Equipping a massage room in a children's clinic. Toilet of the umbilical wound. Equipment of the vaccination room from the specialists of MedMart LLC
Equipping the vaccination room in children's institution should be carried out in accordance with the order of the Ministry of Health and social development RF No. 366n dated 04/16/2012. This page will help you choose necessary equipment, furniture, tools and materials, without violating the established requirements and norms.
What are the vaccine cabinet standards?
The vaccination room of a childcare institution, like any other institution, requires daily cleaning, decontamination and ventilation. Its equipment includes cleaning equipment, as well as a germicidal lamp, the performance of which must correspond to the size of the room. Among the furniture, the presence of:
- ... doctor's desk;
... medical cabinet;
... changing table;
... couches for carrying out medical and diagnostic measures;
... table nurse;
... at least 2 chairs.
Vaccination room equipment standard for licensing includes hand wash, dispenser liquid soap other hygiene products... Given the focus of the premises, it is necessary to create an appropriate level of safety for children and medical staff. For these purposes, the presence of containers for the disposal of medical waste is provided. The storage of vaccines and thermometers is carried out in the refrigerator, which is also part of the standard for equipping the vaccination room at school, boarding school, baby house and other childcare facilities.
Special attention should be paid to tools and materials. Their list includes disposable syringes with needles, rubber bands, tweezers, heating pads, sterile material beads and much more. You need to understand that the equipment and licensing of the vaccination room must go hand in hand. To obtain official permission, you need to observe not only the list of items, but also their quantity. For example, an office in a child care facility should include 4 kidney-shaped trays, 2 scissors and 5 tweezers.
Equipment of the vaccination room from the specialists of MedMart LLC
With our help, you can quickly, and most importantly, competently prepare premises for further licensing. When collecting inventory, we are guided by the orders, rules and regulations in force in the territory of the Russian Federation. Cooperation with the company "MedMart" will provide an opportunity to select products within each position, adjusting to individual characteristics premises and financial capabilities of the organization.
With "MedMart" equipping any medical office will become simple and straightforward!
Ordering goods for equipping a vaccination room in a child care facility
This page contains all the equipment and tools necessary to equip the vaccination room, prepare the premises for the licensing procedure. To order all the necessary goods, you should:
- 1. Follow the links of all items.
2. Select in each category that opens suitable for cost, type and other characteristics of the product.
3. Add the selected model to the order by clicking the "Add to cart" button located in the product card. After that, the inscription "Added" should appear.
4. Click on the "Trash" icon at the top of the site page.
5. Check the list of all goods, if necessary add additional ones by reopening the catalog or the page of the equipment cabinet.
6. Press the button "Place an order", then form an application by selecting the necessary items and filling in the fields offered by the system.
7. Wait for a call from the online store manager
If any actions on our website caused you any difficulties, call the toll-free number 8 800 500 84 27 on the phone hotline, or order a call using the feedback form.
1. Nurse's desk
2. Chair for a nurse
3. Spiral chair
6. Bedside table
9. The couch is medical
10.Procedural table
12.Sinks;
14. Cleaning equipment:
Floor cleaning bucket
Wall wash bucket
Window cleaning bucket
16. Disinfectants
17. Detergents
Vaccination room documentation
1. Notebook of quartzing cabinet.
2. Notebook of general cleaning
3. Journal of appointments of the vaccination office.
4. Notebook of the account of daily cleaning.
5. Notebook of temperature control in refrigerators.
6. Notebook for recording intravenous blood sampling for biochemical analysis.
7. Notebook of intravenous blood sampling for HbSAg.
8. Notebook for recording intravenous blood sampling for blood group and Rh factor.
9. Notebook of intravenous blood sampling on RW.
10. Notebook for recording intravenous blood sampling for HIV infection.
11. Journal of appointments.
12. Register of prof. vaccinations: DTP, ADS, ADS-m,
13. Register of prof. vaccinations: measles, mumps, rubella.
14. Polio vaccination register.
15. Hepatitis vaccination register.
16. Register of Mantoux reactions.
BCG accounting log., BCG-m.
Varicella vaccination register.
Hemophilus influenza vaccination register.
Medicines (Medicines) of the vaccination room
In the polyclinic, the work with medicines, their accounting, storage and consumption occurs in accordance with the instructions and orders of the Ministry of Health of the RSFSR.
All medicines are divided into three groups: "A", "B" and "General list". According to the method of application, medicines are divided: parenteral, internal and external.
To group "A" relate narcotic and poisonous funds that are kept by the main honey. sisters in a metal safe locked and shot to the floor. On the inner wall of the safe door is a list of narcotic and poisonous agents, their highest daily and single doses.
Everything potent funds include to group "B" , stored in lockers marked: on back wall red letter "B" on a white background. List "B" includes 14 groups of medicines, determined by the mechanism of action:
1. Antibiotics
2. Sulfonamides
3. Some digitalis drugs
4. Analgesics
5. Antispasmodics
6. Hypotensive
7. Sedatives
8. Sleeping pills
9. Hormonal
10. Diuretics
11. Anticonvulsants
12. Antiarrhythmic
13. Stimulating CNS
14. Excitatory respiratory center.
In the cabinets they are arranged according to the mechanism of action, according to the application. Internal drugs are separate from parenteral drugs.
Medicines "general list" are stored in cabinets with the inscription inside: on a white background in black letters "general list".
Parenteral products are stored separately from internal and external medicines are arranged according to the mechanism of action.
Based on order No. 523, all medications must be in original packaging, with a clear name, series and expiration date. Pouring, pouring, re-sticking, transferring from one package to another is prohibited. Coloring, odorous and flammable medicines are stored separately from each other. Medicines requiring protection from light are stored in dark glass containers. Medicines requiring a certain temperature regime stored in the refrigerator.
Disinfectants are stored separately from medicines of all groups.
Dressings, rubber products, medical instruments are stored separately.
Biological products, serums, vaccines are stored in the refrigerator at temperatures from +2 to +8 degrees Celsius.
Subject quantitative accounting subject to alcohol, which is accounted for by the main honey. sisters. In the office, alcohol is issued upon request of inoculated honey. sisters and is written out in a notebook to obtain alcohol.
