What to do if joints hurt during menopause. Why does knee pain occur - causes and treatment
The climacteric period that begins after 45 years in women, implies extinction reproductive function when the hormones of the reproductive system are produced in smaller quantities. Along with an imbalance of some hormones, the production of others may decrease, which ultimately provokes various negative processes in organism. These include rapid weight gain, excessive irritability, excessive sweating and joint pain.
The latter appear especially often when a woman has chronic inflammatory processes in her body.
Why joints hurt during menopause and how to cope with such a manifestation without harm to health, we will analyze further.
Features of the course of menopause
 Climax is a special period in the life of every woman, which signals the end of her ability to procreate. Menopause lasts about 3-4 years, and during this time the body undergoes restructuring, the need for which is dictated by a decrease in the production of sex hormones.
Climax is a special period in the life of every woman, which signals the end of her ability to procreate. Menopause lasts about 3-4 years, and during this time the body undergoes restructuring, the need for which is dictated by a decrease in the production of sex hormones.
Since it is hormones that control the work of the entire body, even a slight imbalance can provoke serious problems. The eggs no longer mature, and the genitals of women after 45 years of age lose their main function. Menstruation stops, along with which symptoms such as:
- fast fatiguability;
- increased irritability;
- sudden change of mood;
- increased sweating;
- deterioration of the bone tissue, which is expressed by a decrease in its strength and elasticity (change in posture, risk of fractures);
- uncontrolled weight gain that is not related to the food consumed;
- appearance unwanted vegetation on the skin.
Also quite often the joints hurt with menopause.
There are many reasons and explanations for this. scientific point vision. Therefore, it is worth considering this issue in more detail.
Decreased function of estrogen synthesis
Functioning of the ovaries after 45 years markedly reduced, which indicates the irreversibility of the upcoming processes. In the body, all functions and systems are interconnected, therefore, when attenuating hormonal system the whole body suffers. Estrogen is produced in a smaller amount, which provokes deterioration general condition woman's health. Along with irritability and hot flashes, bone tissue suffers. Calcium is no longer absorbed in the right amount, which makes the bone tissue looser. This factor increases the risk of fractures, and also affects the state of posture.
Immunity is also reduced, so women Balzac age may be more likely to develop respiratory problems. Menopause is a kind of stress for the body. Most difficult time fall on 45-50 years, when there is a complete extinction of the reproductive system. The condition of the skin worsens, wrinkles become more noticeable.
In the case when the level of estrogen decreases quickly, the stress for the body increases. Most often it causes hormonal disbalance, in which the level of all hormones is unstable.
This affects the performance of the whole organism, especially the musculoskeletal system.
kind of pain
Aching pain in the joints that appears suddenly and is not associated with influence external factors. Most often, the peak of pain occurs in evening hours when the body is most tired.
Additional symptoms
Joint pain may present on its own or may be associated with additional symptoms climax like:
- drowsiness;
- irritability;
- hot flashes and increased sweating;
- loss of self-control;
- increased appetite and desire to eat more unhealthy foods;
- fatigue and inability to walk for long distances.
Pain localization
Unpleasant sensations that distract from daily work can be associated with changes in the weather, especially with high humidity.
All joints can hurt, but the peak of pain is in the knees and lower back.
Which doctor will help?
When pain occurs frequently and interfere with life you need to seek help from professionals such as:
- Gynecologist - will help evaluate the process of menopause, as well as identify possible pathologies reproductive system caused by menopause.
- Endocrinologist - will reveal the level of hormones in the blood, and also help to correct them.
- A rheumatologist or surgeon will advise on the treatment of joint pain directly.
Diagnostics
Many women let the menopause process take its course without giving own health due attention. However, it should not be forgotten that diagnostics helps to avoid serious problems with health. A blood test for hormones will help to identify the presence of deviations in the level of estrogen from the norm. The direction for the analysis is given by the endocrinologist on the basis of the patient's stated complaints.
With severe pain in the joints, x-rays will be required, since there is a high probability of progression of destructive processes.
Treatment
Synthetic substitutes will make up for the deficiency of hormones or equalize their levels relative to the recommended norms. hormonal nature. Women are assigned hormonal preparations, but there is a need for constant monitoring. Once a week, the patient should donate blood to find out if the medicines are suitable and how the body reacts to them.
Pain can be relieved by drugs of the NSAID group: Diclofenac, Naklofen, Nurofen. They are used both orally and topically, in the form of ointments and creams with analgesic effect.
As prophylactic many doctors recommend the use herbal preparations in the form of teas that contain natural substances able to control the climacteric process.
Osteochondrosis
 This disease is a consequence of a decrease in the synthesis of hormones and the leaching of calcium compounds from the body. The spine is affected, and the posture is bent. Appear constant pain in the back, which are especially pronounced during physical exertion. Distance between vertebrae spinal column is constantly reduced, as cartilaginous tissues are prone to dystrophy. There is a high probability of the appearance of a hump on the back, which is caused by the displacement of the vertebrae relative to the skeleton, as well as the infringement of the nerve endings.
This disease is a consequence of a decrease in the synthesis of hormones and the leaching of calcium compounds from the body. The spine is affected, and the posture is bent. Appear constant pain in the back, which are especially pronounced during physical exertion. Distance between vertebrae spinal column is constantly reduced, as cartilaginous tissues are prone to dystrophy. There is a high probability of the appearance of a hump on the back, which is caused by the displacement of the vertebrae relative to the skeleton, as well as the infringement of the nerve endings.
As a result of violation of the natural position of the vertebrae, soft tissues and nerve endings located around suffer. They can be pinched between the vertebrae, causing pain, numbness, and shooting.
Osteochondrosis most often develops in those women who:
- lead a sedentary lifestyle;
- do not play sports;
- are overweight;
- wear uncomfortable shoes on the high heels, which contributes to uneven distribution of the load on the spine;
- malnourished, and their diet is devoid of enough protein and calcium with magnesium.
kind of pain
The pain is aching, shooting, aggravated by turning and bending the back.
Also development pain syndrome promotes prolonged sitting at the computer and a sedentary lifestyle.
Additional symptoms
Back pain can be accompanied by: unpleasant phenomena, how:
- fast fatiguability;
- increased appetite;
- apathy;
- depressive state;
- hot flashes and excessive sweating.
Pain localization
Most often, osteochondrosis affects the thoracic spine, so the pain is more pronounced in the chest, shoulder blades and neck.
Sometimes osteochondrosis is manifested by pain in the lower back, giving to the sacral region.
Which doctor will help?
Since the disease is directly related to endocrine system consultation of the following specialists is required:
- Surgeon - assesses the degree of damage to the joints of the spine, informing about the need for treatment.
- Endocrinologist - establishes the relationship of the disease with deviations in the level of hormones produced in the body.
- Gynecologist - examines for the presence of diseases of the genital organs, since problems with hormones provoke their rapid development.
Diagnostics
The plan of diagnostic measures includes such procedures as:
- Radiography - helps to identify the degree of damage to the spine, the focus of the lesion and further prognosis.
- A blood test for hormone levels - shows a real picture of the functioning of the endocrine system.
- Ultrasound of the genital organs.
Diagnostic measures are carried out in a complex, since one problem is closely interconnected with another.
Treatment
Severe back pain that cannot be relieved with complex pain medications, reduced by intra-articular injections by injecting an anesthetic directly into the pain site. Such intra-articular blockades are used only in the acute course of the disease. In other cases, conservative methods of treatment are used:
- Taking NSAIDs - reduce inflammation, swelling and pain in soft tissues damaged vertebrae.
- Drugs that improve neural conduction - help restore the sensitivity of the back, which has disappeared due to compression of the nerve roots.
- Drugs that accelerate metabolic processes - help reduce the level of toxic substances in cells and tissues.
- Local anesthetics - help reduce back pain.
- Vitamin complexes with chondroitin and calcium help to fill the deficiency useful substances in the body, as well as accelerate the processes of regeneration of damaged cells and slow down their degeneration.
To maintain posture, special corsets and bandages are used to help relieve the tone of the muscles of the spine.
Arthritis
 This disease develops against the background of a weakened general immunity, as well as in the presence of chronic foci of inflammation in the body. In the joint bag, the inflammatory process progresses, affecting nearby tissues. Cartilage is the most vulnerable tissue, which further thins out and causes the bones articulated into the joint to rub against each other during movement, causing severe pain.
This disease develops against the background of a weakened general immunity, as well as in the presence of chronic foci of inflammation in the body. In the joint bag, the inflammatory process progresses, affecting nearby tissues. Cartilage is the most vulnerable tissue, which further thins out and causes the bones articulated into the joint to rub against each other during movement, causing severe pain.
Arthritis is chronic disease, it is impossible to cure it completely (and even more so with menopause). The joints are gradually affected, the articular bag is deformed, which ultimately leads to complete immobilization.
During menopause, this process develops extremely rapidly, so it is important to control it and not delay treatment.
kind of pain
The pain is aching, bursting. There may be a burning sensation in the joint itself. Unpleasant sensations are manifested mainly in the morning hours, which is explained by the increased likelihood of the development of stagnant processes in the joint. Also, the joints react to changes in the weather, starting to hurt long before it changes.
Additional symptoms
In addition to pain manifestations that increase with movement, arthritis symptoms such as:
- feeling of heat and swelling of the joint;
- hyperemia skin;
- discoloration of the skin around the joint;
- puffiness;
- decrease in performance.
Localization
The knee joints are most commonly affected, but pain can also occur in the elbows, hands, toes, and hands.
Which doctor will help?
V this case you will need to consult a rheumatologist, as well as a surgeon, therapist and endocrinologist, since arthritis is a systemic disease.
Diagnostics
To identify arthritis, a comprehensive diagnosis is used, which includes:
- Ultrasound of the joint - shows the presence inflammatory process.
- Radiography - helps to determine the localization of the inflammatory process and its prevalence.
- A blood test for rheumatic factor - reveals the presence of a tendency to rheumatoid arthritis.
- Examination of the joint fluid for the presence of pathogenic microflora - a puncture is performed, in which a syringe needle is inserted into the intra-articular gap.
- Visual examination - the doctor examines the affected joint, visualizing clear signs deformities, hyperemia of the skin and swelling of soft tissues.
