine. The nerve provides skin sensitivity to the anterior and lateral surfaces of the mid-thigh. It does not have a motor branch. Typically there is a well-defined oval area of attenuation or loss pain sensitivity with a pin prick on the anterolateral surface of the thigh. There are also tactile and thermal paresthesias in the area of nerve innervation. Patients usually accurately determine these sensations on the skin. The described symptomatology contrasts with the pain felt in the middle of the anterior-lateral surface of the thigh, which is associated with injuries in the spine (I-III lumbar vertebrae). They cannot be accurately identified by the patient.
Diagnosis is confirmed by local tenderness at the site of nerve exit from deep tissue through the dense fascia of the upper thigh, usually 10 cm below the anterior superior iliac spine. This point can be determined by careful palpation or with with the help of a lung hammer tapping.
Roth-Bernhardt disease must be differentiated from initial manifestations shingles in the area of the anterior surface of the thigh, since the pain is also superficial and can be quite accurately localized. There are other sources of pain in this area. Thus, the pain associated with the defeat of the hip joint is specified by a thorough study of the range of motion in it, especially rotation, abduction and rotation in the bent position of the hip joint. It should also be remembered that pain in this area can be due to Paget's disease, bone damage in the thigh and pelvic bones.
Injection Therapy Technique
There are almost no indications for injections into the hip joint. This is due to the following reasons.
Firstly, the appearance of significant pain in the hip joint during movements on the background of rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, Reiter's disease, other reactive arthritis, as a rule, indicates the presence late stages lesions, when intra-articular injections of PHCS are unlikely to help. In these cases, you should think about the need for joint prosthetics. Injection therapy for aseptic necrosis of the femoral head is not only inappropriate, but can be harmful. With predominantly degenerative-dystrophic lesions (deforming osteoarthritis, ossification of the capsule), additional traumatization of the joint can also aggravate the course of the pathological process.
Secondly, the decrease in pain intensity after intraarticular administration of PHCS is more associated with the manifestation of the systemic effect of the drug and is comparable with the effectiveness of intramuscular administration.
Thirdly, long needles and correct determination of the direction of the needle during insertion are necessary to penetrate the joint. The complexity of the latter is due to the fact that it is impossible to palpate the space between the two articulating bones, as can be done with an injection into the knee or wrist joints. Moreover, it is often impossible to be sure that the needle has penetrated the joint. It is difficult to aspirate fluid from the hip joint experienced specialist using X-ray control, except when the joint capsule is stretched by chronic synovitis for a long time. As with other joints, an attempt to aspirate synovial fluid may be unsuccessful due to its increased viscosity or blockage of the needle by solid particles.
In addition, it is often difficult to exclude secondary purulent arthritis. However, circumstances may arise in which it is necessary to puncture the joint precisely in order to exclude infectious arthritis. The technique of aspiration of fluid from the joint is the same as the technique of intra-articular injection.
In a patient lying on his back with a slightly bent and internally rotated hip joint, the position of the anterior superior iliac spine, pubic tubercle and greater trochanter is noted. Then, with the help of palpation, the femoral artery is found and its position is noted. All injections and punctures for aspiration should be done lateral to the artery. With an anterior approach, the skin and underlying tissues are anesthetized, and the aspiration needle or trocar, observing complete asepsis, is inserted lateral to the artery, 2 cm below the inguinal ligament. If the needle rests against the bone and there is no fluid, then it is partially removed and re-introduced, directing it lateral to the femoral neck, focusing on the position of the greater trochanter. For lateral access, the skin should be pierced more laterally, at the level of the lower edge of the greater trochanter, and the needle should be directed inward, medially and upward along the line of the femoral neck. The needle is inserted until it touches the bone, then pulled back slightly and re-introduced at a lower angle until it passes through the capsule and synovial membrane.