2.4 To provide emergency care in the office there are special styling to provide assistance in case of emergency conditions:
1. Cardiovascular failure
3. Anaphylactic shock
4. Hyperthermic syndrome.
5. Bronchial asthma.
The volume of work performed in the vaccination room.
In the vaccination room they do
▪ subcutaneous,
▪ intramuscular and
▪ intravenous
jet injection.
The procedures are prescribed either by district pediatricians or by narrow specialists.
After the injection, a record of the manipulation is made in the appointment sheet and in the vaccination journal.
In the vaccination room, on specially designated days, intravenous blood sampling is carried out for research: RW, HIV infection, HbSAg, and biochemical analysis.
2.6 The essence and purpose of immunization.
Immunity - This is the immunological surveillance of the body, its way of protecting against various antigens that carry signs of genetically foreign information.
Penetration (or introduction during vaccination) of microbial or viral antigens causes immune response , which is a highly specific reaction of the body.
the main role in the development of acquired immunity belongs to the cells of the lymphoid system - T - and B-lymphocytes .
Other cell populations and nonspecific defense factors (lysozyme, complement, interferon, properdin, etc.) take part in immune reactions.
Vaccination work
Vaccination work is proceeding according to plan.
There are documents regulating vaccine prophylaxis:
1. the federal law No. 157 of 1998 "On the immunization of infectious diseases."
2. Order No. 9 dated 16.01. 2009 year.
All preventive vaccinations are planned strictly according to the national calendar preventive vaccinations,
The control over the implementation of vaccinations and the timely registration of medical withdrawals is carried out.
2.7.1 Vaccination calendar:
Newborns (in the first 24 hours) - Hepatitis B V1.
4-7 days V BCG (M)
3 months V1 DPT + V1 polio + V2 hepatitis B
4.5 months V2 DPT + V2 polio.
6 months V3 DPT + V3 poliomyelitis. + V3 hepatitis + V1. Hemophilic infection.
7 months V2p hemophilic infection
12 months V measles, V mumps, V rubella.
18 months R1 DTP + R1 poliomyelitis R. hemophilic infection
20 months R2 polio.
24 months V. varicella + V. pneumococcal infection
6 years R measles, R mumps, R rubella
7 years R BCG (carried out by those who are not infected with mycobacterium tuberculosis, tuberculin - to negative children) + R2 ADS-M
13 years V rubella (girls who were not previously vaccinated or received only one vaccine), V (girls) p. Human papilloma virus, V hepatitis (previously not vaccinated)
14 years old R2 BCG (carried out by non-infected with mycobacterium tuberculosis, tuberculin-negative children who have not been vaccinated at the age of 7)
R3 ADS-M, R3 poliomyelitis.
2.7.2 ADDITIONAL INFORMATION on Mantoux Reaction and Viral Hepatitis B.
1. Mantoux reaction every year.
2. Viral hepatitis B:
◦ 1 scheme - 0 -3 months -6 months
Children born to mothers, carriers of the hepatitis B virus or patients with viral hepatitis B in the third trimester of pregnancy, are vaccinated against hepatitis B according to the scheme 0-1-2-12 months.
Vaccination against heratitis B at 13 years old and children after 1 year old is carried out previously unvaccinated
◦ according to 2 scheme 0-1 months-6 months
3. In the absence of BCG, RMantu twice a year.
4. Up to 2 months BCG without Mantoux.
Used in the framework of the national calendar of preventive vaccinations (except for BCG), you can enter simultaneously with different syringes in different parts of the body or with an interval of 1 month.
3. Infection control system, infection safety of patients and medical personnel.
Each medical institution has a system of infection control, which is regulated by orders.
The infection control system includes a set of sanitary and epidemiological measures that reliably prevent the emergence and spread of nosocomial infection.
To prevent infection of patients and medical personnel, a sanitary anti-epidemic regime is strictly observed in the vaccination room, and the rules of both asepsis and antiseptics are strictly observed.
Asepsis - a set of measures aimed at preventing the ingress of microorganisms into the wound during operations, diagnostic and therapeutic procedures.
Antiseptic - a set of measures aimed at limiting and destroying the infection that has entered the wound.
There are methods:
1. Mechanical method ... This is the primary surgical treatment of the edges and bottom of the wound, washing.
2. Physical method - drainage of the wound.
3. Chemical method - the use of hydrogen peroxide, bacteriostatic drugs.
4. Biological method - the use of sera, vaccines, enzymes and antibiotics.
Hand processing.
1. Hands are washed with double soaping, rinsed thoroughly warm water and wiped dry with a clean towel or napkin.
2. Hands are disinfected with 70% ethyl alcohol solution.
3. Hands are treated with skin antiseptics
Tool processing
After use, the instruments pass three stages of processing :
1. Disinfection
2. Pre-sterilization processing
3. Sterilization
Disinfection is a set of measures aimed at destroying pathogenic and opportunistic pathogens.
Definition and etiology
Anaphylaxis is an acute, life-threatening hypersensitivity syndrome. Any drug can cause anaphylaxis.
The most common reasons are:
Insect bites
Medicinal substances(antibiotics, especially penicillins and anesthetics,
It should be noted that there is no dose dependence of anaphylactic shock. The route of administration plays a certain role (intravenous injections are the most dangerous).
Clinic and pathogenesis
The clinical picture of anaphylactic shock is diverse, due to the defeat of a number of organs and body systems. Symptoms usually develop a few minutes after the onset of exposure to the causative factor and peak within 1 hour.
The shorter the interval from the moment the allergen enters the body and until the onset of anaphylaxis, the more severe clinical picture... Highest percentage deaths anaphylactic shock gives when it develops 3-10 minutes after the allergen enters the body.
Symptoms include:
Skin and mucous membranes: urticaria, itching, angioedema.
Respiratory system: stridor, bronchospasm, asphyxia.
The cardiovascular system: acute decrease in blood pressure due to peripheral vasodilation and hypovolemia, tachycardia, myocardial ischemia.
Digestive system: abdominal pain, vomiting, diarrhea.
Convulsive syndrome with loss of consciousness.
It is necessary to differentiate anaphylactic shock from a heart attack (heart attack, arrhythmias), ectopic pregnancy(in a collaptoid state in combination with sharp pains lower abdomen), heat stroke, etc.
