Knee arthritis: pain that can be relieved. Knee pain: causes and how to eliminate
Among all forms of articular pathology, osteoarthritis of the knee joint occupies a special place, the treatment of which is one of the central problems not only of rheumatology, but of the whole modern medicine... This is due to the wide spread of the disease and an objective risk severe complications, up to the disability of patients.
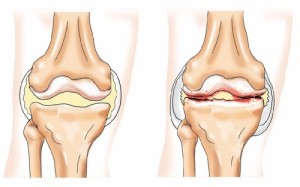
The disease is marked by damage to the cartilage tissue of the knee due to an imbalance in the process of its renewal. Natural recovery ceases to compensate for the course of tissue destruction, as a result of which the cartilage becomes thinner and does not perform its function in the required volume. (the second name of the disease) is an organ pathology. The entire joint is involved. His condition is characterized by progressive stiffness and deformity.
How to notice this disease?
Morning stiffness in knee joint may indicate the beginning of the development of osteoarthritis
Pain is the leading symptom of the disease. It is she who determines the patient's appeal to the doctor and is the main cause of disability. At the same time, there is no clear correlation between the severity of pain and various destructive changes.
Another important sign a disease that can sometimes be more indicative of pain is a limitation of the mobility of the affected knee. Morning limb stiffness can be up to 30 minutes. With the development of the disease, this symptom is fixed and gains regular stability.
An additional sign of gonarthrosis is characteristic (crepitus). Not those light clicks that occur with healthy people, but a rough crunch that accompanies the movement of diseased joints.
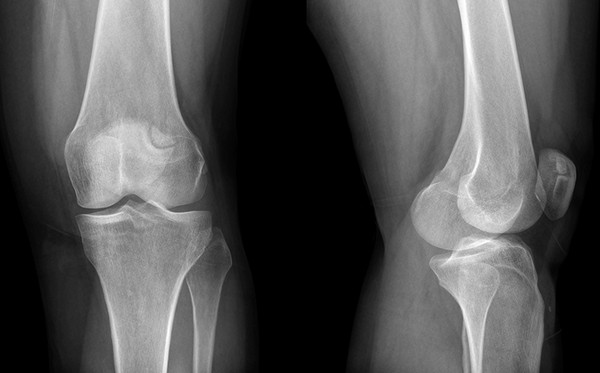
X-ray examination shows the presence of bone growths in the joint - osteophytes, which are formed at a certain stage of the disease. There are four such stages, when pathologies are recorded on the roentgenogram:
- questionable changes in the joint;
- minimal changes, narrowing of the joint space;
- moderate distinct changes;
- severe pathology.
Treatment of osteoarthritis of the knee
In deforming osteoarthritis of the knee joint, the treatment regimen is determined by several basic principles:
- reduction of pain syndrome;
- improving joint function;
- preventing the development of disability.
Besides, great attention paid educational work with the sick. The patient's ability to live with arthritic pain, correctly use the load on the joints, and correctly apply medications are important components successful treatment and improving the quality of life.
Pain relief
An important goal in the treatment of osteoarthritis of the knee is to minimize the use of drugs with side effects.
To reduce pain in gonarthrosis, there is a large number of methods, but the use of non-steroidal anti-inflammatory drugs is of primary importance. Standard preparations are widely known: aspirin, diclofenac, ibuprofen, piroxicam, etc. They are good at suppressing inflammatory and pain reactions, but they can cause side effects a wide spectrum: from gastrointestinal to platelet. Therefore, when prescribing these funds, clinical and laboratory monitoring is mandatory.
An important goal of treatment is to minimize the use of drugs with undesirable effects. In this regard, their use is combined with local therapy. The use of non-steroidal drugs in the form of creams, gels can significantly reduce pain and reduce the need for oral administration of the drug. This is important aspect long-term treatment... However, anti-inflammatory drugs only remove the main symptoms - pain and inflammation, but they do not cure the disease itself. If limited only to them, the disease will progress to its most severe stage.
Intra-articular treatment
Knee osteoarthritis requires systemic treatment drugs that slow the progression of the disease. They should be taken for a long time. These are symptomatically delayed action drugs. The effect of their use develops after a few months from the start of admission. However, their effect continues. for a long time and after drug withdrawal.
We are talking about chondroprotectors - drugs that feed the articular cartilage and prevent its destruction. These include: chondroitin sulfate (Structum), glucosamine sulfate (Dona) and combined meanssuch as Teraflex or Artra. These disease-modifying drugs are selected by the physician individually for each patient. They help especially well in the first and second stages of the disease.
Hyaluronic acid preparations are widely used in the treatment of gonarthrosis. They belong to non-drug therapy, since they do not have a systemic effect. In fact, these are synovial fluid prostheses. They replace it in the affected joint. This reduces pain and significantly improves joint mobility. The effect can last up to 8 months. Drugs are injected into the joint, 3-5 injections with a weekly interval.
IN critical stage diseases when the function of the joint is lost in a very to a large extent, and pain syndromes are not amenable to relief traditional means, apply surgical techniques treatment. The problem is solved by joint replacement. The damaged surfaces are replaced with a biocompatible prosthesis, which allows painless, smooth knee movement.
Currently, osteoarthritis of the knee joint has good prospects for treatment without cardinal surgery. By creating new drugs that affect various processes of the pathogenesis of the disease. And the spectrum medicines, to get rid of this heavy suffering, is steadily expanding.
Osteoarthritis of the knee joint, like other types of arthrosis, is best treated if started early. The success of treatment depends on the correct diagnosis, and the symptoms of arthrosis of the knee joint are sometimes mistaken for symptoms of other diseases. Even a specialist cannot always make an accurate diagnosis based on the patient's complaints and the results of a physical examination (examination, palpation). It is necessary to pass tests, undergo an instrumental examination.