- Greater trochanter area
The patient is laid on a couch or table on his side, facing the doctor, the diseased thigh is on top and bent. The second leg is straightened at the hip joint. It is necessary to palpate the elevation of the greater trochanter, find the points of maximum pain and mark them. A mixture consisting of a 1% solution of lidocaine and 1 ml of metipred or diprospan is drawn into a 10 ml syringe. A needle with a length of at least 5 cm is used. After treating the skin with an antiseptic, the needle is inserted into the designated point and advanced until its tip reaches the top of the greater trochanter. If the needle rested against the bone, then it is necessary to remove it a little and move it again at a large angle to the horizontal. The goal is to reach the insertion site of the gluteal fascia. The entire area is extensively infiltrated with a mixture of local anesthetic and PHCS. The procedure is performed in a similar way if the pain is localized at the site of attachment of the gluteus maximus muscle below the posterolateral edge of the greater trochanter.
- Area of ischial tuberosity
The injection into the area of the ischial tuberosity is the same as in the area of the greater trochanter [Fig. 26]. After careful palpation, the point of maximum pain sensitivity is determined and this area is infiltrated with the drug mixture.
Rice. 26. Injection into the ischial tuberosity
To perform this manipulation, the patient should lie on the couch on his side, facing away from the doctor. 10 ml of lidocaine and 1 ml of PGCS are drawn into the syringe and the area of pain sensitivity is widely infiltrated with a long needle.
- Neuralgia of the lateral femoral cutaneous nerve (Roth-Bernhardt disease)
After determining the exit point of the nerve through the fascia in the upper thigh, this area is infiltrated with a mixture of 5 ml of local anesthetic and 0.5 ml of PGCS.
The articular cavity of the hip joint is formed by the pelvic bone and is called the acetabular (acetabular) cavity. Along the edge of the cavity is the acetabular lip - a fibrocartilaginous formation. It increases the depth of the cavity by 30%, but its main function is to uniformly lubricate the articular cartilage of the femoral head with synovial fluid (articular). By creating a suction effect, it strengthens the hip joint.
Inside the acetabulum is the head of the femur, which is connected to the body of the femur through the neck. Often the neck of the femur is referred to as the "neck of the femur", but this is jargon. Slightly below the femoral neck are bone elevations called the greater and lesser skewers. Powerful muscles are attached to them.
Around the joint there is a joint capsule that contains ligaments that strengthen the hip joint. On the one hand, these powerful ligaments are attached at one end to the pelvic bone, and at the other end to the femur. Another powerful ligament (called the ligament of the femoral head, often also called the round ligament) connects the head of the femur to the floor of the acetabulum. It is possible that this ligament also adds strength to the hip joint by limiting the external rotation of the hip. The capsule of the hip joint serves the same purpose, which is stretched during external rotation and extension of the hip.
The hip joint is covered by the muscles of the gluteal region at the back and the muscles of the anterior thigh group at the front. The head of the femur, located in the acetabular cavity, is covered with articular cartilage. The articular cartilage in the hip joint reaches an average of 4 mm in thickness, has a very smooth surface of a whitish color and a densely elastic consistency. Due to the presence of articular cartilage, friction between the contacting articular surfaces is significantly reduced.
A bone can only live when it receives blood. The blood supply to the femoral head is carried out in three main ways:
1. Vessels leading to the bone through the joint capsule
2. Vessels running inside the bone itself
3. Vessel passing inside the ligament of the femoral head. This vessel works well in younger patients, but in adulthood this blood vessel usually thins and closes.
The muscles that move the leg in the hip joint are attached to the bony protrusions of the pelvic bones and the upper end of the femurs.
Causes of pain in the hip area
It is sometimes difficult to establish the cause of pain in the hip joint, since it can be caused not only by local damage or disease, but also by a pathological process in abdominal cavity, in the lumbar spine or in the genitals.
!!! Often, pain in the hip joint radiates to the knee joint.
Basically, the causes of pain in the hip joint can be divided into four groups:
1) injuries in the hip joint and their consequences:
contusions of the pelvis, hip joint and upper thigh (including Morel-Lavallée syndrome, myositis ossificans);
ruptures of the acetabular lip;
sprains, partial and complete muscle tears and avulsion fractures, including hamstring syndrome;
fatigue fractures (stress fractures) pelvic bone, femur, stress fractures of the femoral neck are especially dangerous;
damage to the ligaments and joint capsule;
APS syndrome or APC syndrome;
fractures of the neck of the femur;
pelvic fractures;
fractures in the region of the trochanters of the femur;
dislocations of the femur.