Therapy
Treatment is categorized by urgency into primary and secondary interventions.
Primary activities
Epinephrine 0.1% - 0.5 ml / m. Injections are best done in upper part body, such as the deltoid muscle. If there is no reaction, the dose can be repeated after 5 minutes. Intramuscular injections, unlike intravenous ones, are safe. For intravenous administration, 1 ml of 0.1% adrenaline is diluted in 10 ml of saline and injected slowly over 5 minutes (risk of myocardial ischemia). In case of deep shock and clinical death, adrenaline is administered intravenously without dilution.
Passability respiratory tract: suction of secretions, if necessary, enter an air duct. Inhale 100% oxygen at a rate of 10-15 l / min.
Fluid infusion. First, a jet is injected (250-500 ml in 15-30 minutes), then drip. An isotonic sodium chloride solution of 1000 ml is used first, then 400 ml of polyglucin is connected. Though colloidal solutions fill the vascular bed faster, it is safer to start with crystalloid solutions, because dextrans themselves can cause anaphylaxis.
Secondary activities
Prednisolone IV 90-120 mg, repeat every 4 hours as needed.
Diphenhydramine: i / v slowly or i / m at 20-50 mg (2-5 ml of 1% solution). Repeat if necessary after 4-6 hours. Antihistamines are best prescribed after hemodynamic recovery, because they can lower blood pressure.
Bronchodilators. Inhalation of beta 2-agonists using a nebulizer (salbutamol 2.5-5.0 mg, repeat as needed), ipratropium (500 mcg, repeat as needed) may be beneficial in patients treated with beta-blockers. Eufillin (initial dose: IV 6 mg / kg) is used as a reserve drug in patients with bronchospasm. Euphyllin, especially in combination with adrenaline, is capable of provoking arrhythmias, therefore, it is prescribed only if necessary.
Additional activities
Give the patient a horizontal position with raised legs (to increase venous return) and a straightened neck (to restore airway patency).
Remove (if possible) the causative factor (insect sting) or slow down absorption (venous tourniquet above the injection / bite site for 30 minutes, apply ice).
Forecast
About 10% of anaphylactic reactions result in death. Stopping an acute reaction does not mean a successful outcome. Perhaps the development of a second wave of falling blood pressure in 4-8 hours (two-phase flow). All patients after relief of anaphylactic shock should be hospitalized for at least 1 week for observation.
Prophylaxis
Any allergic reaction, even limited urticaria, must be treated to prevent anaphylaxis. Among the latest generation antihistamines, the most effective is claritin, which is applied once a day. Of the complex antiallergic medicines, the drugs of choice are fenistil and clarinase.
Do not get carried away with polypharmacy, observe patients after patient injections for 20-30 minutes. Always take an allergic history.
Medical staff must be specially trained to provide emergency care for anaphylactic shock and to treat similar conditions.
In all vaccination rooms, it is necessary to have a special packing for the relief of anaphylaxis.
ANAPHYLACTIC SHOCK EMERGENCY STYLING
(configuration option)
Epinephrine hydrochloride 0.1% - 1.0 (COLD) 10 ampoules
Atropine sulfate 0.1% - 1.0 (List A, SAFE) 10 ampoules
Glucose 40% - 10.0 10 ampoules
Digoxin 0.025% - 1.0 (List A, SAFE) 10 ampoules
Diphenhydramine 1% - 1.0 10 ampoules
Calcium chloride 10% - 10.0 10 ampoules
Cordiamin 2.0 10 ampoules
Lasix (furosemide) 20 mg - 2.0 10 ampoules
Mezaton 1% - 1.0 10 ampoules
Sodium chloride 0.9% - 10.0 10 ampoules
Sodium chloride 0.9% - 400.0 ml / or 250.0 ml 1 bottle / or 2 bottles
Polyglyukin 400.0 1 bottle
Prednisolone 25 or 30 mg - 1.0 10 ampoules
Tavegil 2.0 5 ampoules
Euphyllin 2.4% - 10.0 10 ampoules
System for intravenous drip infusion 2 pcs.
Disposable syringes 5.0; 10.0; 20.0 x 5
Disposable alcohol wipes 1 pack
Rubber harness 1 pc.
Rubber gloves 2 pairs
Ice pack (COLD) 1 pc.
ALGORITHM OF ACTIONS
1. Stop the injection of the drug that caused the shock, if the needle is in the vein, do not remove it and carry out the therapy through this needle; in case of a Hymenoptera bite, remove the sting.
2. Mark the time when the allergen enters the body, the appearance of complaints and the first clinical manifestations allergic reaction.
3.Place the patient with raised lower limbs, turn your head to the side, push forward lower jaw to prevent tongue retraction and aspiration of vomit. Remove existing dentures.
4. Assess the patient's condition, complaints. Measure your pulse arterial pressure(BP), temperature. Assess the nature of shortness of breath, the prevalence of cyanosis. Inspect the skin and mucous membranes. With a decrease in blood pressure by 20% of the age norm - suspect the development of an anaphylactic reaction.
5.Provide access fresh air or give oxygen.
6. Apply a tourniquet above the injection of the drug, if possible (every 10 minutes, loosen the tourniquet for 1 min, total time application of a tourniquet for no more than 25 minutes).
7. Place an ice pack over the injection site.
8. All injections must be made with syringes and systems that have not been used for the administration of other medications, in order to avoid repeated anaphylactic shock.
9. When injecting an allergic drug into the nose or eyes, rinse them with water and drip a 0.1% solution of epinephrine 1 - 2 drops.
10. With the subcutaneous injection of the drug that caused the shock, prick the injection site crosswise with 0.3 - 0.5 ml of 0.1% adrenaline solution (dilute 1 ml of 0.1% adrenaline solution in 3 - 5 ml of saline).
11. Prepare the intravenous system with 400 ml of saline prior to the arrival of the doctor.
12. At the command of the doctor, slowly inject 1 ml of 0.1% solution of adrenaline diluted in 10-20 ml of saline. If the puncture of the peripheral vein is difficult, adrenaline injection into soft tissue sublingual area.