Gonarthrosis of the knee joint is associated with the destruction of cartilage tissue, therefore it is extremely important to start taking chondroprotectors from the moment the first symptoms appear. If the pain is relieved with pills and rubbing instead, the destruction of cartilage will progress and become irreversible.
Pathogenesis and symptoms
With gonarthrosis, the symptoms increase gradually, and often patients do not consider periodic pain in the knees and stiffness of movements a sufficient reason to see a doctor. When, finally, the patient comes to a specialist, he makes a diagnosis of arthrosis of the 2nd degree. Some people seek help only at stage 3 of the disease, when conservative treatment has practically no effect. Knowing the symptoms of gonarthrosis of the knee joint will help to avoid such a situation by raising the alarm in time.
Signs of arthrosis of the knee joint:
- pain, from moderate and episodic at an early stage to intense and persistent at a later stage. If at first the pain is localized in the knee area, then over time it covers the entire leg;
- crunch, clicks during flexion-extension of the leg at the knee;
- stiffness of movement, turning into a limitation of joint mobility;
- swelling, swelling of the knee;
- deformation of the knee joints.
Knee arthrosis can be unilateral and bilateral. In primary arthrosis associated with age-related changes, both joints are usually affected, with secondary, especially post-traumatic - one.
The causes of arthrosis are varied: trauma, systematic excessive stress on the joints, autoimmune, endocrine, metabolic disorders. But the mechanism of development of the disease in all cases is the same, as is the symptomatology. Only the development of post-traumatic arthrosis can immediately begin with acute manifestations, in other cases, the increase in symptoms stretches for a couple of years.
First, the properties of the cartilage tissue change, the cartilage becomes less elastic, dries out, becomes cloudy and begins to crack. The cushioning between the bones becomes thinner and painful when rubbing against each other. Often an inflammatory process develops in the synovial membrane - synovitis. The volume of the joint fluid increases, the knee becomes like a ball, and the temperature may rise. The destruction of cartilage leads to deformation of bones, the appearance of osteophytic growths on the periphery of the articular surfaces. Deforming osteoarthritis (DOA) is manifested by intense pain, muscles spasm, and a change in the contour of the joint is striking. Acute pain syndrome, muscle spasm and mechanical obstacles in the form of osteophytes severely restrict limb mobility.
Diseases with similar symptoms
Knee pain is typical for a number of other diseases, so you need to focus on the totality of symptoms, test results, and imaging diagnostics. In the differential diagnosis of arthrosis, the following points should be taken into account:
- if the meniscus is damaged, the pain is severe, accompanied by a crunch, appears immediately after an awkward movement, but after about a quarter of an hour it subsides, and the next day edema develops;
- inflammation of the knee tendons (tendonitis) is manifested by pain with active movements and palpation, crunching, joint stiffness, there are signs of an inflammatory process - skin redness, local fever, swelling. The diagnosis is clarified using ultrasound;
- with arthritis, a blood test reveals an inflammatory process;
- pain associated with vascular diseases, have a specific character, which is usually described by the words "twists the knees." Such pains are always symmetrical;
- to exclude tuberculosis of the knee joint, it is necessary to perform a biopsy of the synovial membrane;
- hydrarthrosis (dropsy of the joint) resembles arthrosis, complicated by synovitis, but studies do not reveal the inflammatory process, changes in the bone and cartilage tissue of the joint;
- tumors of the articulating bones are excluded by radiography.
Secondary arthrosis of the knee can develop against the background of arthritis, gout, ankylosing spondylitis, varicose veins veins. Therefore, it is important not to miss the moment when manifestations of arthrosis itself join the symptoms of the cause of the disease.
Diagnostics
Clinical signs of DOA of the knee joint are quite expressive, bone growth is visible without X-ray, the leg deviates from the normal axis. With bilateral gonarthrosis, an X-shaped (valgus) or O-shaped (varus) deformity of the extremities is formed, gait changes. At stage 2, you can already notice the coarsening of the contours of the joint. But arthrosis of the 1st degree does not have pronounced external signs, manifested by starting pains, joint stiffness in the morning, with the development of synovitis - swelling.
This set of symptoms allows experienced specialist to suspect osteoarthritis of the knee joint, but not to make a definite diagnosis with certainty. Therefore, in arthrosis of the knee joint, diagnosis should not be limited to examination and questioning of the patient.
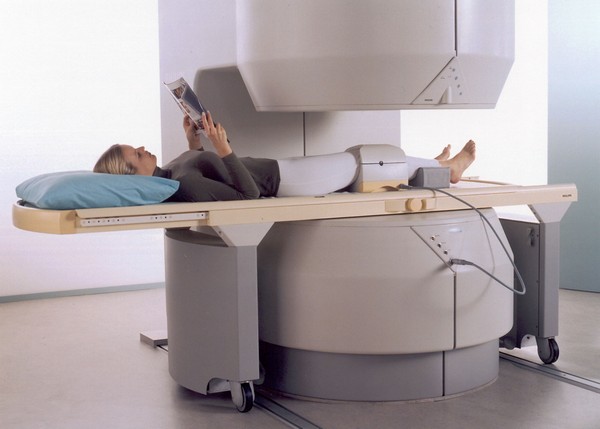
The following will help to confirm the diagnosis of gonarthrosis:
- radiography;
- cT scan (CT);
- magnetic resonance imaging (MRI).
Tests are prescribed to exclude other diseases with similar symptoms, primarily arthritis.With arthrosis, the general and biochemical blood test does not reveal abnormalities, and a slight increase in ESR indicates synovitis.