Treatment
Based on the results of the analyzes and identification of the type of causative agent of the inflammatory process, a decision is made on the need for one or another type of antibiotic therapy. For cupping acute pain use novocaine blockade, which is injected directly into the joint space. Drugs of the NSAID group are widely used, helping to eliminate swelling and inflammation, but key role given antibiotics.
Auxiliary components are vitamin complexes and bio-additives, whose action is aimed at strengthening the immune system. If the joint is worn out, it may need to be replaced with an artificial implant.
Physiotherapy procedures help accelerate the regeneration of damaged cells of cartilage and bone tissue.
These include:
- shock wave therapy;
- magnetotherapy;
- balneotherapy.
Hernias
 In the presence of osteochondrosis, a fairly common phenomenon is intervertebral hernia. They formed as a result of increased compression of the vertebrae when the latter compress the intervertebral discs, forcing them to change their usual anatomical position.
In the presence of osteochondrosis, a fairly common phenomenon is intervertebral hernia. They formed as a result of increased compression of the vertebrae when the latter compress the intervertebral discs, forcing them to change their usual anatomical position.
The intervertebral discs protrude outward, forming a hernia. This neoplasm causes severe pain, since at the slightest movement the hernia can rupture, and the contents of its capsule will pour into the region of the vertebrae, provoking a large-scale inflammatory process.
The risk group includes those women whose work is directly related to weight lifting.
Excessive stress on the spine, as well as wrong shoes and lack good sleep provoke a deterioration in the condition of the intervertebral discs, and with menopause, the likelihood of their occurrence is maximum.
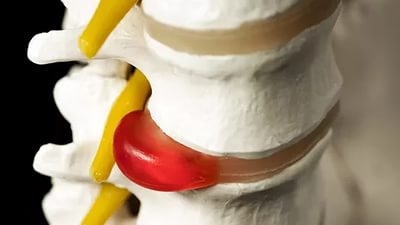 kind of pain
kind of painThe pain is sharp, shooting, squeezing. A person cannot move, and any movement causes severe pain.
Additional symptoms
In addition to back pain, symptoms such as:
- increase in body temperature;
- general weakness
- cold sweat;
- painful shock.
Localization
The peak of pain falls precisely on that part of the spine where there is a hernia.
Which doctor will help?
In this case, you will need the help of a surgeon and an orthopedist.
Diagnostics
The protrusion of the disc is visualized on the radiograph, which is a key method for diagnosing pathology. As auxiliary components can be used:
Treatment
The main task facing surgeons is to reduce compression, as well as return the disc to its usual place, which is achieved through surgery. Intra-articular injections help to stop pain shock, but they should not be abused.
In the postoperative period, it is necessary to wear a bandage, as well as compliance with all precautions.
Other reasons
Indirect causes, which are also capable of provoking joint pain during menopause, are:
- gout;
- the presence of an infection in the body;
- problems with immunity;
- violation of sleep and rest;
- poor nutrition, devoid of nutrients.
In which case immediately see a doctor?
- there is a hormonal imbalance;
- the condition worsens sharply;
- new symptoms are added every day.
Many women do not know what to do with menopause, when the joints hurt.
Don't panic. Early diagnosis will avoid serious health problems, and also prolong the youth of a woman.
Therapy to improve the condition
Treatment of pain in the joints with menopause should be carried out in a timely manner. It is impossible to stop the aging process, but there are a number of ways to make it less painful for the body:
- Exercise daily with simple exercises.
- Eat right, avoid harmful products and alcoholic drinks.
- Take vitamin complexes that will help fill the deficiency of nutrients in the body.
- Watch out for the strong physical activity.
Thus, menopause is inevitable, but its course can be alleviated.
Watch a video on this topic
Diseases in the joints, which are a consequence, cannot be ignored, since after 45 years the regenerative processes are slowed down by 5-10 times. If persistent aching pains appear, you should consult a specialist, and if there are any acute pains, you should not postpone a visit to the doctor.
In contact with
Hormones play important role in a woman's life. And this is not only maintaining the reproductive function, but also ensuring the smoothness of the skin, Have a good mood, protection against infections, cardiovascular disease. The onset of menopause in a woman leads to a change in the functioning of all body systems. From the age of 40-45, there is a gradual decrease in the level of sex hormones, menstruation loses its cycle, symptoms of menopausal syndrome appear, and menopause occurs at 45-50 years.
After the onset of menopause, only one inactive hormone remains in the hormonal arsenal of a woman - estrone, which is produced by subcutaneous fat cells and cannot provide the usual estrogen functions.
connective tissue aging
The absence of female sex hormones triggers the aging process, primarily the aging of the connective tissue. Where is most of the connective tissue found? These are skin, joints and ligaments. We can observe changes on the skin with our own eyes - these are wrinkles. The cartilaginous structures of the joints also age in the same way. There are pains in the knee joints when going down the stairs, in the evening, and in the morning there is starting stiffness, which takes 5-10 minutes to disperse. All of these symptoms fit into the diagnosis of osteoarthritis. Chondroprotectors help prevent the rapid progression of osteoarthritis.
Osteoporosis: Bone loss in the first 2 years of menopause is comparable to that of astronauts in orbit.
Estrogen deficiency triggers the processes of resorption (destruction) of bone tissue. Within 2-3 years after the cessation of menstruation, a woman loses 4% of bone tissue per year. In the future, the processes of destruction of bone tissue slow down somewhat, but many women, especially those with a slender physique, develop osteoporosis. In menopause, all these processes are manifested by pain in the bones, cramps in the calf muscles, and back pain. Bone mineral density can be determined using x-ray densitometry. This study available almost everywhere. It allows you to assess the initial state, as well as the dynamics of the process during treatment. For the prevention of osteoporosis in menopausal women, it is advisable to increase the amount of dairy products in the diet, active image life and take calcium supplements.
immune restructuring
Another disease that manifests itself in women 40-50 years old is rheumatoid arthritis. The reasons for its occurrence at this age are unclear, a certain role is assigned to the immune restructuring of the body, infection against the background of a genetic predisposition. With rheumatoid arthritis, the small joints of the hands are affected, severe stiffness appears. All groups of joints are connected to the process like an avalanche, up to the jaw. In severe cases, patients with difficulty move and need outside help.
Immune restructuring leads to increased sensitivity to infections. In this regard, women often develop reactive arthritis (more often against the background of infections of the urogenital tract). The disease is acute, with the development of intense pain in one or more joints, the process is eliminated by the appointment of antibiotics.
The thyroid gland is weakening
Women in their 40s and 50s often show changes in thyroid gland. Its restructuring is not directly related to estrogen deficiency. But we all live in an iodine-deficient region, so it is by this age that nodes often begin to form in the thyroid gland (multinodular goiter), and autoimmune thyroiditis often begins. Diseases thyroid gland often provoke pain in the wrist joint. It is this pain that brings a woman to the doctor. And further examination reveals the pathology of the thyroid gland.
Do not despair, the whole cascade of events will gradually end. More precisely, by the age of 55-60, the body will “get used” to the new hormonal background, the processes of destruction and aging of tissues will slow down somewhat. In addition, a woman always has the opportunity to prolong youth and delay all of the above points with the help of a replacement hormone therapy(HRT). A gynecologist will be able to exclude contraindications and help determine the choice of the drug. It is known that HRT drugs can contribute to the development of breast cancer. Because of this side effect many women are afraid to take hormones. But in vain. With careful observation, regular mammography, examination of venous vessels, etc. the risk of complications when taking HRT is minimized. The main thing is to always love yourself (namely, love, not pity). Love is active life position It will help you live a long and healthy life.
The knee joint is prone to various injuries, since it receives the maximum load when walking. There is also a large number of diseases that contribute to this problem. Consider why the knee joints hurt, as well as ways to treat this ailment.
Causes of pain
Most often this symptom observed in people over 50 years of age. This is due to the fact that the articular tissues wear out by this age, lose their elasticity. A person can develop certain joint diseases. The most common articular pathologies are:
- Arthrosis. This disease is characterized by the gradual destruction of the knee joint, which, if not properly treated, can lead to dangerous consequences.
- Arthritis. This pathological process is caused by the development of inflammatory processes in the joint. It can occur as a result of various joint injuries or against the background of other diseases.
- Meniscopathy. This disease is an injury to the meniscus, which is sometimes irreversible. With such injuries, a person feels unbearable acute pain.
- Job disruption of cardio-vascular system. Painful sensations can be caused by improper blood circulation in knee joint.
- Periarthritis. This pathology is characterized by inflammation of the ligaments or tendons. A person feels aching pain on the inside of the knee. This usually occurs after prolonged physical exertion, especially in people who are obese.
- Arthrosis hip joint. This disease does not affect the kneecap. But with her active development pain can spread throughout lower limb including the knee.
V young age discomfort may occur after excessive physical exertion on the legs. This is not pathological process, but simply indicates severe fatigue.
The nature of the pain and possible causes
To get started necessary treatment, it is required to identify true reason pain sensations. Depending on the nature of the pain, the cause of its occurrence is identified. When diagnosing, the doctor asks the patient for complaints. The pain can be different, namely:
- Sharp pain that comes on suddenly. It may indicate a recent knee injury.
- Aching pain with an uncharacteristic crunch during flexion or extension of the lower limb. Most often, the cause of this ailment is a certain joint disease, which is chronic.
- Shooting pain. It can shoot in the knee due to the development of an inflammatory process associated with damage to the nerve channels.
- Regular discomfort. This symptom indicates muscle spasms.
- Cutting pain, manifested even after minor exertion. Such a malaise indicates damage to the patella.
- Pain after childbirth. This condition most often occurs after the transferred loads and overweight which the knees had to endure.
If the pain is pulling in nature, then this can be caused by any pathologies of the articular tissues.
It's important to know! The effectiveness of treatment directly depends on identifying the cause of pain in the knee joint!
knee pain in children
In some cases, a child of any age may complain of knee pain. A qualified specialist in pediatrics, Dr. Komarovsky, says that these symptoms in children occur by various reasons like in adults. The most dangerous conditions for a child are:
- Increased sensitivity of the shell of the knee joint. This takes place during active growth child. Shells react in this way to drops atmospheric pressure, that is, a change in the weather. This discomfort is temporary. Not considered a pathology.
- Infection in the kneecap. This is an extremely rare occurrence. The pain becomes unbearable. Even analgesics will not help get rid of it. Pathogenic microorganisms begin their active life, which brings a lot of suffering to the baby.
- Injuries. If the child has fallen or otherwise caused injury, the bruise may hurt for a long period of time.