13. Introduce intravenous stream, and then drip glucocorticosteroids (90-120 mg of prednisolone).
14. Introduce a solution of diphenhydramine 1% at a dose of 2.0 ml or a solution of tavegil 2.0 ml intramuscularly.
15. In case of bronchospasm, inject intravenous aminophylline 2.4% - 5-10 ml.
16. When breathing is weakened, enter s / c cordiamine 25% - 2.0 ml.
17. In case of bradycardia, enter s / c atropine sulfate 0.1% - 0.5 ml.
9. APPENDIX 2 Job description vaccination office nurse:
9.1.1 I. General Provisions
TO professional activity as honey. sisters of the vaccination room, a nurse with at least three years of hospital work experience, having a qualification category, a certificate in the specialty "Nursing in Pediatrics" and trained in the workplace, is allowed.
Appointment and dismissal of honey. sisters of the vaccination room is carried out by the head physician on the proposal of the head. department, senior med. sister of the department and in agreement with the chief medical officer. sister of the hospital.
Honey. the nurse of the treatment room is directly subordinate to the head of the clinic and the chief medical officer. sisters.
9.1.2 II. Duties
The nurse checks the number of vaccine vials per workday, monitors the temperature in the refrigerator, and notes the readings in a journal. The nurse conducts psychological preparation the child to be vaccinated. In the history of development, it records the doctor's admission to vaccination, the intervals between vaccinations and their compliance with the individual vaccination schedule. Registers the vaccination in the card of preventive vaccinations (f. No. 063 / y), the register of preventive vaccinations (f. No. 064 / u) and in the history of the child's development (f. No. 112 / u) or in the individual card of the child (f. No. 026 / y). Carries out vaccinations and gives advice to parents on caring for a child.
The nurse receives vaccinations, medicines. Responsible for the use and rejection of bacterial preparations. Complies with the rules for storing vaccines during immunization and the rules for handling the vaccine instrument. Responsible for the sanitary and hygienic regime of the vaccination room.
During the working day, the nurse destroys all remaining vaccine in open vials, records the amount of vaccine used and sums up (the number of doses remaining) in the register, checks and records the temperature of the refrigerators.
The nurse prepares a vaccination report every month.
1. Organization of work in accordance with this instruction, hourly work schedule.
2. Organization of the vaccination room in accordance with the standard.
3. Compliance with the requirements for marking items medical purpose.
4. Clear and timely management medical records. Timely submission a report on the performed manipulations for a month, half a year, a year.
5. Preparation of the office for work.
6. Perfect knowledge of the methods of carrying out preventive, therapeutic, diagnostic, sanitary and hygienic procedures, manipulations and their high-quality, modern implementation.
7. Strict adherence to the technology of taking blood for all types of laboratory tests.
8. Timely and correct transportation of the test material to laboratory departments.
9. Timely message to the attending physician about complications from the manipulation, about the patient's refusal to carry out the manipulation.
10. Ensuring the availability and completeness of the first aid kit for the provision of emergency care, the provision of emergency first aid.
11. Monitoring the sterility of the received material and medical instruments, compliance with the shelf life of sterile products.
12. Regular and timely passage of honey. examination, examination for RW, HbSAg, HIV - infection, carriage of pathogenic staphylococcus.
13. Ensuring proper order and sanitary condition of the vaccination room.
14. Timely discharge and receipt from the main honey. sisters necessary for the work of medicines, tools, systems, alcohol, honey. tools, medical items. destination.
15. Ensuring the correct accounting, storage and use of medicines, alcohol, honey. tools, medical items. destination.
16. Carrying out a dignity. enlightenment work on health promotion and disease prevention, advocacy healthy way life.
17. Constant increase professional level knowledge, skills and abilities. Timely completion of the improvement.
9.1.3 III. Rights
1. Receiving necessary information for the clear fulfillment of professional duties.
2. Making proposals to the management to improve the work of honey. sisters of the vaccination room and the organization of nursing in the clinic.
3. Requirements from the main m / s of timely provision of medicines necessary for work, honey. tools, forms.
4. Requirement of the senior m / s to provide timely vaccines;
5. Requirement from the hostess sister to timely provide the necessary soft and hard utensils, disinfectants, detergents and cleaning agents.
6. Improving your qualifications in the prescribed manner, passing certification, recertification in order to assign a qualification category.
7. Participation in the public life of the clinic.
9.1.4 IV. A responsibility
The nurse of the vaccination room for non-fulfillment of her professional duties, accounting, storage and use of medicines is responsible under the current legislation.
Your gender
1.man
2. female
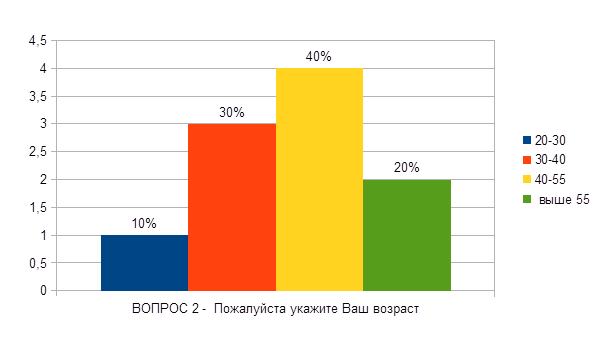
1. 20 -30
2. 30-40
3. 40-55
Above 55
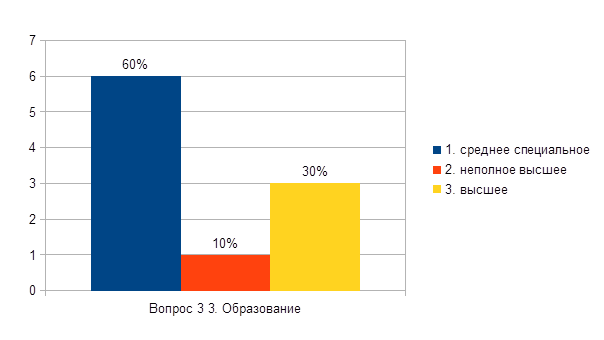
Education
1.secondary special
2.incomplete higher education
4. Please indicate how many years have you devoted to medicine (work experience)?
1.5 or less
2.there is the first
3. there is a higher
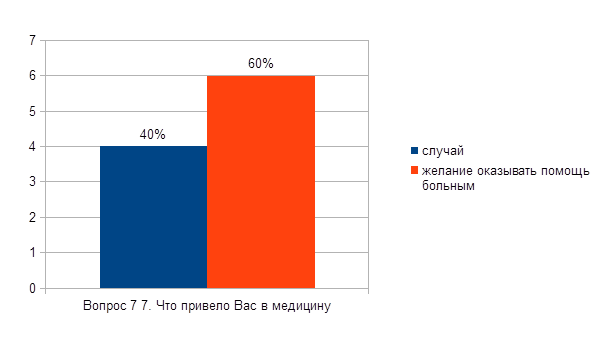
What brought you to medicine
2. desire to help the sick
APPENDIX 4 Table of answers to the Questionnaire.