X-ray is the main method for diagnosing gonarthrosis, the medical history necessarily includes a number of images taken on different stages diseases. If the development of arthrosis has just begun, the X-ray may not show changes, and later on the picture shows:
- narrowing of the gap between the articulating bones;
- thickening of the subchondral bone (bone plate located directly under the articular cartilage);
- expansion of the articular ends of the bones;
- sharpening of the edges of the condyles;
- spine-shaped osteophytes;
- free foreign bodies (pieces of decayed cartilage) in the articular cavity.
In older people, X-rays can reveal a number of changes from this list, but symptoms characteristic of arthrosis of the knee joint are absent. Therefore, on the basis of only one X-ray examination, it is impossible to diagnose arthrosis, it is necessary to take into account the clinical signs.
With arthrosis of the knee joint, polypositional radiography is required. At a minimum, pictures are taken in frontal and lateral projections; to obtain more accurate and detailed information, they resort to oblique, axial and other projections. This requirement is due to the structural complexity of the knee joint and the possibility of localizing the degenerative-dystrophic process in a limited area, which is visible only when shooting at a certain angle.
Other methods of hardware diagnostics
Changes in bone tissue develop in a certain sequence, therefore, with the help of X-ray examination, it is possible to accurately determine the stage of arthrosis. But this method does not allow you to visualize changes in soft tissues, ligamentous-meniscus complex. Therefore, it is complemented by ultrasound diagnostics, tomography.
Ultrasound shows:
- thinning, destruction of articular cartilage;
- damage to the menisci;
- change in the volume of articular fluid (its increase is a sign of arthritis or arthrosis complicated by synovitis, but the absence of an increase in volume clearly indicates arthrosis).
Ultrasound is not enough exact method diagnostics, the reliability of the results largely depends on the qualifications of the specialist who conducts the examination. CT and MRI are more informative. Computed tomography allows you to assess the condition of bones, cartilage and menisci, ligaments and tendons, to see in detail the contents of the joint capsule. MRI is the most expensive, but the most accurate and informative diagnostic method, thanks to which specific changes can be identified at the stage of the first clinical manifestations. In especially difficult cases, arthroscopy is used - a miniature camera is inserted into the joint through a small incision.
The insidiousness of gonarthrosis lies in the mild severity of symptoms at the stage when the development of the disease can still be slowed down. If you are worried about knee pain that occurs at the beginning of the movement, but soon passes, and in the morning it takes some time to "disperse", to overcome stiffness, you should be alert and consult a doctor. Only a rheumatologist can make an accurate diagnosis and prescribe correct treatmentwhich will help on long years save physical activityavoiding disability. Early diagnosis arthrosis of the knee joint - the key to the effectiveness of treatment.
Hello dear blog guests! Irina and Igor are with you again. Everyone faced this, regardless of age and physique. Unsuccessfully got up from the sofa, unsuccessfully sat down - a crunch in the knees. We go up the stairs - an unpleasant sensation in the knees. Where does such pain come from - it's understandable, but where does constant pain in knees and joints come from?
What are the causes and what should be the treatment for knee pain? Let's figure it out.
What's special?
Due to its location, the knee is almost the main organ in pain. It just so happened that the knee, almost like the heart, is constantly involved. Over time, it wears off, gets tired and “breaks down”.
What causes the pain? There are many such factors. It all starts with fatigue and ends too active pursuits sports and diseases that affect the knee joint.
Sprain - the moment when one or more muscles are damaged. Ligaments can be stretched or broken (this is a particularly difficult case).
Damage to the meniscus - when the small pad inside the joint is damaged in some way.
For example, when squatting, lifting, etc. You can also damage the meniscus when you hit the patella, and you may not even feel the impact, but damage this small part. In older people, cartilage abrasion is more common.
Tendon rupture - this happens when there is a rupture of that part of the muscles that support the leg.
A bone fracture that forms this muscle and a dislocation of the joint itself can also occur. Many diseases carry a symptom such as knee pain.
Symptoms
Pain in the knee or under the knee itself is not a disease. This is just a symptom, a harbinger of some kind of disease.
And the symptoms can be very different and you need to understand them in order to help the doctor establish the correct picture of the disease, so we will talk about them, about the symptoms.
The most common:
- Swelling
- Bruising and redness
- Stiffness of movement
- Low amplitude of leg flexion and extension
- General weakness
- Clicks and crunches when moving
Causes of pain

Arthrosis - this is such a disease that depressingly affects all the muscles of the leg and its structure, which brings with it constrained movements, progression of pain, joint atrophy.
Arthritis – inflammatory disease, when a lot of fluid appears and the tissue grows, and this leads to the destruction of cartilage. An excellent way to get rid of this disease will be the manual "How to cure arthritis with home folk remedies" .
Osteochondrosis - a violation in the work of muscles and a strong painful phenomenon.
Gout - a consequence of the reduced work of metabolism, because it is characterized by this disease deposition of urea crystals. Under the kneecap, the muscle swells, turns red, and fatigue appears. Temperature rise is possible.
About gout, we will only remind you that you can use the manual How to Treat Gout with Natural Home Remedies , which will answer all your questions about this disease.
Inflammation bone marrow - this disease came from bacteria. Bone tissue is deformed, elevated temperature and abscesses.
Sensitivity to the cold. Muscles freeze and become fragile. It is in the cold that characteristic sensation "Break" in the knees.
Physical Education. You often spend time at work and forget about it - that's the whole reason. The muscles are weakened, and the disease develops with renewed vigor. The same can be said from the other side. You do too much, and this is no longer beneficial, but harms the whole body.
What to do?
When appearing serious symptoms consult an orthopedic surgeon, who will already determine the next steps.