In any case, children's complaints should be promptly responded to. The child must be shown to a specialist who will identify the exact cause, and then determine next steps aimed at treatment.
Treatment for knee pain
In order to get rid of this disease, it is necessary to carry out complex therapy. We will talk about its components in more detail later.
Medical treatment
To start using drugs, you need to consult a specialist. Which doctor should I contact for help? A rheumatologist or traumatologist can prescribe the most effective therapy. It depends on the cause of the discomfort.
Drug treatment is aimed at the use of such drugs:
- Tablets. Medicines in the form of tablets are used to relieve inflammation, normalize blood circulation and metabolic processes. For this, the following groups of drugs are used: non-steroidal anti-inflammatory drugs, glucocorticosteroids, painkillers, chondroprotectors. The following drugs are usually prescribed: Diclofenac, Ibuprofen, Meloxicam, Structum, Mydocalm and others.
- Ointment treatment. If the knees are very sore, then they take painkillers and anti-inflammatory drugs, which are also available in the form of ointments. Their advantage is that they act locally without causing side effects.
- Injections. Injectable solutions are used if the knee hurts a lot, and other treatments do not give desired result. They provide more effective action than the tablet form of drugs, since they are injected directly into the affected joint.
Important to remember! Assign medical preparations only the attending physician can!
Physiotherapy
These procedures help to alleviate the patient's condition, restore mobility to the knee joint. For these purposes, the following activities should be carried out:
- hardware procedures. These include: electrophoresis, magnetotherapy, UHF, phonophoresis. They have a warming effect, improve local blood circulation and metabolic processes, thereby contributing to the restoration of the patella.
- Massage. Such procedures give an identical effect. It also tones the muscles.
- exercise therapy. Treatment according to Bubnovsky provides for the restoration of joint mobility with the help of specially designed exercises.
Effective physiotherapy also includes the use of therapeutic mud and treatment with leeches.
An integrated approach to the treatment of knee joints will help to achieve the desired result as quickly as possible. Most important point in therapy - strictly adhere to the doctor's recommendations.