2) diseases and individual characteristics the structure of the hip joint, its ligaments, surrounding muscles:
snapping hip;
free intraarticular bodies of the hip joint and chondromatosis of the hip joint;
impingement syndrome (femoral-acetabular impingement syndrome);
arthrosis of the hip joint (synonyms: osteoarthritis, coxarthrosis, osteoarthritis);
trochanteric bursitis (trochanteritis), sciatic bursitis, iliac crest bursitis;
proximal ilio-tibial tract syndrome;
piriformis syndrome;
tendonitis and tenosynovitis;
osteonecrosis of the femoral head (avascular necrosis, aseptic necrosis);
transient osteoporosis;
3) diseases and injuries of other organs and systems, which are manifested by radiating (radiating) pain in the hip joint:
neuralgia of the lateral femoral cutaneous nerve common cause pain in the hip joint in pregnant women, patients diabetes);
neurological diseases of the spine;
sports pubalgia;
dysplastic coxarthrosis.
arthritis (polymyalgia rheumatica, gout, rheumatoid arthritis, systemic lupus erythematosus, arthritis in inflammatory diseases intestines - Crohn's disease);
Ankylosing spondylitis;
psoriatic arthritis;
arthropathy Charcot (Charcot);
fibromyalgia;
leukemia;
Paget's disease;
infectious diseases hip joint (Lyme disease, Reiter's syndrome, tuberculosis, etc.).
There are other causes of pain that are difficult to classify (toxic synovitis, primary and secondary oncological lesions, osteomalacia, osteomyelitis, etc.)
Many of these causes are interrelated: for example, osteoarthritis of the hip joint may be the result of chronic traumatization, arthritis may be post-traumatic in nature, etc. hip area and treatment.
Typical features characteristic of joint pain
At the very beginning of the development of diseases, the joints hurt intermittently and slightly. So a person, at this time, does not pay attention to them and quickly forgets. And he remembers only when he answers the questions of the doctor and, as a rule, if it turns out that the pain in the joints began 3-4, or even 5 years ago, then we can already say that the disease is slowly but surely close enough approached you. It is no coincidence that they say, for example, about deforming arthrosis, that it “sneaks” imperceptibly. If during this “creeping” period you start the right preventive treatment, then the development of the disease can be stopped.
Pain in the hip joints have typical features:
1. Mechanical pain- occurs when the joint is loaded. They are more bothersome in the evening and usually go away or subside after a night's rest.
2. Starting pains- appear at the beginning of the movement, when standing up, at the beginning of walking, with any load on the diseased joint. Then these pains disappear. Often people say: “I’ll walk 10-50-100 meters and the pain goes away”
3. Night pains. The name itself indicates the time of their occurrence. As a rule, they are dull, aching in nature and disappear in the morning when walking.
4. Reflected pains. Sometimes pathological processes can occur in the spine, and pain can be in the hip and knee joints, and even in the foot, but not in the spine itself. In diseases of the hip joint, treatment is often carried out knee joint because it is the knee that hurts, not the hip joint. All these pains are called referred pains.
When should you see a doctor
In case of severe, constant or long-lasting pain, visible deformity of the joint, reddening of the thigh and its heating, discoloration of the leg below the thigh and impaired sensitivity, as well as if an injury is suspected, it is necessary to urgently consult a doctor. When you talk about the hip and your doctor says the same word, you may be talking about different things. Most people, when they talk about hip pain, they mean pain in the upper thigh or buttocks, where the rounded places are. female figure. As for the doctor, this means pain in the groin - at the location of the hip joint itself.
As already mentioned, the origin of hip pain can be difficult to determine. You may feel pain inside the joint. Pain is noted in soft tissues in the joint area - for example, in a bag. (The bursa is a sac filled with fluid. It envelops that part of the femur that is closer to the surface of the body. If the bursa becomes inflamed, then they talk about the development of bursitis.) There are also tendons in the femur. They connect the thigh to other bones of the limb and the spine. An inflammatory process can also occur in the tendons (often after an injury). This condition is called tendinitis. The pain you feel in your hip may be coming from somewhere else. Possible pain due to irradiation. This means that you feel pain in the hip, and its source is located in another place, for example, in the spine. Hip pain is caused by a mattress that is too soft or uncomfortable shoes.