Firstly, this is the identification of symptoms, that is, when the disease appeared, how much it progresses, what symptoms, what will aggravate the disease, what medications you are taking, etc.
Secondly, the analysis of the data obtained is carried out.
Then a referral for a blood test is given in order to exclude infectious diseases and viruses that caused this type of inflammation.
The fourth step is an x-ray to understand what exactly happened to the joints.
An ultrasound is done to analyze the condition of the soft tissues. Based on the procedures performed, the doctor draws a conclusion, diagnoses and selects an individual treatment.
How to eliminate the pain itself?
You can also remove pain in joints using folk methods.
Salt and snow
Take some snow and mix with a tablespoon of salt, spread right place sunflower or olive oil and attach the prepared mixture by wrapping it in a linen cloth. In the first days of treatment, it will seem to you that the pain is only getting worse, but after a few days it will disappear. It costs about 10 times to do these actions, alternating between rest and a day of treatment.
Kvass and ammonia
Soak a small linen cloth in kvass, then also in ammonia. Place the cloth on sore joints, and wrap with a warm cloth
Yellow clay
Mix clay with water so that there is a viscous sour cream consistency, and apply on the leg with a layer of 40 millimeters (the clay should be warm). Wrap woolen cloth and leave overnight. You need to do about 23 procedures
The doctor may also prescribe medication, so you need to be prepared for injections into the muscles.

It could be cortisone or hyaluronic acid... When the procedures are completed, it is worth thinking about undergoing physical therapy in order to increase muscle tone and eliminate posture problems, if any. If the injury is serious, then be prepared for intervention through surgery.
There is nothing wrong with that, because an experienced doctor will help you get back on your feet. The question may arise about replacing the joint with an artificial one, the so-called implant.
If the pain in the knee is not caused by a disease, then most likely you will be prescribed anesthetic and will be prescribed bed rest for a couple of days in order to leave the joint alone for a while.
Prevention

To once again do not load the joint, it is worth sticking to simple rules, namely: keep body weight in a healthy state, regularly provide the body with physical activity, but do not overdo it and correct posture.
Try also using the tips of the workshop "Joint gymnastics 60+" ... Do not be afraid of the figure, this gymnastics will be an excellent prevention in terms of the manifestation of any joint pain.
We hope you didn't have knee problems. But if there were any, please share with us your methods of pain relief.
Monitor your health, listen to the sensations and let the body be your ally, not an enemy. Be healthy! See you soon!
Best regards, Irina and Igor
The knee joint is considered the most vulnerable joint, primarily because of its complex structure and the loads placed on it. Orthopedists and traumatologists have to deal with a large number of patients every day who complain of pain in the knee when extending, at rest or when walking.
Causes of non-disease related knee pain
Vascular knee pain occur due to deterioration of blood circulation in the knee joints. They usually start at adolescence, during the period active growth - since the development of blood vessels in fast-growing adolescents often does not keep pace with accelerated growth bones. But their intensity after 18-20 years usually decreases (and does not increase with age, as is the case with arthrosis), are not accompanied by a decrease in the mobility of the knee joints. Pain sensations are usually symmetrical.
Diseases that accompany knee pain
Diseases in which knee pain is observed are very diverse, due to the complexity of the structure and function of the knee area. Injury to the knee can affect any of the ligaments, tendons, or fluid-filled sacs (bursitis) that surround the knee joint, as can the bones, cartilage, and ligaments that form the joint itself.
Injuryin the area of \u200b\u200bthe knee joint, it is characterized by limited bleeding into the soft tissues in the joint area, edema and local soreness that impedes movement. As a result of a bruise, microcirculation is disturbed in the tissues. Damage to blood vessels and nerve endings causes varying degrees of hemorrhage, swelling and soreness.
Traumatic hemarthrosis the knee joint, or hemorrhage into the joint cavity, develops both with bruises and with more severe damage to the joint; as a rule, it accompanies damage to the menisci, ligaments, capsules, bone tissue. With hemarthrosis, the outflowing blood affects the synovial membrane, causing it to swell and swelling of the synovial villi, which in turn begin to produce an excess amount of synovial fluid. By the nature of the remote exudate, one can judge the localization and severity of damage to the intra-articular formations. If blood predominates in punctate, it is possible to assume rupture of the synovial membrane, cruciate ligaments, damage to the internal meniscus in the subapsular zone. With damage to the articular cartilage and transchondral rupture of the menisci, there is usually no blood in the joint. Bone tissue damage is characterized by the presence of blood with fat drops in the joint. Removing blood from the joint and flushing it are recommended for the prevention of chronic serous-fibrinoid synovitis, when there is a lot of fibrin in the exudate, which has fallen out in the form of separate threads and clots, which can grow in vessels with the formation of semi-free villi.
Ligament rupture (full or partial). Damage to the external lateral ligament of the knee joint occurs less frequently than the internal one, and occurs when the lower leg is too deflected inward (for example, when the leg is twisted). The rupture is often complete, it can be combined with an avulsion fracture of a part of the head of the fibula. The patient complains of pain in the area of \u200b\u200binjury, which increases with the deviation of the lower leg inward. Movement is limited. The joint is swollen, hemarthrosis is determined. The severity of symptoms depends on the degree of damage to the ligaments of the knee joint. With a complete rupture, laxity (excessive mobility) in the joint is revealed.
Injury to the internal lateral ligament of the knee occurs more often, however, usually its damage is incomplete. Trauma occurs when the leg is too far outward. A rupture of the lateral ligaments is often combined with a rupture of the inner meniscus and damage to the joint capsule, which can be diagnosed by magnetic resonance imaging of the knee joint. The patient complains of soreness during palpation, movements, deflection of the lower leg outward, the joint is swollen. Hemarthrosis is revealed. Movement is limited. A complete rupture is accompanied by excessive joint mobility.