Treatment with folk remedies
deal with knee pain can help not only traditional medicine, but also folk remedies. What to do to start such an impact? To do this, you can refer to the recipes alternative medicine which will help relieve pain and eliminate inflammation.
White cabbage
Cabbage treatment involves applying a compress. This will require cabbage leaf, which should be slightly beaten off so that it starts up the juice. It is fashionable to put a little honey and salt on it. Attach to the sore knee, fix with a bandage. It is better to carry out the procedure at night. Cabbage leaf can be replaced with burdock.
Kerosene
For treatment with kerosene, it is required to take purified raw materials. It will take 200 g table salt, 100 g dry mustard. Dilute the dry ingredients with purified kerosene until a thick slurry is obtained. Rub prepared medicine massage movements into the diseased joint. This procedure should be done at night, keeping the leg warm. For best effect the knee should be wrapped in a warm scarf.
Celandine
50 g of fresh celandine grass should be placed in a 0.5 liter jar. fill it up olive oil. Close the container tightly with a lid, leave to infuse for 14 days. After the time has elapsed, the agent should be filtered, and then applied to the affected areas 4-5 times a day. This remedy has a pronounced analgesic effect.
In order to use alternative medicine, you need to consult with your doctor. It will help you choose the most effective home remedy considering the patient's condition.
Diagnosing diseases of the knee joint can be a difficult task even for an experienced doctor. Pain in the knee is not at all a “senile” symptom, as many used to think. People from young to old can face this scourge. Now we will try to understand in more detail why our knees hurt.
Main symptoms: pain, stiffness, swelling, clicks in the joint and its blockade. In almost 100% of cases, pain occurs in the knee joint and is localized on the anterior surface of the knee, much less often under the knee. Can "give" to the thigh or lower leg.
False knee pain: pain in the joint can be reflected, it can be caused by diseases of the hip joint, lumbar and sacral spine, including a herniated disc. In addition, depression can respond to knee pain, diabetes, side effect medicines or intoxication with them (taking diuretics and in the elderly can lead to gout).
_______________________________
Diagnostics and self-diagnosis
The main questions for the patient in the presence of a knee injury:
Describe how the injury happened?
Was it a blow to the knee? Which side?
Did the lower leg rotate during the injury?
Was there a click in the knee?
Was there an unsteady gait after the injury?
How quickly did the pain and swelling of the joint appear?
Have you had previous knee injuries or surgeries?
The main questions for the patient in the absence of injury:
Does the pain occur at rest or during exertion?
Do you often have to kneel, for example, during house cleaning? In this regard, could there be needles or pins in the carpet that could injure the joint?
Does it happen that the knee is blocked or you cannot bend or straighten it? Does it happen in the morning hours?
Is there joint swelling or creaking when moving?
NB! Be sure to see your doctor if you experience any of the following warning signs:
1. Increase (swelling) of the joint after injury. What matters is how quickly the joint increased - in the first hours after the injury or during the first day. Pay attention to this and be sure to tell your doctor.
2. Blockade of the joint: a sudden inability to bend or straighten the leg, the slightest movement causes acute pain.
3. Stiffness of movements in the knee joint.
4. Clicking in the joint when moving.
Of course, the diagnosis of a disease cannot be based only on the examination and questioning of the patient. The problems associated with the knee joint are no exception. Based on the combination of symptoms, the doctor will prescribe the following tests for you:
Blood test for rheumatic factor, ESR, culture;
radiography;
Bone scintigraphy;
arthroscopy;
Why do my knees hurt?
As we said above, knee pain can occur at any age. Now let's try to figure out what reasons may be behind its appearance:
0-10 years
infectious arthritis.
Juvenile rheumatoid arthritis.
Congenital dislocation of the patella.
10-20 years
Chondromalacia of the patella.
Epiphyseolysis of the head femur.
Muscle damage rear group hips.
Osteochondritis dissecans (Koenig's disease).
Osteochondropathy of the tibial tuberosity.
Tendinitis crow's feet.
20-30 years old
Bursitis and trauma.
30-50 years old
Longitudinal or transverse tear of the medial or lateral meniscus.
After 50 years
Osteoarthritis of the knee.
Ischemic necrosis of the condyles of the femur and tibia.
Paget's disease.
Bursitis of the goose foot bursa.
Gout and pseudogout.
Osteoarthritis of the hip joint - in this case we are talking about referred pain.
Now let's take a closer look at each age period. Some joint diseases can only occur in young children under the age of 10 years. An increase in muscle tone during the period of active growth can lead to functional overload of the knee joint. If a child does not play sports, then he practically does not face such a problem as knee pain. If she nevertheless made itself felt, that first of all, juvenile rheumatoid arthritis and purulent arthritis should be excluded. There may be an X-shaped or O-shaped deformity of the legs, which is not accompanied by pain. If a child goes in for sports, then when the knee joint is overloaded, pain may occur, with an X-shaped deformity, this happens approximately at the age of 4-6 years. Much more often, complaints of knee pain can occur after 10 years. And the main reason for this is chondromalacia (softening of the articular cartilage) of the patella. This disease affects both girls and boys equally. In the period up to 16 years in boys, osteochondropathy of the tibial tuberosity may make itself felt. Moreover, unpleasant symptoms in the joint can cause epiphyseolysis of the femoral head, goose foot bursitis and osteochondritis dissecans.
Speaking of sports. It's not only healthy lifestyle life, but also the zone increased risk! It is not sports that are good for health, but physical education! So jumping and running can contribute to the development of some knee problems. So at the age of 10 to 16 years, osteochondropathy of the tibial tuberosity can make itself felt. Moreover, in boys this disease occurs 3 times more often than in girls. And here one of the main medicines may be a temporary cessation of training and physiotherapy. An important role the prevention of this disease also plays: it is enough to include exercises for stretching the quadriceps femoris muscle in the training program.
Why do knees hurt in old age? There are reasons for this too. Most often, these are joint diseases, osteoarthritis, gout, pseudogout and apatite disease. In 50 percent of people over 80, the knee joints are affected. By the way, pseudogout affects the knees more often than others. Moreover, the patient may have no complaints. But with acute arthritis, which develops after 60 years, pain, enlargement and redness of the joint are possible. After 60, ischemic necrosis of the condyles of the femur and tibia can “knock”. It is characterized by the sudden onset of pain.
What other causes can lead to knee pain?
- Osteoarthritis. It affects people of middle and older age, and it is rare. Overweight women are most susceptible to it, and osteoarthritis can also be observed after a knee joint injury.
- Arthritis rheumatoid and infectious. With rheumatoid arthritis, not only the knee joint can be affected, but also others. This disease is characterized by pain in the joints, stiffness of movements, especially in the morning, increased pain at rest. Infectious arthritis affects the knee joint.
In our clinic you can always make an appointment with qualified specialists to help you beat the unpleasant symptoms associated with knee pain.
After forty-five years: for some early, for some later, the work of the female gonads begins to stop. This means not just the cessation of menstruation, stop producing female hormones. And they have very important functions, in addition to participation in fertilization, fetal growth, essential for the work of all organs and life support systems of a woman. The result of this is the development of diseases, ailments, including muscles with menopause begin to hurt. disturbed hormonal background leads to aging of the whole body, a general deterioration in well-being, weakness, fatigue, pain both during the day and at night. Muscle, joint pain is a common companion of women during menopause.
No one can escape from aging. It is so laid down by nature that the body after a fruitful life needs rest. The following factors help to bring old age closer:
- hard work;
- lack or uneven sexual life;
- many pregnancies, childbirth;
- alcoholism, smoking, drugs;
- unhealthy diet, lack of daily routine, lack of sleep;
- a lot of stress;
- chronic diseases.