| Question number | Answer number | Answer number - 2 | Answer number | Answer number | Answer number |
| 1. | |||||
| 2. | |||||
| 3. | |||||
| 4. | |||||
| 5. | |||||
| 6. | |||||
| 7. | |||||
| 8. | |||||
| 9. | |||||
| 10. | |||||
| 11. | |||||
| 12. | |||||
| 13. | |||||
| 14. | |||||
| 15. | |||||
| 16. | |||||
| 17. | |||||
| 18. | |||||
| 19. | |||||
| 20. |
Your gender
1.man
2.women
1. 20 -30
2. 30-40
3. 40-55
4. above 55
Education
1. specialized secondary
2. incomplete higher
3. higher
What brought you to medicine
2.the desire to help the sick
References - sites
1.https://ru.wikipedia.org/wiki/
2.http: //www.homfo.ru/stat/neotlozhnaya_pomosch/
List of abbreviations
I. WHO
The World Health Organization dates back to 7 April 1948 at WHO headquarters in Geneva.
II. BCG
BCG (Bacillus Calmette-Guérin or Bacillus Calmette-Guérin, BCG) is a tuberculosis vaccine prepared from a strain of a weakened live bovine tuberculosis bacillus (lat.Mycobacterium bovis BCG), which has practically lost its virulence for humans, being specially grown in an artificial environment.
III. DTP
DTP (international abbreviation DTP) is a combination vaccine against diphtheria, tetanus and pertussis.
IV. HbSAg
Hepatitis B virus is a DNA-containing virus from the hepadnavirus family, the causative agent of viral hepatitis B. According to various estimates, from 3 to 6% of people in the world are infected with the hepatitis B virus. Carriage of the virus is not necessarily accompanied by hepatitis
Vii. Hiv
Human immunodeficiency virus - a retrovirus from the genus of lentiviruses that causes a slowly progressive disease - HIV infection
VIII. AIDS
Acquired Immune Deficiency Syndrome (AIDS) is a condition that develops against the background of HIV infection and is characterized by a drop in the number of CD4 + lymphocytes, multiple opportunistic infections, non-infectious and neoplastic diseases. AIDS is the final stage of HIV infection.
IX. Mantoux test
A research method that evaluates the body's response to the ingestion of the antigen of the tuberculosis pathogen. In addition, the Mantoux reaction is used to confirm the diagnosis of tuberculosis and as a control analysis in assessing the effectiveness of treatment.
X. Ministry of Health of the RSFSR.
MINISTRY OF HEALTH OF THE RSFSR
Glossary
II. Polyclinic
A highly developed specialized medical and preventive institution providing mass species medical care(for the prevention and treatment of diseases) to the population living in the territory of its activity.
Immunoprophylaxis
III. Disinfection
Disinfection is a set of measures aimed at destroying pathogens infectious diseases and destruction of toxins on objects of the external environment.
IV. Sterilization
Sterilization (microbiology) - complete release various substances, items, food products from living microorganisms.
V. Immunity
Immunity (Latin immunitas - liberation, getting rid of something) is the ability immune system rid the body of genetically foreign objects.
Vi. Immune response
The immune response is a complex multicomponent, cooperative response of the body's immune system, induced by an antigen and aimed at its elimination. The phenomenon of the immune response underlies immunity.
Equipping the vaccination room with solid equipment
1. Nurse's desk
2. Chair for a nurse
3. Spiral chair
4. Medical cabinet for sterile solutions and medicines
5. Instrument tables for preparing and carrying out procedures;
6. Bedside table
7. 2 refrigerators for storing vaccines;
3. Refrigerator for storing medicines;
9. The couch is medical
10.Procedural table
11.Medicine cabinet for emergency and syndromic aid
12.Sinks;
13.Dust bin (bucket enameled with a lid)
14. Cleaning equipment:
Floor cleaning bucket
Wall wash bucket
Window cleaning bucket
Tank for washing heating devices
15. Apparatus for irrigation des. means (general cleaning)
16. Disinfectants
17. Detergents
INSTRUCTION No. 1
1. GENERAL INFORMATION
2. EQUIPMENT
2.1. Medical furniture:
the couch is medical;
changing table;
a table for a nurse;
medical chair;
2.2. Hygrometers.
2.5. Medicines in ampoules (vials).
injection needles;
syringes with needles;
gauze napkins;
balls of cotton and gauze;
self-adhesive bandages.
medical bandages;
medical adhesive plaster.
2.12. Other medical devices:
venous tourniquet;
sterilization boxes;
racks for test tubes.
tonometer with a phonendoscope;
the mouth dilator is sterile;
sterile tongue holder;
glasses or protective shield.
INSTRUCTION No. 2
INSTRUCTION No. 3
WORKPLACE PREPARATION
INSTRUCTION No. 4
SECONDARY NEWBORN HANDLING,
INSTRUCTION No. 5
BABY TOILET
1. GENERAL INFORMATION
The toilet of the newborn is performed twice a day (in the morning before the first feeding and in the evening). The toilet of a newborn includes care for the skin, mucous membranes, and the umbilical cord (umbilical wound). During morning toilet the newborn is weighed and the body temperature is measured. The nurse is obliged to explain to the mother the purpose of the manipulation, to teach and monitor the correctness of the execution.
2. EQUIPMENT
2.1. Medical furniture and equipment:
changing table with heating;
manipulation table (mobile if necessary);
a table for carrying out disinfection measures;
crib for a newborn;
radiating heater.
2.2. LS (individual spill):
sterile vaseline oil;
2.4. Reusable sterile medical instruments:
2.5. Sterile dressing:
cotton balls;
cotton swabs.