Often, especially in older people, pain in the hip joint is the result of arthritis. Usually it is osteoarthritis - a disease of the so-called "worn out" joints. This type arthritis occurs in almost all people during the aging process. Osteoarthritis of the hip joint is especially common for people who have had a hip or pelvic fracture in the past.
It is also possible to damage the joint (although much less often) due to rheumatoid arthritis. This disease is associated with a potential threat of disability. It usually starts at young age.
Sometimes the reason lies in the defects of the skeleton. Pain can occur, for example, with a curvature of the spine or when one of the lower limbs becomes shorter than the other.
Although overweight does not belong to the category of defects in the body structure, the hip joint will respond to this. Overweight can cause hip pain regardless of other disorders.
If you experience pain in the hip joint, you may need the help of such specialists:
- Rheumatologist.
- Traumatologist or orthopedist.
- Physiotherapist.
- Neurologist
Pain in the hip joint - a disease of the joint or a disease of the spine?
This issue must be resolved by the doctor when the patient complains of pain throughout the back, lower back, gluteal region, inguinal region. After all, the examination, diagnosis and treatment appointment depend on the picture of the disease.
Pain in the hip joint can occur due to damage directly to the hip joint itself or due to damage to the surrounding soft tissues.
The most common diseases that give pain in the hip joint arecoxarthrosis (arthrosis of the hip joint) and intervertebral hernia.
With arthrosis of the hip joints, the earliest and most sensitive sign of the disease is limited internal rotation with flexed hip and hip pain. As a rule, the pain comes from the upper part of the thigh and gives to the knee, which is especially felt when walking. Often aggravated by standing on one leg (on the affected side).
With inflammation of the hip joint usually its back and side surface hurts. Frequent mlocation pain- groin area(projection of the joint space). May join later crunch and joint stiffness.
Pain in the hip area tends to increase sharply with movement, the skin over the joint may be swollen, with signs of inflammation
The mechanical rhythm of pain is characteristic, that is, their occurrence in evening hours under the influence of daytime load and subside during the night rest. Such pains indicate that there has already been a decrease in the depreciation properties of cartilage and the osteoarticular surface to loads. At night, dull pains associated with venous stasis in the subchondral bone and increased intraosseous pressure may disturb. When walking, these pains usually disappear.
All this leads to changes in muscle tone, ligament tension, the position of the pelvic bones, and the spine.
Literally the following happens: the configuration of the hip joint changes, the leg shortens, the pain intensifies, the person loads the sore leg less when walking, the muscles on the groan of the affected joint weaken (hypotonicity), and the muscles on the opposite side compensatory become stronger (hypertonicity). The difference in the tone of the muscles of the thighs, deep and superficial muscles of the lower back and pelvis leads to a distortion of the pelvic bones.
Since the bones of the pelvis are connected by the sacrum to the lumbar vertebrae, in pathological process the spine is gradually involved. The load on the lumbar vertebrae increases, often there is a shift of neighboring vertebrae relative to each other - antelisthesis of the vertebral bodies.
Next, the spinal nerves (roots) are inevitably affected. spinal cord), which are responsible for the nutrition and functioning of the muscles, ligaments and vessels of the leg. A person feels pain in the lower back, weakness, pain and chilliness of the leg. In severe cases, weakness and weight loss of the leg can join the constant pain, urinary incontinence develops.
Now consider the reverse situation - can a disease of the spine lead to pain in the hip joint? Unfortunately, maybe.
Such pains appear in the presence of herniated discs. lumbar, with long-term painful spasm of the muscles of the lower back, or with a combination of both factors.
Lumbar disc herniations can compress the nerve fibers (roots) that exit on both sides of each vertebra and are then located in the tissues and organs of the pelvis and muscles of the lower extremities. Compression (squeezing) of the spinal nerves disrupts the nutrition of the muscles and ligaments around the hip joint (or both joints). In such cases, people experience deep aching pain in the lumbar region, in the groin, in the buttocks, thighs, but they cannot pinpoint the exact location of the pain. Sensitivity disorders in the form of a feeling of "goosebumps", numbness, coldness, "leakage" of the legs, as well as decreased sensitivity of the skin on the side of pain.- also a sign of compression of the spinal nerves.