On occurrence discomfort in muscles and joints, mental breakdowns in a woman with menopause, insomnia, and hot flashes can also be affected.
Muscle pain
Women whose lives are spent with heavy loads on their legs, standing, carrying heavy loads, suffer more than others from diseases of the skeleton and muscles with the onset of aging. Muscle fibers, tendons, blood vessels suffer greatly from a lack of hormones, become lethargic, not elastic, with dystrophic lesions. Vessels poorly pass blood with oxygen and substances for the successful functioning of organs, cholesterol plaques also interfere with it.
Also, muscle pain during menopause can begin after increased movement or labor, if before that the woman was not physically active and usually led a passive lifestyle.
Muscle pain has scientific name- myalgia. As with body tension, and with inactivity, pain can appear the same way. One ligament or several can get sick, since the muscular corset is arranged with a complex interweaving and interaction of ligaments, tendons, muscles. Muscle pain can be due to the following reasons:
- due to sprain;
- due to inadequate, sharp loads on the ligaments;
- due to hypothermia of the body;
- due to medication high pressure, statins;
- due to malnutrition, lack of vitamins in the body;
- from strong feelings, stress.

Myalgia may occur in following parts limbs:
- shin;
- pelvic girdle;
- hip;
- foot.
The occurrence of soreness can begin immediately in all parts of the leg. Pain in the muscles during menopause appear due to spasmodic phenomena in the nerve endings of the spine and joints.
Pain can be characterized by different types:
- chronic;
- sharp;
- sharp;
- aching for a long time;
- tingling.
An important fact is that you can confuse muscle pain with joint or bone pain, which can be caused by too long walking or uncomfortable shoes.
Constant manifestations of soreness should force a woman to consult a doctor who will conduct an examination and tests, and prescribe treatment. Such health problems are dealt with by a traumatologist, phlebologist, angiosurgeon, rheumatologist.