2.6. Other medical devices:
diapers are sterile;
disposable diapers.
CO - medical gown, medical cap;
gloves;
apron.
2.8. Containers:
"No. 3" or "Physical method. Dressing";
"No. 4" or "Physical method. Gloves".
2.9. Capacity "Packaging".
2.10. Sanitary and hygienic products:
towel.
2.11. Sanitary equipment:
wash basin;
pedal bucket;
diaper capacity.
3. PERFORMANCE TECHNIQUE
PREPARATORY STAGE
3.1. Wash and dry your hands.
3.3. Disinfect apron, surfaces of manipulation tables, changing table, scales. If there is an additional "non-sterile" changing table to free the child from dirty diapers, disinfect his work surface.
individual packaging with sterile material - cotton balls, cotton swabs;
sterile vaseline oil;
sterile water (sodium chloride solution 0.9% sterile);
hydrogen peroxide solution 3%;
potassium permanganate solution 5%;
3.6. Inform the mother of the child about the upcoming manipulation.
3.7. Switch on the radiant heater.
3.9. Check the sterilization date of the diapers, open the sterile bag, spread the diapers on the changing table. Lay out the diaper to dry the skin.
3.10. Open a tap with water and adjust its temperature.
MAIN STAGE
3.11. Remove the medallion. Unwrap the baby in the crib (or on the "non-sterile" changing table). Unfold the inner diaper without touching the baby's skin.
3.12. Before contact with skin and the mucous membranes of the child to carry out hygienic antiseptics of the skin of the hands.
3.13. Verify the text of the medallion and bracelets.
3.14. Take a child in accordance with subparagraph 3.17. Instructions # 4. Boys with a small body weight can be taken out of the crib in another way: with the 1st finger and palm, cover the shoulder girdle and chest front and sides; With the 2nd, 3rd, 4th and 5th fingers of the hand, grasp the chest from behind. Turn the child face down. In this case, the newborn lies with the front surface of the body across the lower third of the nurse's forearm.
3.15. Wash the child under running water. Girls are washed from front to back to avoid contamination and infection of the urinary tract. Boys are washed from the buttocks to the crotch.
3.17. Place the diaper in the pedal bucket, wet diaper and diapers left in the crib (or on the "non-sterile" table) in the "Diaper" container.
3.18. Conduct hygienic hand antiseptic. Wear gloves.
3.19. Carry out the toilet of the umbilical cord ( umbilical wound) in accordance with Instruction No. 5.1. (No. 5.2.).
3.20. Process:
eyes in one movement from the outer corner to the bridge of the nose by separate cotton balls moistened with sterile water (sodium chloride solution of 0.9% sterile);
if necessary, the nasal passages with flagella moistened with sterile vaseline oil (sodium chloride solution of 0.9% sterile). The right and left nasal passages are cleaned by rotating movements alternately with separate flagella. Depth of flagella insertion 1 - 1.5 cm;
face with a cotton ball with sterile water (sodium chloride solution of 0.9% sterile). Carry out the processing in the following sequence: forehead, cheeks and, last but not least, the skin around the mouth;
in a child with a sexual crisis, the external genitals with a cotton ball with sterile water (sodium chloride solution of 0.9% sterile);
folds of skin symmetrically from top to bottom with a cotton ball with vaseline oil. A cotton ball is held in hand during processing. Use one ball to process the folds of the upper half of the body, with the other - the folds of the lower half of the body. Last but not least, the third ball, groin folds from top to bottom and intergluteal region from bottom to top .
3.21. Put on a diaper, swaddle a baby, put on a medallion.
3.22. Disinfect the surface of the crib mattress.
3.23. Cover the mattress with a diaper.
3.24. Place the baby in the crib.
THE FINAL STAGE
3.25. Disinfect the surface of the changing table and apron after each child's toilet.
3.26. Remove gloves, place them in container # 4 or "Physical method. Gloves".
3.27. Wash and dry your hands.
INSTRUCTION No. 5.1
TOILET OF UMBRELLA
1. EQUIPMENT
2. PERFORMANCE TECHNIQUE
PREPARATORY STAGE
MAIN STAGE
2.3. To raise umbilical cord up, grasping the plastic clip with your hand.
2.4. With a juicy residue, treat the cut with a sterile stick with cotton wool moistened with an alcohol-containing antiseptic, as the most likely entrance gate of infection, then in a circular motion the entire remainder from top to bottom towards the base. Process the mummified residue from the base - the area of the upcoming rejection, from the bottom up.
2.5. After treating the remainder with the same stick, treat the skin around it from the center to the periphery.
2.6. With another sterile stick with cotton wool, moistened with a solution of potassium permanganate 5%, treat the umbilical cord residue in the same sequence, without touching the skin of the abdomen. Place the used sticks in container "No. 3" or in container "Physical method. Dressing".
THE FINAL STAGE
See subclauses 3.21.-3.27. Instructions # 5.
INSTRUCTION No. 5.2
TOILET OF THE UMBRELLA
(fragment of a newborn's toilet)
1. EQUIPMENT
1.1. Prepare equipment in accordance with subparagraphs 2.1.-2.11. Instructions # 5.
2. PERFORMANCE TECHNIQUE
PREPARATORY STAGE
2.1. Spend preparatory stage according to subparagraphs 3.1.-3.10. Instructions # 5.
MAIN STAGE
2.2. Conduct hygienic hand antiseptic, wear gloves.
2.3. Use your hand to separate the edges of the umbilical ring.
2.4. Liberally cover the umbilical wound with a 3% hydrogen peroxide solution using a dropper on the bottle (a sterile pipette or a cotton swab taken with sterile tweezers).
2.5. After 20-30 sec. dry the wound by extinguishing it with a sterile cotton swab.
2.6. Treat with a sterile cotton swab moistened with a solution of potassium permanganate 5%, only the wound, without touching the skin. Place the used sticks in container "No. 3" or in container "Physical method. Dressing".
THE FINAL STAGE
See subclauses 3.21.-3.27. Instructions # 5. When using a pipette, carry out disinfection measures in accordance with subparagraph 3.4. Instructions # 2.
INSTRUCTION No. 6
Swaddling a newborn
(in obstetric care)
1. GENERAL INFORMATION
In the obstetric facility, swaddling is done before each feed using sterile underwear. For newborns, clean home clothes, linen and disposable diapers.
There are several options for swaddling. Their choice depends on the maturity of the newborn baby.
2. EQUIPMENT
2.1. Prepare equipment in accordance with subparagraphs 2.1., 2.6.-2.11. Instructions # 5.
3. PERFORMANCE TECHNIQUE
PREPARATORY STAGE
3.1. Wash and dry your hands.
3.2. Put on an apron, gloves.
3.3. Disinfect the apron, the surfaces of the manipulation table, the changing mattress. If there is an additional "non-sterile" changing table to free the child from dirty diapers, disinfect his work surface.
3.4. Remove gloves, place in container # 4 or “Physical method. Gloves".
3.5. Turn on the heating lamp.
3.6. Open a tap with water and adjust its temperature.
3.7. Inform the mother of the child about the necessity and essence of the procedure.
3.8. Conduct hygienic hand antiseptic.
3.9. Check the sterilization date of the diapers, open the sterile diaper bag.
3.10. Spread 4 diapers on the changing table: 1st flannel; Fold the 2nd chintz diaper diagonally and fold it upwards above the level of the first diaper by 15 cm (for making a headscarf) or fold it in half along its length and put it above the level of the 1st diaper for making a "hat"; 3rd cotton diaper; Fold the 4th diaper-diaper (made of soft flannel) in four with a long rectangle; disposable diapers can be used instead. Lay out the diaper to dry the skin.
In case of insufficient air temperature in the ward, an additional 1-2 diapers are used, folded in four and placed in a "diamond" after the 2nd or 3rd diaper.
To make a "hat", the folded edge of the diaper must be tucked backward by 15 cm. Fold the upper corners of the diaper, joining them in the center. Fold the bottom edge several times up to the bottom edge of the "cap". Place at the level of the top edge of the 1st diaper.
MAIN STAGE
3.11. Remove the medallion.
3.12. Unwrap the baby in the crib (or on the "non-sterile" changing table). Unfold the inner diaper without touching the baby's skin.
3.13. Before contact with the skin of the child, conduct hygienic antiseptics of the skin of the hands.
3.14. Verify the text of the medallion and bracelets.
3.15. Wash the child under running water if necessary.
3.16. Dry the baby's skin with a sterile diaper, first on the weight, then again on the changing table.
3.17. Place the wet diaper and the diapers left in the crib (or on the "non-sterile" table) in the "Diaper" container, the diaper in the pedal bucket.
3.18. Conduct hygienic hand antiseptic.
3.19. Place the 4th diaper (diaper) between the baby's legs, place its upper edge in the underarm area on one side or fix the disposable diaper.
3.20. With the edge of the 3rd diaper on the same side, cover and fix the shoulder, the front of the child's torso and the axillary region on the other side. If a disposable diaper was used, place the bottom corner of the diaper between the newborn's torso and arms. Cover and fix the second shoulder of the child with the opposite upper edge of the diaper. Separate the feet from one another with its lower edge. Loosely roll the excess diaper underneath and place it between the baby's feet.
3.21. Put on a “hat” or headscarf made from the 2nd diaper.
3.22. Fix all the previous layers and the "hat" (kerchief) with the 1st diaper. Wrap the lower end of it up and circle it around the child's torso 3-4 cm below the nipples and fasten it on the side, tucking the corner of the diaper over its taut edge.
3.23. Put on the medallion.
THE FINAL STAGE
See subclauses 3.22.-3.27. Instructions # 5.
INSTRUCTION No. 7
INSTRUCTION No. 8
INSTRUCTION No. 9
Capacity "Packaging".
2.11. Sanitary and hygienic products:
wall-mounted elbow dispenser with antiseptic;
wall-mounted dispenser with liquid pH-neutral soap;
towel.
2.12. Sanitary equipment:
wash basin;
pedal bucket;
diaper capacity.
3. PERFORMANCE TECHNIQUE
PREPARATORY STAGE
3.1. Wash and dry your hands.
3.2. Put on an apron, gloves.
3.3. Disinfect the apron, the surfaces of the manipulation tables, the changing table.
3.4. Remove gloves, place in container # 4 or “Physical method. Gloves".
3.5. Prepare a manipulation table (mobile if necessary):
3.5.1. place on the top shelf:
packaging with sterile material - cotton balls;
sterile tweezers (if necessary);
vaseline oil;
cosmetics skin care;
boiled water(sterile water, sodium chloride solution 0.9%);
nasal aspirators;
Check the sterility of the packages and the expiration date of the medicinal products.
3.5.2. place equipment on the bottom shelf in accordance with subparagraph 3.12.2 (3.13.2) of Instruction No. 3.
3.6. Inform the mother of the child (legal representative) about the necessity and essence of performing the manipulation.
3.7. Spread the diaper on the changing table, prepare the clothes. Lay out the diaper for drying the skin, the diaper.
MAIN STAGE
3.8. Conduct hygienic hand antiseptic.
3.9. Undress the baby in the crib, remove the diaper, roll it up and throw it into the pedal bucket.
3.10. Wash the baby with running warm water, preferably using baby liquid cleansers. The girl is washed strictly from front to back.
3.11. Dry the skin with blotting movements, first on the weight, and then on the changing table, thoroughly blotting the gluteal, inguinal and popliteal folds.
3.12. Place a wet diaper, contaminated clothing in the "Diaper" container.
3.13. Conduct hygienic hand antiseptic, wear gloves.
3.14. Process:
eyes in one movement from the outer corner to the bridge of the nose with separate cotton balls moistened with boiled water (sterile water);
if necessary, the nasal passages with flagella moistened with vaseline oil (sterile water, 0.9% sodium chloride solution);
face with a cotton ball with boiled water (sterile water). If necessary, dry your face with a dry ball;
folds of skin with cotton balls with a moisturizing baby cream (other skin care products) in the sequence in accordance with subparagraph 3.22. Instructions # 4. The ball is held in the hand during processing. If necessary, apply a special protective baby cream under the diaper.