When cruciate ligament rupturethat are located inside the joint, hemarthrosis often occurs. Therefore, the diagnosis of rupture of these ligaments in acute period very difficult, since with hemarthrosis it is almost impossible to investigate the symptom " drawer"Characteristic for damage to the cruciate ligaments. The study of this symptom should be returned after 3-5 days or after a puncture of the joint and removal of blood. Treatment of rupture of the cruciate ligaments is surgical.
Damage to the meniscus (Meniscopathy) is the most common knee injury and is sometimes difficult to diagnose. A sharp unusual movement in the joint with a turn of the hip with a fixed foot and lower leg sometimes leads to the detachment of a part of the meniscus or to crushing it between the bones. Hemarthrosis occurs quickly; an important symptom of the blockade is determined - the patient cannot fully straighten the leg at the knee joint. This condition requires immediate referral to a traumatologist to remove the blockade. Often joint blockade resolves on its own, hemarthrosis also resolves after 5-7 days and the patient, without seeking help, continues to work. The blockade is repeated, but each time the pain after the infringement of the meniscus and hemarthrosis becomes less. However, this is a very serious situation, since repeated infringements of the meniscus over time (within 1 year) lead to the development of deforming arthrosis, and then meniscectomy (removal of the meniscus) is ineffective.
Even with the slightest suspicion of a meniscus rupture, consultation with a traumatologist and X-ray of the joint are required. The latter is due to the frequent combination of meniscus injury with intra-articular fractures.
Chronic patellar dislocation (displacement of the patella) is relatively rare (0.4 - 0.7% of all dislocations), but often recurs later. In the case of the development of the habitual dislocation in children, as a rule, with age, deformity of the knee joint is formed in the form of a valgus (X-shaped) deviation of the lower leg and a progressive dysfunction of the limb. In most cases, there is an external dislocation of the patella, less often - an internal one. Patellar dislocation, called torsional dislocation, in which the patella rotates around its axis is very rare. Patients with chronic instability of the patella are concerned about pain in the anterior and inner surface knee joint. They may complain of a feeling of unsteadiness, looseness in the knee. When examining patients special methods determine the degree of displacement of the patella. Clarify the diagnosis by X-ray examination.
Inflammation of the tendon (tendonitis). The reasons for the development of tendonitis are:
- significant physical stress on the joint for a long period of time.
- injuries;
- infections caused by bacteria, such as gonorrhea;
- the presence of diseases of a rheumatic nature (gout or arthritis);
- allergic reaction the body for medications;
- anatomical features body structure: different length extremities contributes to the development of knee tendinitis;
- Weakened tendons or their improper development;
- non-observance of correct posture.
The most prominent symptoms of tendonitis are pain and limitation of movement. Painful sensations at the site of inflammation and nearby areas are persistent, do not pass for a long time. The pain may come on suddenly, but sometimes the soreness increases as the inflammation intensifies. It is noted hypersensitivity when probing the affected tendon.
Bursitis - inflammation of the periarticular bursa (bursa), which contains fluid that washes the joint. Common symptoms of bursitis are redness, swelling, pain and tenderness over the kneecap, and limited mobility in the joint. If bursitis is allowed to develop into a state of chronic inflammation, there is the possibility of adhesions that can only be removed by surgery.
Synovitis Is an inflammation of the synovial membrane, which covers the articular cavity from the inside. In this case, an effusion is formed, which accumulates in the joint capsule. In addition to injury, synovitis can develop with various autoimmune processes, with metabolic disorders, against the background of existing diseases (gonarthrosis) of the knee joint, inflammation can be secondary (reactive synovitis of the knee joint). As a rule, the inflammation is aseptic in nature (that is, there is no infection) and is manifested by the formation of serous effusion. If an infection joins, the nature of the synovial fluid changes, pus appears in it and purulent synovitis develops. Symptoms appear gradually, over several hours or even days after the injury. The joint increases in volume. The fluid, as it were, expands the intra-articular structures, deforms the contours of the knee. Joint function is limited, but movement disorder is not always accompanied pain syndrome... Nevertheless, the pain is still characteristic of this pathology, but it is not sharp, but dull, of medium intensity. The skin over the joint is not hyperemic, the temperature is not elevated.
Baker's cyst - a soft, dense, elastic tumor-like formation that develops on the back of the knee joint (in the popliteal fossa). The skin above the swelling is of normal color, not adhered to the underlying tissues. Baker's cyst protrudes more with an extended knee. When bent, it decreases in size or disappears completely. The appearance of a Baker cyst is a consequence of any diseases of the knee joint, among which the most common are: joint injury, damage and degenerative changes menisci, damage to the cartilage of the joint, chronic synovitis (inflammation of the synovial membrane of the joints), osteoarthritis, patellofemoral arthrosis, osteoarthritis, rheumatoid arthritis. Visually, Baker's cyst is a dense, elastic, rounded formation in the popliteal fossa, which can be imperceptible when the knee is bent and protrudes quite clearly when the joint is extended. In this case, in the popliteal region there may be a feeling of discomfort or pressure (and sometimes pain), difficulty or soreness when moving the knee. With a significant size of Baker's cyst, due to compression of adjacent vessels and / or nerve trunks, there may be a coldness of the skin of the leg below the knee, a feeling of numbness, tingling, "creeping", edema and other signs of impaired blood circulation and innervation. TO possible complications Baker's cysts include the development of thrombophlebitis and deep vein thrombosis of the lower leg, the development or aggravation of pre-existing varicose veins of the saphenous veins, as well as rupture of the cyst wall, manifested by a sharp severe pain, reddening of the skin of the back of the leg, increased local temperature, swelling.