Anatomical pain
Painful sensations in the legs do not always indicate a disease: the ligaments can hurt from the consequences of incorrect postures when working, standing or sitting for a long time.
With immobility, stagnation occurs in the blood vessels, which do not allow blood to circulate normally. Arises oxygen starvation, toxins accumulate in the shins, knees, feet, thighs, provoking the occurrence of stabbing, aching, dull pains. It may seem that the whole body hurts. Carrying out a warm-up, exercises will help the blood flow to return to normal, and the symptoms will pass.
Obesity
Excess weight is also bad for the condition of the legs. Since during menopause, due to a hormonal deficiency, the body begins to build up fat in order to produce estrogen from it, many women suffer from pain in both the joints and the muscles of the legs.

Accompany muscle pain in women after a stroke, heart attack, with edema and aching pains. It gives reason for the appointment diet food women, to bring the weight back to normal, relieve the load from the limbs.
convulsions
Cramps are the occurrence of involuntary muscle contractions, manifested both in one bundle and in several at once.
Most often, cramps are present in the legs, calf muscles, after prolonged exertion on the legs. This is very painful sensation, and is not uncommon in menopausal women. To overcome cramps, do the following manipulations:
- relax the muscle by changing the position of the leg;
- rub the muscle with your hands;
- apply cold or stand in a cold place;
- prick the muscle with a sharp object;
- lift your toes up as high as you can towards your shin.
Myalgia in vascular diseases
There are two types of diseases in which pain in the muscles of the legs is possible: atherosclerosis and thrombophlebitis. After a number of reasons, the blood supply to the limbs is disturbed, these diseases occur. Here, massage is indispensable: the treatment is long and complex, it does not tolerate delay.
Atherosclerosis
If a woman's muscle pain increases after walking, this may be a sign of the development of obliterating atherosclerosis of the arteries.
In addition to the symptom of pain when walking, with atherosclerosis, there are signs such as fatigue and muscle weakness. With these manifestations, it is necessary to go to the doctor, because without treatment of the disease, vasogenic intermittent claudication occurs. Despite the fact that atherosclerosis obliterans is more common in the male population, women also suffer from it, especially those who smoke and are dependent on alcohol. Women who do not suffer from chemical addictions are twice as likely to get this disease.
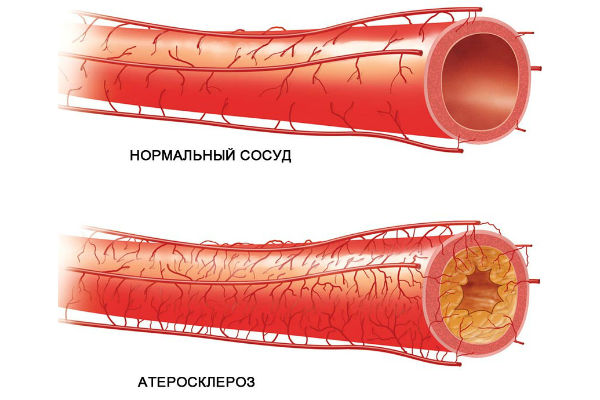
Cholesterol blockage of veins and arteries leads to insufficient blood supply to the legs, stenosis, which is fraught with gangrene and limb amputation without treatment. The development of the disease proceeds very quickly, the following parts of the limbs begin to hurt:
- buttocks with an affected aorta;
- hips - when clogging the artery of the thigh;
- feet - with blockage of the popliteal arteries;
- calf muscles - due to common blockages in the deep veins, arteries of these muscles.
There are a number of causes of obliterating atherosclerosis of vessels:
- cardiac ischemia;
- hypertension;
- vasculitis;
- systemic HF;
- herpes;
- high cholesterol;
- diabetes;
- bleeding disorders;
- violation of fat metabolism;
- aortic aneurysm in the peritoneal region;
- lack of movement
- chemical dependencies;
- injuries, frostbite of the legs;
- power overloads.
Treatment for this disease is prescribed by the doctor after a thorough diagnosis, taking into account concomitant diseases.
A healthy lifestyle is recommended, an anti-cholesterol diet, replacing meat in the diet with fish, drugs that normalize vascular health, vitamin complex. Obliterating atherosclerosis is accompanied by paresthesia (numbness, goosebumps), pain not only during movement, but also at rest.
Thrombophlebitis
Thrombophlebitis in medicine is considered an insidious, unpredictable disease. This inflammatory disease the walls of the veins, narrowing the lumen of the vessels. Venous blood cannot pass freely, stagnates, this leads to blood clots. There is thrombophlebitis not only of the legs, but of the arms, cervical and chest. It happens that inflammation of the walls of the veins is observed without thrombus formation, then it is phlebitis.
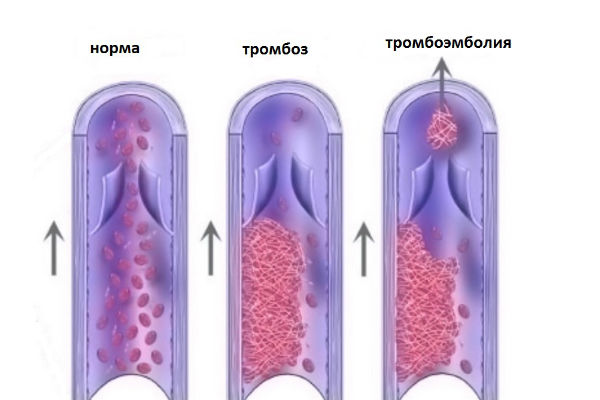
The disease is initially asymptomatic, the pain comes when a large area of the vessels is inflamed. The formed thrombus at one tragic moment breaks off, rises through the vein towards the heart and beyond. It is impossible to determine its direction, in which organ it will fall at the end of the voyage. If it reaches the blood vessels in respiratory tract, this is fraught with arterial embolism, that is, blockage.
This will cause instant death.
Signs of thrombophlebitis
Many people go to the doctors when the disease has already severely affected the vessels. Symptoms of the onset of inflammation of the veins are as follows:
- legs begin to swell;
- pain in the calf muscles;
- burning and heaviness of the legs;
- the skin of the legs turns red.
If you do not go to the hospital in time, the swelling increases, the skin at the site of the thrombus turns blue and then blackens. Places of formation of blood clots - thigh, lower leg, ankle.
Who is at risk for thrombophlebitis?
- having a sedentary job;
- suffering from varicose veins;
- suffering from severe blood clotting;
- obese;
- with a sedentary lifestyle in menopause.