With intervertebral hernia of the lumbar pain in the joint worsens with exertion or movement (eg, rising from a sitting position, standing, walking, standing up on toes) and is felt primarily in the groin. However, it can radiate along the anterior and lateral surface of the thigh, into the buttocks, into the anterior part of the knee, and occasionally along the anterior surface of the lower leg up to the ankle joint.
A prolapsed intervertebral disc can cause pain in the groin. The abrupt nature and aggravation on exertion (cough + additional pain in the back) allow us to establish its nature.
Painful spasm of the muscles of the lumbar region appears after an unusual physical activity or awkward movement when lifting weights. In this case, the spinal nerves are not affected, but the spasmodic muscles themselves are a source of pain.
With a large hernia, movement in both legs can be painful. In the vertical position of the body, pain in the hip joint caused by pinching of the spinal nerve may decrease slightly.
Localization of pain in other most common diseases of the hip joints is as follows:
Trochanteric bursitis causes local pain and tenderness over the trochanter, sometimes radiating down the lateral surface of the thigh. It is especially painful when lying on a sore side. The pain of ischio-gluteal bursitis is felt mainly from behind and worsens when the patient is sitting.
Fibrosis of the joint capsule leads to compression of nerve endings, which leads to pain during certain movements associated with stretching of the capsule
Constant pain with any movement in the joint, it can cause a reflex spasm of nearby muscles. Tension in the groin is usually a consequence sports injury and aggravated by standing on the affected leg.
Unfortunately, people often do not apply for medical care immediately, hoping that "everything will pass by itself." This can lead to further damage to the spine and joints and increased pain. A timely visit to the doctor will help to avoid serious consequences. Additional studies will help to identify the exact cause of pain in the hip joint and lower back: X-ray, MRI
The hip joint usually responds well to treatment, except in cases of significant destruction of the tissues of the joint. It is important not only to relieve inflammation and pain, but also to pay attention to blood circulation in the joint, and to ensure its nutrition, and correct work muscles.
First aid for hip pain
If you suspect that mild pain is due to a minor injury or joint overload, the following steps can be taken:
!!! Even with a slight suspicion of a fracture of the femur, it is urgent to call a doctor.
Therapeutic effects to alleviate and eliminate pain
Pain in the hip undoubtedly creates obstacles and causes anxiety. Fortunately, there are many ways to reduce their intensity.
With hip pain, great attention is paid to reducing the load on the joint. It is better to do housework in a sitting position, wash the floors only with a mop, and not tilt, the height of the chair and toilet should be sufficient, it is better to install handrails in the bathroom to make it easier to climb.
Limit exercise. You should shorten the program exercise(but you do not need to completely abandon them) for several weeks, while the pain remains the most severe. Give yourself the opportunity to improve your health. Do only warm-ups, refrain from lifting weights.
Try skin rubbing ointments. The ointments themselves and rubbing the skin and muscles with them reduce tension in the muscles of the thigh. Try using ointments such as Ben-Gay, Flex-ol 454, or Eucalyptamine. Never use menthol ointments with heating pads. This may cause burns.
Use massage. Whether you do it on your own or with the help of a spouse, massage is a powerful remedy for hip pain. During the massage, the main efforts are directed to the tissues in the circumference of the joint, and not to the joint itself, since it is they who most often hurt. Since there are so many types of massage, ranging from Swedish to Shiatsu, you need to find out during the experiment which one brings more relief.
Ask about medications. If common drugs such as aspirin and acetaminophen do not relieve pain, your doctor may prescribe stronger drugs for you. He will also advise you on cortisone injections or tablets. This is an excellent tool for quickly reducing inflammation in the first few days after an injury.
Provide yourself comfortable position during sleep. Try not to lie on the affected hip. On top of a regular mattress for greater softness, place a mattress made of porous material.
Use appropriate footwear for walking. Buy running shoes for walking, not walking, aerobics or cross-country. They are very light and are designed to increase foot stability.
Choose the right cane for you. The use of a cane for pain in the hip allows you to reduce the load on the vertical axis on the joints.
If you need a stick or cane for more stability, make sure they are right size. If you use your grandfather's cane and it doesn't work for you, you can make your hip pain worse.
The cane must be carried in the hand opposite the affected joint.
Get rid of excess weight. This factor is often underestimated. However, being overweight significantly increases pain in the hip. With each step, body weight places an increased load on the hip. This weight pressure is transferred to the joint. A decrease in body weight by 0.5 kg is equivalent to a decrease in pressure on the thigh by 1-1.5 kg.
Try to identify the source of the pain. If you need to see a doctor for hip pain, be prepared to talk about where you feel pain and when it occurs. You will need to tell your doctor what type of pain is bothering you - whether it is dull or sharp, when it starts and goes away, whether it gets worse with movement or stays the same even at rest, and what movements make you feel worse.
Be patient. If arthritis is suspected, you will have to perform various diagnostic tests because there are over 100 types of arthritis. Be prepared for a bone scan or magnetic resonance imaging. The doctor may also prescribe anti-inflammatory drugs and prescribe heat treatments and ultrasound treatments,
Do a body survey. You may not be aware of your gait disturbances due to spinal curvature or because your leg has become shorter. Take a test that you can do at home. Undress and turn your back to the mirror. Take a mirror in your hand so that you can see yourself from behind over your shoulder. You can ask a family member to examine you. If your knees are on different height, the pelvis will seem to you displaced in one direction or you will notice a curvature of the spine, which means that you have established the causes of your disorders.
Fortunately, gait can be corrected. This can usually be done quite easily. You may need to order a higher boot or have a ready-made instep inserted into it. If you have severe abnormalities, your doctor will refer you to an orthopedist (a specialist who makes special shoes, braces and other devices).
Seek help from surgeons. Typically, hip fractures require special surgical intervention. One of the operations involves preserving the thigh bone and placing a needle inside it for strength. For more complex fractures and even severe arthritis, the surgeon can remove the affected joint and completely replace the damaged bone with a prosthesis.
Remember! Physiotherapy, massage, manual therapy, acupuncture- these are serious methods of treatment that have contraindications, they can only be prescribed by a doctor after an examination! The use of certain methods for purulent inflammation, trauma, or tumors can lead to disability.
According to travmaorto.ru, www.neuronet.ru, www.clinica-voita.ru, www.odalife.ru
We are pleased to present you the first in the Russian-speaking Internet social network supporters of a healthy lifestyle and a full-fledged platform for the exchange of experience and knowledge in everything related to the words "health" and "medicine".
Our task is to create an atmosphere of positive, goodness and health on the site, which will cheer you up, heal and prevent, because information and thoughts are transformed into material events! ;-)
We strive to create a highly moral portal in which it will be pleasant to be the most different people. This is facilitated by, in accordance with which we control the actions of all users. At the same time, we want the site to be sufficiently objective, open and democratic. Here everyone has the right to express their personal opinion, to their own assessment and commenting on any information. In addition, anyone can article, news or any other material in most sections of the site.
Project "Health!" positioned as a portal about health, not about medicine. In our opinion, medicine is the science of how to recover from a particular disease, and health is the result of a lifestyle in which you do not get sick. The more health you have, the less likely you are to get sick. Our bodies are designed in such a way that the right way We don't have to get sick at all. So let's improve our health instead of studying diseases. There are quite a lot of sites about medicine, but in our opinion, they are intended more for medical professionals than for ordinary people. We want to talk to you about health. We do not want to write much about diseases and methods of their treatment - enough has already been written about this. Instead, we will focus your attention on how not to get sick.
We are interested healthy lifestyle life, and we want to live happily ever after. We believe that you are also not indifferent to the topic of healthy longevity. Therefore, if you wish to have an environment healthy people and those who aspire to this, this site will help you solve this problem. Our vision is to create an active community of people leading a healthy lifestyle, and in this regard, we are pleased to offer you the following opportunities:
- create your page with personal photos, blog, forum, calendar and other sections
Do what you like, and we will try to provide you with everything you need for this. We strive to make this site as comfortable as possible for you. There are many new and interesting things ahead.
Register yourself and invite your colleagues, friends and relatives to the site for constant contact with them and exchange of experience. Be always in touch, discussing all the news and interesting things in the field of health.
Stay with us!