Goff's disease is damage and degeneration of the adipose tissue surrounding the knee joint. This is a rather difficult to diagnose condition, which is often confused with damage to the meniscus, the so-called "articular mouse" - a fragment of cartilage or bone in the body of the joint. Without proper treatment of the knee in Hoffa's disease, the "fat pad" ceases to perform its buffer function - the disease becomes chronic, which increases the risk of knee arthrosis, can provoke constant pain in the knee joint for many years. Most often, with a knee injury, fatty lobules are damaged, pinched, hemorrhage and tissue edema. In place of damaged cells, fibrous tissue grows, which cannot perform the functions of adipose tissue. In a number of situations, Hoffa's disease can develop against the background of arthrosis of the knee or under the influence hormonal changes, for example, in women in menopause. In the acute stage of the disease, damage to the fatty body can be diagnosed already upon examination. Besides knee pain, quadriceps weakness, characteristic feature on palpation is localized swelling. But the chronic stage is not always easy to determine - MRI, CT or arthroscopy may be required if there is no response to conservative treatment.
Osgood-Schlatter disease (osteochondropathy of the tibial tuberosity). Often occurs after increased physical activity or injury caused by tension on the patellar tendon. Affects mainly adolescent boys aged 13-15 years involved in sports. The symptoms are pain, swelling in the area of \u200b\u200bthe tibial tuberosity.
Arthritis - joint inflammation, which most often occurs in diseases such as rheumatoid, reactive, psoriatic arthritis, as well as ankylosing spondylitis, rheumatism, gout. Characteristics - joint pain, stiffness, limitation of joint mobility, swelling, fever in the affected area, joint deformity.
Deforming osteoarthritis Is a joint disease characterized by damage (thinning and destruction) of the cartilaginous tissue of the joints with simultaneous deformation and changes in the structure of the bone heads. On the early stages the development of arthrosis manifests itself with such symptoms as pain, usually arising at the beginning of movement after a state of rest, and these pains disappear rather quickly. As the disease progresses further, pain during movement increases, appears not only during movement, but also at rest, there is a feeling of stiffness of the joints, limitation of their mobility. With deforming arthrosis of the knee joint, a significant curvature of the leg occurs, its axis deviates from a straight line, which leads to difficulty and complete impossibility of the joint. Finally, in the last stages of development, deforming arthrosis leads to its complete destruction. To restore joint function, relieve pain, restore limb length, knee arthroplasty is performed.

Patellar chondropathy – pathological conditioncharacterized by degenerative-necrotic changes in the articular cartilage of the patella. It occurs both immediately after trauma of varying intensity, and against the background of chronic trauma and, especially, with lateral displacements of the patella. Patients complain of pain in the patella, which increases with physical activity... Kneeling is very painful even for a short time. Finding lower limbs in a bent position, such as when driving for a long time in a car, can also lead to pain in the patella. When moving the knee joint, you may hear a crackling sound or clicking sounds.
Knee Chondromatosis - a long-term progressive disease of unknown etiology, consisting in the formation of multiple cartilaginous nodes inside the synovial membrane of the articular bag. Cartilaginous nodes can range in size from a few millimeters to several centimeters, and their number ranges from a few separate formations to several dozen. With a significant number of cartilaginous nodes or with the formation of large nodes, moderate painful sensations, there is a crunch and limitation of limb mobility in the affected joint, swelling, and with the formation of a "joint mouse" - infringement. Severe disfigurement and significant limitation of joint function may occur.
Koenig's disease or dissecting (cutting off) osteochondrosis (ostechondritis) - a disease in which the area of \u200b\u200bcartilage covering the bones gradually exfoliates and may even completely separate from the bone. In the knee joint, it affects only the condyles. femur or the patella (patella). Symptoms depend on the stage of the disease. At the onset of the disease, the patient complains of discomfort in the joint, minor pain. With the progression of the process, there is an increase in pain in the joint, synovitis appears. There may be an incomplete separation of the dead cartilage, a blockade of the joint is possible (occurs due to the detachment of a piece of cartilage, leading to disruption of the joint). Further, the dead cartilage is completely separated from the bone, blockade of the joint, the progression of pain and synovitis is possible. If the disease lasts for a long time, then lameness leads to a decrease in the range of motion in the knee joint and atrophy of the quadriceps muscle of the thigh.
When osteoporosis there is a change in the structure of bone tissue, which leads to an increase in their fragility and tendency to fracture. Osteoporosis is characterized by pain in the joints and bones, leg cramps, more often at night, aching pain in the back (spine), the presence of fractures.
Knee osteophytes - bone formations that arise in the knee joint in the case of the development of degenerative-dystrophic processes or gonarthrosis in it. The people believe that osteophytes are the deposition of salts in the joints, this is not true. In fact, the formation of such "growths" occurs due to malnutrition of the articular cartilage. The osteophyte can break off, and then the pain in the joint will be acute, often this process is accompanied by inflammation.
Infectious diseases, including urogenital (such as chlamydia, gonorrhea, ureaplasmosis, etc.) and intestinal (dysentery, yersineosis, salmonellosis), occurring latently, can lead to reactive arthritis of the knee joints. In this case, pain in the knee joints often occurs not only when walking. Reactive arthritis of the knee joint is bad in that it usually affects the tendons around it in addition to the joint. In addition, inflammation of a number of other joints and eyes, as well as discomfort in the genital area, often join the inflammation of the knee joints. Patients may note the connection of arthritis with a previous genitourinary or intestinal infection.
Bone tuberculosis... The disease begins either with the melting of the bone substance of the bone, or with the necrosis of significant areas of the skin, and this process begins to spread over time to an ever larger area. Regardless of the initial manifestations, tuberculosis of bones and joints causes the formation of a purulent fistula or a cavity that opens outward. It should be noted that after a few weeks, the inflammatory process can stabilize, and the patient has a stable remission.
Osteomyelitis of the bone - a purulent-necrotic process that develops in the bone and bone marrow, as well as in the surrounding soft tissues, caused by bacteria. At the beginning of the disease, a person may complain of weakness, muscle pain. Then the temperature rises sharply to 39-40 degrees. Pain, clearly localized in the affected area of \u200b\u200bthe bone, occurs almost immediately. Sharp, boring or bursting from the inside, aggravated by the slightest movement - such pain is difficult to confuse with anything. The affected knee is edematous, the skin becomes stagnant red, the veins are dilated.
Sciatic nerve neuropathy - manifestations depend on the level and extent of nerve damage. For example, with damage to L4 (lumbar vertebra 4), patients complain of pain in the anterior thigh, along the inner surface of the knee joint and lower leg, impaired skin sensitivity on the anterior surface of the thigh and lower leg, weakness of the flexors of the lower leg and adduction of the thigh, knee reflex decreases.
Other causes of knee pain, such as bone and soft tissue tumors, are much less common.
Examination for knee pain
There are a great many diseases of the knee joint: some are associated with damage to the ligaments, the second - with deformation of cartilaginous tissues, and others - with dystrophic changes in the bone itself or inflammatory processes... Correct diagnosis always begins with patient interview and manual palpation. Depending on certain signs of the disease, the doctor may prescribe additional methods survey.
1. General analysis blood (possible anemia, leukocytosis, increased ESR in rheumatoid arthritis, ankylosing spondylitis);
2. Biochemical analysis blood: an increase in uric acid with gout;
3. Microbiological examination (for example, scraping from the urethra for chlamydia with suspected reactive arthritis);
4. X-ray examination is one of the main methods of examination for pain in the knee joint. Specific changes characteristic of a specific pathology will be visible;
5. Serological analysis: rheumatoid factor in rheumatoid arthritis;
6. Puncture biopsy of bone in case of suspected bone tuberculosis and osteomyelitis: material for inoculation is obtained by aspiration of pus from bone or soft tissues, or a bone biopsy is performed;
7. Puncture of the joint: the needle is inserted into the articular cavity and a part of the exudate is taken for examination for transparency, protein and blood cell content, and microorganisms are cultured.
8. Arthroscopy - carried out with both diagnostic and therapeutic purpose, for example, with trauma to the meniscus, cruciate ligaments, etc.
9. Densitometry - measurement of bone density in osteoporosis.
10. Ultrasound procedure knee joint for suspected osteoarthritis, traumatic injuries and diseases of the menisci, etc.
11. Magnetic resonance imaging and computed tomography (for example, if chondromatosis is suspected).
Knee pain treatment
There is no single universal way treatment of all knee diseases. What treatment is needed in each specific case depends on precise definition causes of pain, because all of the above diseases require different approach to your treatment. However, some rules must be followed when knee pain occurs.
1. Reduce the load to such an extent that unpleasant sensations... In case of acute pain, completely eliminate the load and apply a fixation bandage in order to provide the knee with immobility.
2. Wearing an elastic bandage or bandage to stabilize the joint.
3. On the recommendation of a doctor, the use of hot compresses to warm the knee. This is done to improve tissue microcirculation. Warming ointments (such as finalgon) can be used.
In case of acute pain in the first two days, a cold compress (a plastic bag with ice or bottles with ice water). Cold compresses should be applied for 15 minutes, and then take a break for an hour so that normal blood circulation in the leg is restored.
4. The use of anti-inflammatory drugs (paracetamol, ibuprofen).
5. Thorough warm-up of the joint before running and other workouts with a gradual increase in load, starting with minimal.
6. The use of drugs chondroprotectors.
If your knee pain persists despite all these measures, it is possible that your knee injury is more complex than you initially thought. In this case, you should definitely contact a trauma specialist. A doctor should also be consulted if the pain has arisen spontaneously, for no apparent reason, with severe, constant and long-lasting pain, visible joint deformation, redness of the knee, discoloration of the leg below the knee and impaired sensitivity. Remember that often the health and mobility of your knee depends on the timeliness of the treatment started.
Which doctor to see for knee pain
Depending on whether the injury occurred, it is a therapist or traumatologist. You may need to consult doctors of the following specialties: orthopedist, osteopath, rheumatologist, neurologist.
Physician therapist Yu.V. Kletkina
Knee pain can also be due to a form of arthritis
The first step to treating knee pain is to get the correct diagnosis. Your knee can become painful due to ligaments, tendons, muscle problems, or changes in bone. Knee pain can also be due to one of 100 forms of arthritis.
Knee arthritis symptoms
To help a doctor diagnose the cause of knee pain, it's important to pay attention to the symptoms. What are the symptoms of knee arthritis?
When is knee pain a symptom of arthritis?
The American Academy of Orthopedic Surgeons states that if knee pain is a consequence of arthritis, it is likely to develop gradually and then gradually get worse. This is different from an injury in which sharp pain the knee gets better over time. With arthrosis, knee pain may worsen due to activities such as climbing stairs, standing up from a chair, or other movements that require you to bend your leg and move your entire body weight onto the knee. In the case of rheumatoid arthritis, knee pain may be worse in the morning or worse after periods of inactivity. Rheumatoid arthritis is also characterized by periods of outbreaks and remissions. With osteoarthritis, pain can occur on only one side of the body, and with rheumatoid arthritis, both knees are usually affected equally.
Stiffness and swelling in the knee joint
In the case of osteoarthritis, you may find that your knee becomes stiff and difficult to move. Loss of flexibility in the knee joint can be the result of a sedentary lifestyle, lack of exercise. Rheumatoid arthritis can cause swelling and inflammation in the joints. Your knee may become red and warm to the touch, may develop subfebrile temperature body. In rheumatoid arthritis, the joint can become deformed as the disease progresses. With both forms of arthritis, you may find that your knees are affected by the weather.
Weakness in the knee joint
According to the Arthritis Foundation, both rheumatoid arthritis and arthrosis can cause sensations such as stiffness or crunching in the knee. Your knee may become unstable, and there may be limitedness and pain in the knee joint. Arthritis can even make you limp if you try to relieve pressure on your knee.
How do you know if knee pain is caused by arthritis?
Knee pain can be caused by many things. The tendons, ligaments, and muscles surrounding the knee joint may be damaged. Knee pain can also be associated with a form of arthritis. The only way to know the cause of knee pain is to see your doctor for a correct diagnosis. Tests can help determine the cause of your knee pain.
First of all, the doctor will pay attention to your symptoms: What kind of pain are you experiencing? What leads to better pain, and what makes it worse? The doctor may look for signs of stiffness, swelling, and redness that may indicate arthritis. If you have pain in one knee, osteoarthritis may be suspected; pain in two knees most likely indicates rheumatoid arthritis. Arthritis pain in the knee usually gets worse after periods of inactivity and improves with movement. This may differ from ligament or tendon injuries that worsen with movement. In addition, arthritis can cause general pain, while damage to a tendon or ligament can lead to very localized pain.
X-rays will need to be taken to look for changes in the bone that indicate arthritis. Osteoarthritis, one of the most common forms, results from wear and tear on the cartilage in the knee. When this happens, the bones rub against each other, which can lead to the development of bone spurs. X-rays are the most informative test, allowing you to confirm the diagnosis of osteoarthritis. It may show a narrowing of the space between the bones (indicating that the cartilage is thinning), as well as changes in the bone (like a spur). If your doctor does not see any changes on the x-ray, they may order an MRI test that shows injuries to the surrounding soft tissue and can help rule out arthritis as a cause of knee pain.
We need blood tests. When diagnosed with rheumatoid arthritis, additional blood tests will be needed to determine if knee pain is associated with arthritis. Rheumatoid arthritis is autoimmune diseasewhich causes inflammation of the joint capsule. A blood test can show active inflammation and other factors that are present in this condition (See article:). For rheumatoid arthritis, a blood test is likely to show low level erythrocytes, high level leukocytes and elevated level platelets. In addition, your doctor may take a fluid sample from your knee, which may help confirm the diagnosis of rheumatoid arthritis.
How to relieve arthritis knee pain?
If you suffer from pain in one or two knees due to arthritis, you should be aware that there are ways to relieve the pain. There are many forms of arthritis that affect each person differently. Therefore, you may even need to try a combination of methods and approaches to help relieve knee pain and stay active.
- You need to lose weight! The lower your body weight, the less stress on the knee joint. The American Academy of Orthopedic Surgeons states that weight loss can reduce stress on weight-bearing joints (like the knee joint). Losing weight can help reduce pain and improve joint function, especially when walking. A weight loss of just 7.5 kg can reduce knee pain by 50% (according to a recent study presented at the American College of Rheumatology; 10th Annual Scientific Meeting). Aerobics or cardiovascular exercise is the best way for weight loss. So walk, bike, swim and do and dance. To successfully lose weight, a person needs to do 30 to 45 minutes of aerobic exercise at least three to five days a week. These 30-45 minutes can even be broken down into shorter segments throughout the day if needed.
- Perform regularly physical exercises... Exercise is an important part of knee arthritis treatment. Stretching and flexibility exercises can help reduce stiffness in the knee joint. Strengthening the muscles in your thighs and legs will help relieve pressure from the knee joint. Squats, lunges, etc. are helpful. The National Institute of Aging believes that exercise strengthens muscles and strong muscles support and protect joints. If the exercises on the ground are too difficult for you, do the exercises in the water. Do exercises that do not put pressure on your knees. It is important to remember that for rheumatoid arthritis, you should not exercise on the days when the outbreak occurs.
- Use assistive devices and supports. Using a cane, crutch, or brace can also help with knee arthritis. If you have arthritis in only one knee, use a cane or crutch in your opposite hand. Using a cane in the same hand as the affected knee will cause you to lean too hard on the affected side. Also, talk to your doctor about which type of brace is best for your case. A brace can help maintain proper knee alignment, which can help reduce your symptoms.
- Let your doctor prescribe treatment for your arthritis. There are medications that are effective for treating knee arthritis. However, the lifestyle changes listed above are still needed. According to the data National Institute Health, lifestyle changes without medication are preferable for osteoarthritis and other forms of joint inflammation. If necessary, drugs should be used in addition to lifestyle changes. Usually doctors prescribe pain medications, anti-inflammatories, steroids, and muscle relaxants. In addition to medication, hot and cold therapy is helpful for knee arthritis.
- Consider having surgery. Where arthritis of the knee causes severe symptoms or significantly affects your daily life, you may need surgery to relieve symptoms. There are many types of knee surgery, including knee replacement options. Consult with your doctor if you need surgery.
Never ignore knee pain! Without adequate treatment injury, inflammation, and pain in the joint may develop into a more severe condition. The sooner you start treatment, the better your chances of recovering quickly. See your doctor for a correct diagnosis. Only ascertaining the exact cause of your knee pain will help you find the right approach to manage symptoms. Remember knee arthritis is not a death sentence! There are methods that can help relieve knee pain and medications that a doctor prescribes to treat knee arthritis.