Treatment is complex, depending on the severity of the disease and related problems. There are many medications to relieve acute symptoms, vascular obstruction, assigned personally to the patient's condition, various physiotherapy, in difficult cases an operation is performed to correct the veins or the use of laser obliteration to remove blood clots. Charging and movement are vital for thrombophlebitis.
Osteochondrosis lumbar
With menopause, worn out by work, in the wrong way of life, the joints and vertebrae begin to transform, wear out. Inflamed nerve roots intervertebral discs, squeezed, the pain goes to the legs or longitudinal muscles near the spine. From pain, the back muscles reduce, they become like a stone.
In addition to the lumbar, osteochondrosis is thoracic, cervical, then the pain is given to the muscles thoracic or neck, hands.
Women who take care of their health have strong skeletal muscles, because they go in for sports, they suffer from this disease less often than others. In order for osteochondrosis to be defeated, you need to do exercise to strengthen the muscles of the corset, visit a massage therapist, physiotherapy prescribed by a doctor, treatment with anti-inflammatory drugs, chondroprotectors.

sciatica and lumbago
Sciatica, in which the sciatic nerve becomes inflamed, has the following causes:
- diabetes;
- injury;
- arthritis;
- gout;
- osteophytes (growths on the vertebrae);
- displacement of the vertebrae;
- erasure of intervertebral discs;
- hypothermia;
- strong load on the spine.
The slightest reflex movements of the body: walking, coughing, sneezing, laughing, can cause unbearable shooting pain in the lumbar region.
With lumbago, a displacement or change in the shape of the vertebrae occurs due to heavy loads. Around each vertebrae there are many nerves, when injured, they become inflamed, causing pain in the surrounding ligaments and muscles. Lumbago is manifested by severe shooting, dagger-like pain, sometimes shooting in the thigh, buttock, lower leg to the heel and cramps in the muscles of the buttocks and thighs.
Sciatica and lumbago usually occur in pairs, leading to impaired muscular and cutaneous circulation, and developing leg motor neuropathy, muscle weakness, and lameness. The lumbago occurs unexpectedly while tilting, turning, trying to sit down. Muscle pains of this nature are frequent during menopause, as the muscles become sluggish, weak, it is difficult for them to hold the spine if the weight is also increased.

Inflammation is relieved with anti-inflammatory drugs in injections or tablets, the use of ointments, physiotherapy.
Gonarthrosis of the knee joints
Gonarthrosis (or osteoarthritis) occurs with degenerative-dystrophic damage to the knee joint, in which cartilage is destroyed, the joint is deformed and gradually immobilized.
Osteoarthritis affects mainly women during menopause, men - less often.
Climbing stairs or descending, squatting cause severe pain in the joint and in the tissues around it. The tissues swell, are painful to the touch, during periods of exacerbation, severe spasms of the lateral ligaments from the knee to the femoral joint are possible. Usually the disease is not cured, with the help of drugs and physiotherapy, only inhibition of the development of the disease is possible. In medicine, the replacement of a joint with an artificial one is practiced.
Osteoarthritis of the big toe
Toe disease causes deformation and growth of the joints of the toe due to the fact that calcium salts are deposited on them.
Such a disease does not occur until menopause, when female hormones do not allow the formation of uric acid crystals in the joints. Causes of damage to the joints of the fingers:
- joint injuries due to wearing heels;
- Signs of the disease:
- dull pain while walking;
- it is difficult and painful to bend a finger;
- fingers crackle;
- joints swollen and reddened;
- fingers are bent, can cross one relative to the other.
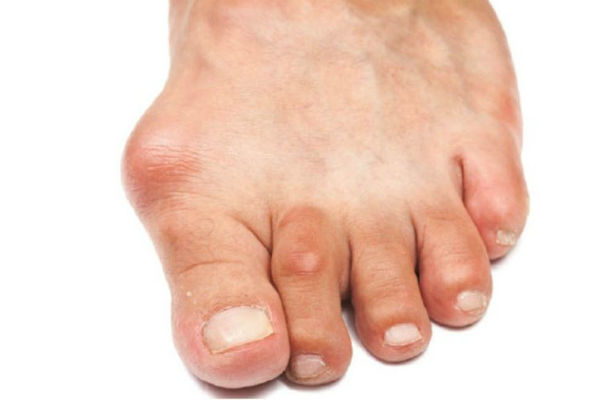
Pain in the joint and in the tissues around increases after walking. The treatment is identical to that of arthrosis.
Polyneuropathy
Polyneuropathy begins when the nerve endings in the limbs are affected, resulting in loss of tactile sensations, difficulty with the movement of the fingers. Strong pain and cramps after movement are signs of illness. Polyneuropathy in menopause occurs for the following reasons:
- toxic poisoning;
- diabetes;
- as a side effect of certain drugs;
- impaired immunity, which is often present during menopause;
- metabolic disorders, often with menopause.

The disease of diabetic polyneuropathy has become very widespread, leading to the fact that muscles atrophy and trophic ulcers appear. Illness requires heightened attention and treatment as early as possible, so as not to paralyze the limbs, and ultimately - breathing.
The treatment of the disease is complex, it is prescribed after a complete diagnosis of the body.
Muscle pain in hypothyroidism and hyperthyroidism
Arise: the first - due to a lack of production of hormones by the thyroid gland, the second - due to their excess. These thyroid diseases affect the muscles of the skeleton. Leukocytes mistakenly attack muscle cells and nearby blood vessels, or abnormal substances begin to accumulate in the ligaments, weakening and causing them to become sore. Symptoms of hypothyroidism are as follows:
- weakness, pain, cramps, poor muscle mobility;
- joint pain, difficulty moving;
- inflammatory processes in the tendons of the extremities;
- the occurrence of carpal tunnel syndrome with pain, tingling, weakness, numbness of the hands, fingers, or forearms;
- the occurrence of tunnel syndrome of the foot, similar to the carpal.