3.15. Put on a diaper.
THE FINAL STAGE
3.16. Dress up the child.
3.17. Place the baby in the crib.
3.18. Disinfect the surface of the changing table, apron after each child's toilet.
3.19. Remove gloves and place them in container # 4 or "Physical method. Gloves".
3.20. Wash and dry your hands.
INSTRUCTION No. 10
INSTRUCTION No. 1
EQUIPMENT AND PREPARATION FOR WORK
PEDIATRIC DEPARTMENT PROCEDURE ROOM
1. GENERAL INFORMATION
The treatment room of a healthcare organization must comply with the requirements of technical regulatory legal acts (hereinafter - TNLA) and include the following premises:
for taking blood from a vein for biochemical and other studies, performing intravenous injections, preparing for intravenous infusions;
to perform intradermal, subcutaneous and intramuscular injections;
for patient registration and medical records.
In the treatment room, the current daily and general cleaning followed by disinfection of the air in accordance with the requirements of the TNLA.
Each medical worker must be provided with personal protective equipment (hereinafter PPE), including sanitary clothing (hereinafter CI). PPE used in health care organizations must comply with the TNLA requirements for the relevant categories of medical devices (hereinafter MP).
Keeping personal and sanitary clothes medical workers in healthcare organizations should be held separately in isolated sections of individual two-section cabinets (one for storing personal clothes, things, shoes; the other for CO, removable shoes).
Before the start of the work shift, the healthcare professional must remove outerwear, shoes and place in a closet, remove from hands Jewelry, wash and dry hands, put on CO and change shoes.
2. EQUIPMENT
2.1. Medical furniture:
the couch is medical;
changing table;
manipulation table for preparing and performing injections and intravenous infusions;
a mobile manipulation table for preparing and performing injections and intravenous infusions outside the treatment room;
table for intravenous injection;
a table for carrying out disinfection measures;
a table for a nurse;
medical chair;
medical cabinet for storing medicines (hereinafter MP) and medical devices;
metal cabinet for storing drugs of the list "A", drugs and psychotropic substances.
2.2. Hygrometers.
2.3. Devices for disinfection of indoor air.
2.4. Radiant warmer for newborns "Radiant warmth"
2.5. Medicines in ampoules (vials).
2.6. Sterile water for injection, sodium chloride solution 0.9% and others in ampoules (vials) for the preparation of drug solutions.
2.7. Sterile disposable medical instruments:
injection needles;
syringes with needles;
infusion and transfusion systems;
vacuum systems for taking venous blood;
peripheral venous catheters.
2.8. Reusable sterile medical instruments:
2.9. Medical instruments, non-sterile, reusable:
2.10. Sterile dressing:
gauze napkins;
balls of cotton and gauze;
self-adhesive bandages.
2.11. Non-sterile dressing material:
medical bandages;
medical adhesive plaster.
2.12. Other medical devices:
tags (stickers) for marking containers and containers, bags for medical waste and bags for other purposes (hereinafter tags (stickers));
treatment roller or cushion for venipuncture;
venous tourniquet;
sterile disposable plugs for peripheral venous catheters;
sterile infusion guides for single use;
container for heating oil solutions of drugs in ampoules;
thermometer for measuring the temperature of water in the tank;
measuring container for concentrate dosing chemical agent disinfection;
containers for transporting samples of biological material;
sterilization boxes;
coarse calico napkins (diapers) sterile;
clean coarse calico napkins for a tourniquet;
disposable coarse calico or gauze napkins or disinfected for surface treatment (hereinafter referred to as surface treatment napkins);
disposable tubes with stoppers;
ampoule knife and other instrument for opening ampoules and vials;
disposable bags for packaging medical waste (hereinafter, bags for medical waste);
disposable bags for collecting CO and laundry contaminated biological material(hereinafter, bags for collecting CO and linen);
medical stands for intravenous infusion;
racks for test tubes.
2.13. Medical devices and drugs for the provision of emergency medical care:
a device for manual ventilation of the lungs (Ambu bag) included;
sterile disposable air duct (set);
medical electric aspirator;
tonometer with a phonendoscope;
the mouth dilator is sterile;
sterile tongue holder;
drug kits completed in accordance with the TNLA:
for ambulance;
for medical assistance in case of emergency contact with the patient's biological material;
for medical assistance in case of poisoning with a chemical disinfectant.
CO - medical gown, medical cap;
protective gloves, sterile gloves;
medical mask or respirator;
glasses or protective shield.
2.15. Antiseptic, including alcohol-based for the treatment of the injection field (hereinafter antiseptic).
2.16. Chemical disinfectants:
chemical agent for emergency disinfection for ampoules (vials), external surfaces of medical devices (changing table, manipulation table, medical couch, etc.);
a concentrate of a chemical disinfectant;
working solution of a chemical disinfectant (not having a fixing effect) in a container for washing and disinfecting medical devices, disinfecting the external surfaces of medical devices.
2.17. Containers (containers) for carrying out disinfection measures (with a perforated tray, oppression and a lid) marked:
"No. 1" - for washing syringes and other medical devices in a working solution of a chemical disinfectant (hereinafter - container "No. 1");
"No. 2" - for disinfection in a working solution of a chemical disinfection agent for the duration of exposure of syringes and other medical devices to be processed (hereinafter container "No. 2");
"No. 3" - for disinfection in a working solution of a chemical disinfection agent for the duration of exposure of dressings, PPE (except gloves) and other medical devices to be destroyed (hereinafter container "No. 3");
"No. 4" - for disinfection in a working solution of a chemical disinfection agent for the duration of exposure of gloves (hereinafter container "No. 4").
2.18. A non-puncture-proof container with a lid with a disposable needle cutter, marked "Sharp medical devices" for collecting and disinfecting injection needles, syringes with an integrated (sealed) needle and other sharp medical devices (hereinafter the container "Acute medical devices").
2.19. Containers (containers) with lids, marked "Physical method" indicating the name of the medical device for the separate collection of syringes, dressings, gloves and other medical devices when used in a healthcare organization physical method disinfection (hereinafter containers "Physical method").
2.20. A non-puncture-proof container (container) marked "Empty ampoules and vials of drugs" for collecting empty ampoules and vials of drugs (hereinafter the container "Empty ampoules and vials of drugs").
2.21. Container (container) marked "Plastic" for collecting plastic products that are not contaminated with biological material (hereinafter the container "Plastic").