With the disease, the muscles around the joints swell or a tumor develops that presses on the nerve endings.
Hyperthyroidism gives a feeling of weakness and muscle fatigue, that is, muscle atrophy. Complaints in hyperthyroidism are the following manifestations:
- difficult to climb;
- it is difficult to hold or even take something with your hand;
- difficulty keeping arms up;
- seventy percent of hyperthyroid patients have damage to the muscles of the pelvis and thighs.
It is not the symptoms that need to be treated, but the thyroid gland in order to normalize the hormonal background; and with menopause, thyroid damage is caused by hormonal failure.
Therefore, treatment should be competent and comprehensive.
flat feet
With this problem, the entire foot touches the floor, the raised central part of it falls, cannot cushion when moving. Such a problem occurs after the weakening of the muscular-ligamentous mechanism on the foot, the consequences of flat feet are manifested as follows:
- gait becomes heavy; such feet hurt from movement, and with developed flat feet - from prolonged standing;
- with the loss of depreciation of the feet, walking and running lead to pain in the joints, spine and skull. The depreciation function goes to the spine, but it is not adapted to this, it gets injured and starts to hurt due to pinched nerves near worn discs and vertebrae;
- grown bones in thumbs legs - a consequence of flat feet, blood circulation in the legs worsens, the ankles swell and ache;
- a change in the foot leads to deformations of the joints of the knees, hips, pelvic joints;
- gait becomes ugly, heavy, tired.

The disease can be treated with special physical education, massage, wearing insoles, provided that the treatment is on time, without starting the process of changing the foot.
Myositis
Myositis is an inflammation of muscle tissues for various reasons.
If you do not go to the doctor, gradually the pain intensifies, becomes unbearable, the end result of this is atrophy of the ligaments.
The disease occurs for the following reasons:
The first symptom of myositis is the ongoing muscle pain during movement and immobility, the chronic course of the disease reveals the appearance of nodules in the tissues, muscle weakness, fatigue. disease on early stages successfully treated with drugs, rest.

fibromyalgia
Since the balance of many hormones is disturbed during menopause, this can cause the manifestation of this disease.
Fibromyalgia is an extremely increased threshold of sensitivity to pain, when the pain is felt many times stronger and longer than usual, a weak, tired state is constant, depression.
The etiology is poorly understood, but doctors suggest a brain disorder associated with the processing of body signals about painful sensations. The causes of the disease are physical and mental injuries:
- body injury;
- viral infections;
- childbirth;
- operation;
- divorce;
- unfavorable home environment;
- loss of loved ones;
- insomnia;
- the presence of cold and dampness;
- rheumatic lesions.

The treatment of the disease is symptomatic, relieving pain, homemade food without semi-finished products and monosodium glutamate, the exclusion of nightshade vegetables, and the use of alkaline foods help.
Examination for muscle pain
The diagnosis can be made after the following activities:
- general blood test;
- hormonal analysis;
- x-ray or ultrasound of the joints, spine;
- carrying out osteodensitometry to determine the density of the tissues of the skeleton.
A competent doctor will not prescribe treatment without conducting a comprehensive examination.
How to treat muscle pain?
Before treatment, it is necessary to undergo a comprehensive examination of the body in order to find real reason unpleasant sensations. Myalgia is treated with analgesics, antispasmodics, non-steroidal anti-inflammatory drugs:
- Nimesil;
- Finalgon;
- Fastum;
- Nurofen;
- Ketonal;
- Voltaren;
- Spasmalgon.

Against muscle spasms, Mydocalm is used, but together with Omeprazole, so as not to harm the stomach. Any drugs are prescribed by a doctor; self-medication is unsafe for health. Visit an orthopedist and rheumatologist to identify possible non-hormonal problems of muscle pain. Also, during menopause, regular examination by a gynecologist is important so that the appearance possible diseases detect at an early stage, successfully prevent their development.
The menopause period requires the adoption of female hormones after hormonal tests, the doctor prescribes drugs, self-medication can not only help, but aggravate disease state women.
Estrogen forms:
- Klimonorm;
- Divina;
- Femoston.
Phytoestorogens are popular in modern medicine, gently act, relieve many of the unpleasant symptoms of menopause.
Vitamins for menopause
In order to maintain health for a long time during menopause, a woman should carefully monitor her condition, take healthy food with trace elements in order to protect the musculoskeletal corset from the above problems, and have enough time to rest.
After the lady consults with the doctor, he will prescribe the following vitamins that are useful for menopause:
- vitamin A, antioxidant;
- vitamin C;
- vitamin E;
- vitamins B1, B6, B12;
- vitamin D3.

The use of these vitamins in menopause is useful to alleviate the general condition, to increase protective forces, and to normalize the overall metabolism in the body. During treatment with Menopace, Remens, Femoston, the body is filled with microelements, helping to work immune system, strengthening the skeleton of the skeleton. Treatment should occur at the onset of symptoms, rather than waiting for the woman to be in a wheelchair.
Preventive measures for muscle pain
- Physical exercises begin with a warm-up.
- Muscle stretching exercises before and after exercise.
- Eat enough clean water before, during and after exercise.
- Eat healthy food with most vegetables and fruits in your diet.
- Saturate the diet with calcium, take Calcium D3 Nycomed.
- Therapeutic exercises to strengthen ligaments and muscles.
- Massage.

During menopause, you need to constantly take care of your health in order to push back aging, maintain tone muscle corset and skin, besides the movement helps to improve mood, the work of the cardiovascular system and the musculoskeletal framework.
Alternative medicine for muscle and joint pain
Our ancestors a century ago used the gifts of nature to fight body ailments:
- Ten drops of laurel oil + one liter warm water- Wet a cloth with the solution, apply to the affected part of the body.
- Tie a fresh cabbage leaf to the swollen area overnight. Draws out swelling, relieves pain.
- Take a glass vessel made of dark glass, fill it with dandelion flowers, fill it to the top with cologne, insist for a month in the dark. Rub sore spots with osteoarthritis. Dandelion is considered a natural chondroprotector.
- Baths of one liter of warm water and one large spoon sea salt with swelling, pain in the joints.
- Inflammation sciatic nerve treated with infusion of lilac flowers or red pepper in alcohol.
- One small spoonful of natural apple cider vinegar+ 200 ml of water helps with muscle and joint pain. Take 14 days twice a day before meals.
- Contrasting dousing of legs with cold and warm water alternately used for venous thrombosis.
Remember, dear ladies, that any treatment, pain relief, swelling of muscles, joints must first be discussed with your doctor, never exercise self-treatment without a diagnosis. Take care of your health and be happy!
Useful and interesting video on this topic:
